STD's and HPV - St. Luke's Roosevelt Hospital Center, Department
advertisement
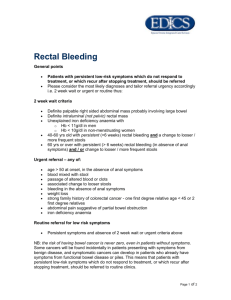
STDs and HPV George Dreszer, MD. Colon and Rectal Conference 10/19/05 St. Luke’s Roosevelt Chlamydia Infection Chlamydia infection is now the most common bacterial STIs in the US 4-8 Million new cases occurring each year Most Frequently seen in the Homosexual Population Particularly High incidence among AfricanAmericans Lymphogranuloma Venereum LGV is a suppurative STI caused by C. Trachomatis Historically Low incidence in US Incidence is increasing as a complication in patients with AIDS Early symptoms are referable to GU tract May lead to PID and infertility in Women Rectovaginal Fistual has been described as a complication LGV Lesion initially appears as a herpetiform vesicle on the genital or anal area Complaints are typically of Dysuria, Pyuria and Mucopurulent Discharge Lower Abdominal Pain may be present Unilateral lympadenopathy and systemic signs appear 1-4 weeks following initial lesion The nodes enlarge, from a mass and drain May start in the rectum as proctitis with symptoms of rectal discharge, bleeding and tenesmus Anal fissures are not uncommon, and rectovaginal or perianal fistulas may develop Intestinal Obstruction may occur late Frei Test-- Intradermal test similar to tuburculin test Treatment TCN, Erythromycin and DS Bactrim x 21 Days Rectal Stenosis may require a resective procedure or diversion Gonorrhea Bacterial Infection caused by Niesseria gonorrhoeae Humans are the only known reservoir Disease affects mucous membranes of the urethra, cervix, rectum and oropharynx Incidence is 40x higher in in black population as compared to the white population Incidence is about 400,000 cases which are reported to CDC per Year Symptoms: Discharge from Penis or Vagina Can cause PID, ectopic pregnancy and infertility Gonorrheal Proctitis Usually seen in the Homosexual popution In women, this condition can be caused by spread from the genital tract To confirm the presence of the bacterium by culture, rectal swabs are innoculated on Thayer-Martin Agar Only the lower rectum is involved Symptoms occur 5-7 days after exposure and include: Pruritis, Rectal Bleeding, Diarrhea and disseminated disease (septicemia, pericarditis, endocarditis, meningitis, perihepatitis, and gonoccocal arthritis) Proctosigmoidoscopy reveals edematous, friable mucosa with occasional areas of ulceration, however, in many individuals no identifiable lesions will be noted Treatment: Single dose of Ceftriaxone IM, or One dose PO Fluoroquinolones Ceftrixone is preferable because it also covers incubating Syphilis Herpes Simplex Proctitis HSV Proctitis is the most common non-gonoccocal proctitis in sexually active male homosexual Klausner and colleagues reported a 16% incidence among homosexual men HSV-2 is the most common cause of HSV Proctitis, but HSV-1 can also produce HSV Proctitis Herpes infections in AIDS patients may develop an ulcerative proctitis which remains confined to the rectum Symptoms include: Tenesmus, anorectal pain, constipation, and perirectal ulceration Anorectal incontinence may present during the acute phase, with resolution after treatment of the HSV Infection Perianal area reveals typical herpetic vesicles, pustules and ulcerations (Digital exam and anoscopy are very painful) Herpes Continued Sigmoidoscopy reveals an acute proctitis with edematous, ulcerated, and friable mucosa The infection is usually confined to the rectum and in immunocompetant individuals rarely extends beyond 15 CM Diagnosis is established by Immunoassay of the Ab to the virus, or by Immunofluorescent Staining Treatment: Acyclovir PO, or Acyclovir IV in AIDS patients Suppressive therapy is recommended to decrease relapses Syphilis (Lues) Caused by the Spirochete Treponema Pallidum Organism enters the skin or mucous membrane, producing a Chancre approximately 3 weeks following the infection (Primary Stage) Chancre is a single painless open sore In the homosexual male population the chancre is usually situated at the anal margin or in the canal (these lesions can be painful) Symptoms include tenesmus, difficulty with defecation, and discharge Sometimes confused with anal fissure, but the presence of lymphadenopathy should alert the examiner Diagnosis clasically has been made by identification of T. Pallidum on Dark-Field Microscopy However, since the absence of a positive test does not rule out the diagnosis of Syphilis, it is preferable to treat patients with suspicious clinical lesions and wait for results of Serologic evaluation It is important to remember that serologic tests for Syphilis do not yield positive results until the primary chancre has been present for several weeks Treatment: Benzathine PCN, or TCN in PCN allergic patients. Erythromycin can also be used Human Papilloma Virus Condyloma Acuminata represents the most common STI in the practice of most surgeons Caused by a DNA virus that is a member of the Papovirus group Most Commonly seen in Homosexual Male population 19 % of patients with HIV have been found to have anal condyloma It is recommended that all patients with anal condyloma undergo HIV testing because of this high correlation HPV Symptoms include discharge, pruritis, difficulty with defecation, anal pain, tenesmus, foul odor, and rectal bleeding Patients have often received some form of topical treatment which has failed Warts are usually, small, discrete, elevated pink to grey vegetative excrescences HPV Histology Hyperplastic Epithelial Growth with irregular acanthosis and marked Hyperkeratosis Treatment of Anal Condyloma American Society of Colon and Rectal Surgeon Recommendations “When Condylomata are limited to the peri-anal skin, treatment with topical medications, local destruction, or harvesting and immunotherapy can be administered in an outpatient setting. Patients with extensive perianal or anal canal condylomata, or those patients with associated genital condylomata may require inpatient care.” Treatment Modalities 1. Podophyllin- cytotoxic chemical agent very toxic to normal skin. Can only be used on external warts. Dysplasia has been reported with prolonged use. Multiple treatments are usually required Other caustic agents are available Eg. Bichloracetic Acid Immunotherapy 2. A Vaccine is created and the patient is vaccinated with six consecutive weekly injections Study of 200 patients showed excellent results in 84%, Fair results in 11% and no results in 5% Another study by Eftaiha et al reported successful eradication in 94% of patients Recurrence rate at 13 Months was 4.6% Immunomodulators (Imiquimod/Aldara) 3. Imidazoquinolines- a new class of immune-response modulators Mechanism of action unknown, but thought to play a role in cytokine-induced activation of the immune system Application 3/week qhs x 16weeks Topical Cytostatics 4. Cheotherapeutic agents such as 5-FU, Thiotepa and Bleomycin Bleomycin is given as an intra-lesional injection q2-3weeks 70% success rate reported Cryotherapy and Laser Therapy 5. Cryotherapy- topical application of Liquid Nitrogen commonly used by dermatologists for the treatment of conventional warts 6. Laser Therapy- work through thermonecrosis Success rate from 88-95% Higher rate of recurrence seen than electrocoagulation No difference in healing time, pain or scarring reported Fulgaration/Electrocoagulation 7. Fulgaration with excision of a portion to send to pathology Gold Standard Very Painful if done too deeply, should not be into the dermis or fat Risk of stricture formation if a large area is to be treated Less than 50% have full resolution after one treatment Anal Intraepithelial Neoplasia Lesion thought to be precursor to Anal Squamous Cell Carcinoma Seen most frequently in patients with HIV/AIDS According to Cleveland Clinic Florida Group, the incidence of AIN in patients with anal condylomata is as high as 31% Incidence in HIV(+) group was 51% vs. 17% in HIV(-) population Anal Condylomata Summary External Condylomata without evidence of Internal Warts can usually be effectively treated by chemical means If the response is unsatisfactory, physical destruction by electrocoagulation is the preferred approach Obtaining tissue for pathologic confirmation, especially with respect to premalignant or malignant change is a a prudent philosophy