chapter four the human body: from food to fuel
advertisement

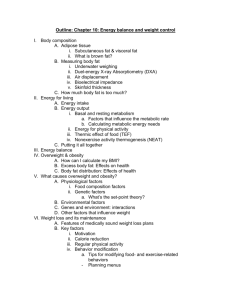
Energy Balance and Weight Management Good health, including weight management, requires an equilibrium: Energy intake must equal energy output Good health, including weight management, requires an equilibrium: Energy intake must equal energy output If energy intake exceeds energy output (“positive energy balance”) the extra calories will be stored as fat - you will gain weight. Good health, including weight management, requires an equilibrium: Energy intake must equal energy output If energy intake exceeds energy output (“positive energy balance”) the extra calories will be stored as fat - you will gain weight. If energy output exceeds energy intake (“negative energy balance”) your body will used stored fat and glycogen (and, if necessary, protein) to produce energy you will lose weight Energy Balance: We’ve already discussed sources of energy intake: Energy Balance: We’ve also discussed some types of energy output: Exercise: Cellular processes: Heat production: Energy Balance: Intake is regulated by both internal and external cues: Internal cues: Your brain is constantly monitoring the energy needs of your body and whether or not these needs are being met. This has three components: Hunger - prompts eating Satiation - signals to stop eating Satiety - keeps you from starting to eat again Energy Balance: Intake is regulated by both internal and external cues: External cues: Your brain creates a desire to eat a specific food or type of food, called appetite, which may or may not be directly related to meeting the energy needs of the body. Components: Mood Stress Social situations Time of day or Time of year Energy Balance: Food intake These internal and external cues work together in a number of ways to influence food (and thus energy) intake: 1. Chewing, salivation, and swallowing send signals to the brain which decrease hunger and appetite Energy Balance: Food intake These internal and external cues work together in a number of ways to influence food (and thus energy) intake: 1. Chewing, salivation, and swallowing send signals to the brain which decrease hunger and appetite 2. Stretching of the stomach (and possibly the intestine) sends signals to the brain which decrease hunger and appetite. Energy Balance: Food intake These internal and external cues work together in a number of ways to influence food (and thus energy) intake: 1. Chewing, salivation, and swallowing send signals to the brain which decrease hunger and appetite 2. Stretching of the stomach (and possibly the intestine) sends signals to the brain which decrease hunger and appetite. 3. More than fifty different chemicals influence how the brain processes feelings of hunger, appetite, satiation, and satiety Energy Balance: Food intake (Chemicals which influence how the brain processes feelings of hunger, appetite, satiation, and satiety) 3a. Neuropeptide Y is a protein produced in the brain which stimulates hunger and appetite and thus increases food intake Energy Balance: Food intake (Chemicals which influence how the brain processes feelings of hunger, appetite, satiation, and satiety) (Neuropeptide Y) 3b. Ghrelin is a hormone produced in the stomach which stimulates hunger and appetite. It rises early in a meal, then falls quickly after the meal is over. It also slows down the body’s burning of fat. Energy Balance: Food intake (Chemicals which influence how the brain processes feelings of hunger, appetite, satiation, and satiety) (Neuropeptide Y; Ghrelin) 3c. Leptin is a hormone produced by fat cells which stimulates satiety, thus decreasing food intake. It is produced in direct proportion to the amount of stored fat, but over time its production drops even of fat is unchanged. Energy Balance: Food intake (Chemicals which influence how the brain processes feelings of hunger, appetite, satiation, and satiety) (Neuropeptide Y; Ghrelin; Leptin) 3d. Insulin is a hormone produced by the pancreatic islets which stimulates satiation and satiety, thus decreasing food intake. Energy Balance: Food intake (Chemicals which influence how the brain processes feelings of hunger, appetite, satiation, and satiety) (Neuropeptide Y; Ghrelin; Leptin; Insulin) 3e. Cholecystokinin is a hormone produced by the small intestine which stiulates satiation and satiety, thus decreasing food intake Energy Balance: Food intake These internal and external cues work together in a number of ways to influence food (and thus energy) intake: (1. Chewing, salivation, and swallowing) (2. Stretching of the stomach) (3. Chemicals) 4. The composition of your diet will also affect food intake: Proteins promote satiety the most Carbohydrates promote satiety moderately Lipids promote satiety the least Diets high in fiber promote satiety Solids promote satiety more than liquids Energy Balance: Food intake These internal and external cues work together in a number of ways to influence food (and thus energy) intake: (1. (2. (3. (4. Chewing, salivation, and swallowing) Stretching of the stomach) Chemicals) Composition of the diet) 5. The flavor, texture, color, and temperature of food can influence appetite Energy Balance: Food intake These internal and external cues work together in a number of ways to influence food (and thus energy) intake: (1. (2. (3. (4. (5. Chewing, salivation, and swallowing) Stretching of the stomach) Chemicals) Composition of the diet) Flavor, texture, color, temperature) 6. The smell of food has a strong effect (either positive or negative) on hunger and appetite Energy Balance: Food intake Many cultural & societal factors also influence food intake: + Your mom or your coach: “Eat, Eat!” Social situations with lots of people Large serving sizes Advertising Dim lighting/romance Distraction from loneliness, anger, boredom - Awareness of what you are eating Fear of gaining weight (anorexia) Energy Balance: Food intake Obviously, the “cues” which stimulate or inhibit hunger, appetite, satiation, and/or satiety are very complex and they all interact in multiple ways. Nutritionists often talk about this as “contol by committee” – no single factor can be identified, but working together these factors effectively stimulate or inhibit a) The need to eat (hunger) b) The desire to eat (appetite) c) The feeling of “I’m full so I’ll stop now” (satiation) d) The feeling of “It’s not time to eat again yet” (satiety) The other side of the energy balance equilibrium, of course, is Energy Output. Just as there are many ways you gain energy through food intake, there are many ways you use energy. Your textbook lists three components of energy expenditure but Physiologists consider heat production to be separate from other types of “resting” energy expenditures Energy Balance: Energy Output 1. Ingesting, digesting, absorbing, and metabolizing the food you eat requires a significant amount of energy. This is called the Thermic Effect of Food. At rest, this is 5% to 10% of total expenditure. It peaks one or two hours after eating and lasts for four to five hours. Energy Balance: Energy Output 2. By far, the largest energy expenditure is the Resting Energy Expenditure (REE) needed for the basic body functions to stay alive such as breathing, circulating blood, nerve function, moving molecules into and out of cells, maintaining body temperature, bone and muscle growth, forming urine, fighting infections, reproducing, etc. At rest, this is 60% to 75% of total energy. It is also known as the Basal Metabolic Rate (BMR) Energy Balance: Energy Output Resting Energy Expenditure or Basal Metabolic Rate are defined as the amount of energy (kcals) used for these functions over a full day. When calculated per hour it is the Resting Metabolic Rate (RMR). Energy Balance: Energy Output Resting Energy Expenditure or Basal Metabolic Rate are defined as the amount of energy (kcals) used for these functions over a full day. When calculated per hour it is the Resting Metabolic Rate (RMR). Thus, if you maintained a Resting Metabolic Rate of 60 kcal/hour then your Resting Energy Expenditure would be (60 kcal/hour) x (24 hours) = 1,440 kcal/day Energy Balance: Energy Output Resting Energy Expenditure primarily depends on the lean body mass – the total mass of everything that isn’t fat. Thus, a muscular person will have a higher RMR and REE than a nonmuscular person. Energy Balance: Energy Output Resting Energy Expenditure primarily depends on the lean body mass – the total mass of everything that isn’t fat. Thus, a muscular person will have a higher RMR and REE than a nonmuscular person. In general, men have more lean body mass than women, but in both sexes the lean body mass (and thus both RMR and REE) decline with age. Energy Balance: Energy Output Resting Metabolic Rate can be estimated by multiplying the weight in kilograms by 1 kcal/kg for men and 0.9 kcal/kg for women and Resting Energy Expenditure can then be calculated by multiplying this by 24 hours. Energy Balance: Energy Output However: many other factors can change resting metabolic rate and resting energy expenditure. Energy Balance: Energy Output 3. The most variable energy expenditure is the Energy Expenditure of Physical Activity. For most people, this is 15% to 30% of total expenditure, but for extremely active people it can be as much as 50% or 60% of total expenditure. Energy Balance: Energy Output 3. The most variable energy expenditure is the Energy Expenditure of Physical Activity. Muscle contraction, whether it is used to walk around during a normal schoolday, climb up Sugarloaf, or run the Twin Cities Marathon, requires a very large amount of energy. Energy Balance: Energy Output Energy Expenditure of Physical Activity: For example: An 80 kg (175 pound) person uses approximately: 95 kcal per hour when sleeping 140 kcal per hour when reading or studying 275 kcal per hour when walking at a moderate pace 550 kcal per hour when jogging 650 kcal per hour when swimming laps 1,300 kcal per hour when running at top speed Energy Balance: Energy Output Energy Balance: Energy Output While it can be useful to separately determine the Thermic Effect of Food, the Resting Energy Expenditure, and the Energy Expenditure of Physical Activity, most often it is more important to know the sum of all three, the Total Energy Expenditure (TEE) Energy Balance: Remember: The total amount of energy your body expends each day must equal the number of calories consumed in food, so you can calculate an Estimated Energy Requirement – the amount of energy intake needed each day to maintain energy balance in a healthy individual of normal weight. Total Energy Expenditure = Estimated Energy Requirements. Energy Balance: Energy Intake but there are many online calculators into which you can enter these values and determine your EER. For most people, this is between 2,000 and 2,800 kcal/day Body Composition: Note that both your Estimated Energy Requirements (calories consumed) and your Estimated Energy Expenditure (calories used) are strongly influenced by your body weight. Body Composition: Note that both your Estimated Energy Requirements (calories consumed) and your Estimated Energy Expenditure (calories used) are strongly influenced by your body weight. However: not all “weight” is equal. Muscles, bones, blood, and solid organs are relatively heavy Body Composition: Note that both your Estimated Energy Requirements (calories consumed) and your Estimated Energy Expenditure (calories used) are strongly influenced by your body weight. However: not all “weight” is equal. Muscles, bones, blood, and solid organs are relatively heavy Fat and other connective tissues are relatively light Body Composition: The commonly accepted method for assessing your body composition is the Body Mass Index (BMI) which is the ratio of your weight to the square of your height. weight (kg) BMI = height (m2) or weight (lbs) x 704.5 2 height (in ) This correlates well with the amount of lean mass and fat you have, and with your risks for developing a number of diseases. Body Composition: Normal: BMI between 18.5 and 24.9 Body Composition: Underweight: BMI below 18.5 Normal: BMI between 18.5 and 24.9 Body Composition: Underweight: BMI below 18.5 Normal: BMI between 18.5 and 24.9 Overweight: BMI between 25 and 29.9 Body Composition: Underweight: BMI below 18.5 Normal: BMI between 18.5 and 24.9 Overweight: BMI between 25 and 29.9 Obese: BMI above 30 Body Composition: Excess body fat, measured as a high Body Mass Index, is a well established indicator of increased risk for diseases such as diabetes, stroke, heart disease, and many cancers. Body Composition: Excess body fat, measured as a high Body Mass Index, is a well established indicator of increased risk for diseases such as diabetes, stroke, heart disease, and many cancers. However, BMI is just an estimate for most adults: it’s less accurate for predicting risk in children, the elderly, highly muscular individuals, and well-trained athletes. In some instances, therefore, more direct measurements of the amount of fat are necessary. Body Composition: (More direct measurements of fat are often necessary) The most accurate way to measure fat is a technique called “dual energy X-ray absorptiometry”. As its name implies, this requires a specific instrument which is not available outside of a hospital setting and is very expensive. Body Composition: (More direct measurements of fat are often necessary) Less expensive methods include Underwater or hydrostatic weighing Air displacement in a contained space Both take advantage of the fact that fat is much less dense than bone, muscle, etc. so it displaces less water or air per kilogram or per pound. Body Composition: (More direct measurements of fat are often necessary) Less expensive methods include Bioelectrical impedence, which takes advantage of the fact that fat conducts electricity much more slowly than other tissues Body Composition: An analysis of skin fold thickness on specific regions of the body using calipers is simple and inexpensive, and if done correctly can accurately measure the amount of fat Body Composition: While the total amount of fat is an important risk factor for health problems and early death, where the fat is located is also an important risk factor. Body Composition: While the total amount of fat is an important risk factor for health problems and early death, where the fat is located is also an important risk factor. Fat deposited above the waist, primarily in the abdomen, is called android obesity because it is more common in men. Body Composition: While the total amount of fat is an important risk factor for health problems and early death, where the fat is located is also an important risk factor. Fat deposited above the waist, primarily in the abdomen, is called android obesity because it is more common in men. Fat deposited below the waist, primarily around the hips, butt, and thighs, is called gynoid obesity because it is more common in women. Body Composition: While the total amount of fat is an important risk factor for health problems and early death, where the fat is located is also an important risk factor. Android obesity, the “apple” shape, indicates a higher risk of disease and death than gynoid obesity, the “pear” shape. Body Composition: A simple way to identify where fat is being deposited is to measure the waist and hips. A waist measurement greater than - 35 inches for women or - 40 inches for men is a sign of increased health risk in individuals with body mass indices between 25 kg/m2 and 35 kg/m2 Overweight and Obesity In fact, obesity has now become the largest contributor to health problems and death throughout the United States and many other countries. - the number of adults with BMIs > 25kg/m2 in the US has increased from 48% to more than 65% in the past 30 years. Overweight and Obesity In fact, obesity has now become the largest contributor to health problems and death throughout the United States and many other countries. - the number of adults with BMIs > 25kg/m2 in the US has increased from 48% to more than 65% in the past 30 years. - one out of five (17%) of U.S. children aged 6 to 19 are overweight or obese. Overweight and Obesity In fact, obesity has now become the largest contributor to health problems and death throughout the United States and many other countries. - the number of adults with BMIs > 25kg/m2 in the US has increased from 48% to more than 65% in the past 30 years. - one out of five (17%) of U.S. children aged 6 to 19 are overweight or obese. - 300,000 deaths each year are due to obesity among US adults. Overweight and Obesity In fact, obesity has now become the largest contributor to health problems and death throughout the United States and many other countries. - the number of adults with BMIs > 25kg/m2 in the US has increased from 48% to more than 65% in the past 30 years. - one out of five (17%) of U.S. children aged 6 to 19 are overweight or obese. - 300,000 deaths each year are due to obesity among US adults. - More than 90% of Type 2 diabetes in the US is due to obesity. Overweight and Obesity Overweight and Obesity Table 8.7 in your textbook lists some of the more common “risks of being overweight”. Be sure you are familiar with the information in this table. It will be “fair game” on exams. Overweight and Obesity So: What is causing this rise in the number of overweight (BMI > 25kg/m2 ) and obese (BMI > 25kg/m2 ) individuals? Biological Factors: Genetics and Heredity You are more likely to be overweight or obese if one or both of your parents are, particularly if they developed it earlier in life. Overweight and Obesity So: What is causing this rise in the number of overweight (BMI > 25kg/m2 ) and obese (BMI > 25kg/m2 ) individuals? Biological Factors: Genetics and Heredity Number and size of fat cells The more fat cells you have, and/or the bigger they are, the greater your risk of becoming overweight or obese Overweight and Obesity So: What is causing this rise in the number of overweight (BMI > 25kg/m2 ) and obese (BMI > 25kg/m2 ) individuals? Biological Factors: Genetics and Heredity Number and size of fat cells Sex Women have somewhat higher rates of overweight and obesity than do men Overweight and Obesity So: What is causing this rise in the number of overweight (BMI > 25kg/m2 ) and obese (BMI > 25kg/m2 ) individuals? Biological Factors: Genetics and Heredity Number and size of fat cells Sex Age Throughout most of your life, your risk of overweight and obesity increases, then declines as you get elderly. Childhood obesity is one of the fastest growing groups. Overweight and Obesity So: What is causing this rise in the number of overweight (BMI > 25kg/m2 ) and obese (BMI > 25kg/m2 ) individuals? Biological Factors: Genetics and Heredity Number and size of fat cells Sex Age Race and ethnicity In the US, hispanic and black women are more likely to be overweight or obese than white or Asian women. Rates are similar among black, white, and hispanic men but greater than in Asian men. Overweight and Obesity So: What is causing this rise in the number of overweight (BMI > 25kg/m2 ) and obese (BMI > 25kg/m2 ) individuals? Biological Factors: Genetics and Heredity Number and size of fat cells Sex Age Race and ethnicity There are obviously many social & environmental factors as well Overweight and Obesity Overweight and Obesity So: What is causing this rise in the number of overweight (BMI > 25kg/m2 ) and obese (BMI > 25kg/m2 ) individuals? Lifestyle and Psychological Factors: Lack of physical activity is the greatest contributing factor to overweight and obesity. Only about 20% of all Americans get adequate exercise. 25% are essentially not active at all Overweight and Obesity So: What is causing this rise in the number of overweight (BMI > 25kg/m2 ) and obese (BMI > 25kg/m2 ) individuals? Lifestyle and Psychological Factors: The desire for sexual attractiveness, often linked with inaccurate body image, drives both eating and exercise decisions. Overweight and Obesity So: What is causing this rise in the number of overweight (BMI > 25kg/m2 ) and obese (BMI > 25kg/m2 ) individuals? Lifestyle and Psychological Factors: Emotional stress and depression are known to be risk factors for overweight and obesity. Overweight and Obesity So: What is causing this rise in the number of overweight (BMI > 25kg/m2 ) and obese (BMI > 25kg/m2 ) individuals? Lifestyle and Psychological Factors: Binge eating, bulemia nervosa, and other eating disorders are linked to overweight and obesity. More than 8,000,000 Americans have an eating disorder, 85% of whom are female Weight Management: Obviously, proper weight management is necessary for good health, and that requires energy equilibrium: Energy intake must equal energy output: If energy intake exceeds energy output (“positive energy balance”) the extra calories will be stored as fat - you will gain weight. If energy output exceeds energy intake (“negative energy balance your body will used stored fat and glycogen (and, if necessary, protein) to produce energy you will lose weight Weight Management: Weight management is the adoption of healthy and sustainable eating and exercise behaviors indicated for reduced disease risk and improved feelings of energy and well-being. Note the two components: Eating behaviors and Exercise behaviors These can be difficult to develop and maintain, particularly as we get older. Weight Management: - Be aware of what you eat and the number of calories Weight Management: - Be aware of what you eat and the number of calories - Balance energy intake among fat (20-35% of calories) protein (0.8g per kg body wt) carbohydrate (45-65% of calories) Weight Management: - Be aware of what you eat and the number of calories - Balance energy intake among fat (20-35% of calories) protein (0.8g per kg body wt) carbohydrate (45-65% of calories) - Eat regularly (don’t skip meals) Weight Management: - Be aware of what you eat and the number of calories - Balance energy intake among fat (20-35% of calories) protein (0.8g per kg body wt) carbohydrate (45-65% of calories) - Eat regularly (don’t skip meals) - Select diet behaviors that will be easy to maintain Weight Management: - Be aware of what you eat and the number of calories - Balance energy intake among fat (20-35% of calories) protein (0.8g per kg body wt) carbohydrate (45-65% of calories) - Eat regularly (don’t skip meals) - Select diet behaviors that will be easy to maintain - Stay active and/or get regular exercise Weight Management: - Be aware of what you eat and the number of calories - Balance energy intake among fat (20-35% of calories) protein (0.8g per kg body wt) carbohydrate (45-65% of calories) - Eat regularly (don’t skip meals) - Select diet behaviors that will be easy to maintain - Stay active and/or get regular exercise - Manage your psychological health Weight Management: For most people, that is difficult to do. Effective weight management requires being aware of the factors which influence both diet (energy intake) and exercise (energy output), and then the conscious modification of behaviors. Weight Management: Many people, of course, are unwilling or unable to make the behavioral changes necessary for weight managment. Weight Management: Many people, of course, are unwilling or unable to make the behavioral changes necessary for weight managment. There are hundreds of over-the counter drugs or supplements which promise to suppress your appetite, “burn fat”, etc. Weight Management: Many people, of course, are unwilling or unable to make the behavioral changes necessary for weight managment. There are hundreds of over-the counter drugs or supplements which promise to suppress your appetite, “burn fat”, etc. Many of these are relatively harmless herbal supplements, but others such as the amphetamines can be dangerous. Weight Management: There are some presciption drugs which can be used to assist in weight management: Phentermine is an appetite suppressant Xenical interferes with the absorption of diglycerides and triglycerides by the intestines. These are almost always used in combination with behavior modification and exercise. Weight Management: There are also hundreds of diet plans advertised or promoted through popular literature The Atkins Diet The Pritikin Principle The Zone Diet The South Beach Diet Ornish Diet Jenny Craig Nutrisystem Weight Watchers Weight Management: Last resort: Surgery Underweight: While most health issues related to weight management are due to overweight and obesity, calling for weight loss, you will also encounter issues related to being underweight and thus needing to gain weight. - Elderly - Children - Illness - Metabolic disorders - Eating disorders - Prolonged emotional or physical stress - Alcoholism Underweight: Weight-gain strategies: Small, frequent meals Fluids between meals High-calorie foods and beverages Timers or other cues Supplements