interventions for clients with gastrointestinal problems
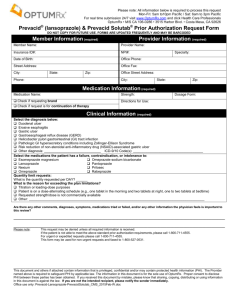
advertisement

INTERVENTIONS FOR CLIENTS WITH GASTROINTESTINAL PROBLEMS PEPTIC ULCER CHOLYCYSTITIS PANCREATITIS 2010 HOW DO ULCERS DIFFER? • • • • PEPTIC ULCER GASTRIC ULCER DUODENAL ULCERS STRESS ULCER PAIN COMPARED • Gastric Ulcer: occurs 30-60 min after a meal, rarely at night, accentuated by food • Duodenal Ulcer: Occurs 1 1/2 - 3 hours after a meal, often awakened at night between 1-2 AM, relieved by ingestion of food COMPLICATIONS OF ULCERS • HEMORRHAGE • PERFORATION • PYLORIC OBSTRUCTION Assessment indicating hemorrhage • • • • • • Hematemesis Melena Coffee Ground Emesis Black stool Hematochezia Profuse upper GI hemorrhage Assessment indicating Perforation • • • • • • • Sudden sharp pain Apprehension Abdominal assessment Client position peritonitis Bowel sounds MEDICAL EMERGENCY, LIFE THREATENING Assessment indicating Obstruction PYLORIC OBSTRUCTION: Nausea/Vomiting GASTRIC OUTLET OBSTRUCTION: • Abdominal bloating • Nausea/Vomiting • F & E imbalances Assessment indicating Obstruction PYLORIC OBSTRUCTION: Nausea/Vomiting GASTRIC OUTLET OBSTRUCTION: • Abdominal bloating • Nausea/Vomiting • F & E imbalances TEACHING CAUSE • Use of certain drugs • Bacterial infection • Genetics ASSESSMENT • • • • • • HISTORY Physical assessment What is the most common symptom? Where is pain? How is the pain described? How is the pain different from gastric to duodenal ulcer? • What other symptom is associated? LABORATORY ASSESSMENT • • • • • Hgb, Hct Stool specimen Ba enema Upper right abdomen series ***EGD (esophagogastroduodenoscopy) • Biopsy ASSESSMENT CONTINUED SMOKING CESSATION: • smoking decreases the secretion of bicarbonate from the pancreas into the duodenum • Acidity of the duodenum is higher when one smokes Assessment Continued SMOKING CESSATION: • smoking decreases the secretion of bicarbonate from the pancreas into the duodenum • Acidity of the duodenum is higher when one smokes NURSING DIAGNOSIS • • • • • • • • Knowledge deficit RT Imbalanced nutrition RT Disturbed sleep RT Risk for falls RT Fatigue RT Nausea RT Ineffective Health Maintenance RT Fear RT DRUG THERAPY GOALS: DRUGS for H. pylori bismuth compound or proton pump inhibitor and two antibiotics BISMUTH: Pepto-Bismol PROTON PUMP INHIBITORS: omeprazole (Prilosec) COMBINATION OF ANTIBIOTICS: metronidazole (Flagyl) & Tetracycline clarithromycin & amoxicillin CHALLENGE WITH THIS REGIMEN? HYPOSECRETORY DRUGS • • • • Reduces gastric acid secretions 1. antisecretory agents 2. H2 receptor antagonists 3. Prostaglandin analogues ANTISECRETORY AGENTS Or PROTON PUMP INHIBITORS EXAMPLES: • omeprazole (Prilosec) • lansoprazole (Prevacid) • rabeprazole (Aciphex) • pantoprazole (Protonix) • esomeprazole magnesium (Nexium) H2 Receptor Antagonists • Block histamine stimulated gastric secretions • OTC Examples: • rantidine (Zantac) • famotidine (Pepcid) • nizatidine (Axid) PROSTAGLANDIN ANALOGUES • HOW: reduce gastric acid secretion and enhance gastric mucosal resistance to tissue injury • EXAMPLES: • Misoprostol (Cytotec) DRUGS CONTINUED Hyposecretory Drugs antisecretory Agents H2 receptor antagonist Prostaglandin analogues Antacids ANATACIDS • HOW: – buffer gastric acid and prevent the formation of pepsin – Speeds up healing of duodenal ulcers EXAMPLES: • Mylanta (magnesium containing) • Maalox (aluminum containing) • TUMS (calcium containing) • Simethicone Combination products: Gelusil & Mylanta Problems: INTERACTION WITH DRUGS & • HIGH SODIUM CONTENT MUCOSAL BARRIER FORTIFIERS • Forms a protective coat • EXAMPLE: – Sucralfate (Carafate) • INSTRUCTIONS FOR ADMINISTRATION: DIET • CONTROVERSY • What is known about food? • Instruct client about foods that increase gastric acid secretion SURGICAL INTERVENTION • Seen in 10-15% of pts INDICATIONS FOR SURGERY: • life threatening bleeding • Perforation • Obstruction TYPE OF SURGERY: • GASTRIC RESECTION: remove the gastrin producing portion of the stomach ADDITIONAL SURGERY: BILROTH I AND II • Used to remove ulcers and cancer, not for peptic ulcer disease • Bilroth I (gastroduodenostomy): fundus of stomach anastomosed to duodenum • Bilroth II (gastrojejunostomy) duodenum is closed, fundus of stomach anastomosed into the jejunum • Heineke-Mikulicz pyloroplasty: enlarges pyloric stricture (most common) ASSESSMENT POSTOP • • • • Observe for blood from NGT Observe for abdominal distention REPORT TO SURGEON IRRIGATION OF NGT: not done POSTOP PROBLEMS RELATED TO BILROTH PROCEDURES DUMPING SYNDROME: vasomotor symptoms after eating after Billroth II procedure RESULTS from rapid emptying of gastric contents into the small intestine which shifts fluid into the gut causing abdominal distention • EARLY S&S seen 30 min after eating:vertigo, tachycardia, syncope, sweating, pallor, palpitations and desire to lie down • LATE S&S: 90 min-3hrs after eating caused by excessive amt of insulin: dizziness. • Light headedness, palpitations, diaphoresis, confusion TREATMENT OF DUMPING SYNDROME • 6 small meals a day high in protein and fat and low in CHO; avoid fluids during meals • Avoid refined or concentrated CHO because they leave the stomach quickly • Eat slowly • Vitamins for nutritional deficiencies • Anticholinergics: decrease stomach motility • Somatostatin analogue: octreotide (Sandostatin) Synthetic form of the hormone found in GI tract used to inhibit dumping syndrome OTHER COMPLICATIONS • Alkaline Reflux gastropathy or bile reflux gastropathy • Delayed gastric emptying • Afferent loop syndrome • Recurrent ulceration REVIEW ALL OF THESE: see page 1303-1304 NUTRITIONAL PROBLEMS POSTOP • deficiencies of : – vitamin B12 – folic acid – iron – impaired calcium metabolism – reduced absorption of calcium &vitamin D • WHY? • WHAT ASSESSMENTS? • WHAT TREATMENT? BILIARY DISORDERS DEFINITIONS • CHOLECYSTITIS: Inflammation of GB • CHOLELITHIASIS: caused by presence of stones • ACALCULOUS CHOLECYSTITIS: inflammation of the GB without stones • CALCULOUS CHOLECYSTITIS: Follows obstruction of the cystic duct by a stone creating an inflammation • CHOLANGITIS: infection of the bile ducts • CHOLEDOCHOLITHIASIS: common bile duct stones CHOLECYSTITIS WITH CHOLELITHIASIS STONES composed of cholesterol, bile pigment and calcium • INCIDENCE: higher in women over age 40 • PREDISPOSING FACTORS: Runs in families, obesity, middle age, multiparity, use of birth control pills, pregnancy, diabetes, after rapid weight loss, alcholism NON-SURGICAL APPROACH • Low fat diet • Replacement of fat soluable vitamins (A, D, E, K), bile salts • Weight reduction • NGT for uncontrolled vomiting • Broad spectrum antibiotics (ampicillin, tetracycline, cephalosporins) • Dissolution therapy (chenodeoxycholic acid or CDCA; ursodeosycholic acid or UDCA) • Lithotripsy • Endoscopic Retrograde Cholangiopancreatography (ERCP) NON-SURGICAL APPROACH CONTINUED DRUG THERAPY: • Meperidine hydrochloride (Demerol): pain AVOID USE OF MORPHINE (causes spasm and constriction of the sphincter of Oddi) • atropine sulfate (Atropine): anticholinergic • dicyclomine (Bentyl, Lomine): antispasmodic ASSESSMENT OF CHOLECYSTITIS AND CHOLELITHIASIS • Abdominal pain, usually in the right upper quadrant, may radiate to back or right shoulder • Pain triggered by high fat/high volume meal • Full feeling • Eructation • Dyspepsia • Flatulence • Nausea/Vomiting • Low grade fever ASSESSMENT CONTINUED: done by MD and NP • Blumberg’s sign • Murphy’s sign • • • • ASSESSMENT CONTINUED FOR CHRONIC CHOLECYSTITIS Jaundice Clay-colored stools Dark urine Steatorrhea DIAGNOSTIC ASSESSMENT • Serum alkaline phosphatase • AST (aspartate aminotransferase) • LDH (lactate dehydrogenase) • Direct serum bilirubin • Indirect serum bilirubin DIAGNOSTIC ASSESSMENT CONTINUED • WBC: • Serum amylase • Serum lipase DIAGNOSTIC ASSESSMENT Ultrasound of right upper quadrant: Hepatobiliary Scan: SURGICAL TREATMENT • CHOLECYSTECTOMY: removal of gallbladder and cystic duct • CHOLEDOCHOSTOMY: opening into the common bile duct through the abdominal wall with insertion of T-tube to keep duct open for healing • LAPAROSCOPIC CHOLECYSTECTOMY: removal of gallbladder via umbilical incision POST-OP NURSING CARE FOR LAP CHOLECYSTECTOMY • May be same day surgery/ or 1-2 hospital stay • Must be able to tolerate food, ambulate, and have stable vital signs to be discharged • Mild to moderate pain for two days postop • Mild discomfort for one week • No lifting heavier than 5 lbs • Normal activity in 1-3 weeks • • • • • • POSTOP NURSING CARE FOR PT WITH OPEN CHOLECYSTECTOMY PCA for severe postop pain (avoid morphine) Low to semi Fowler’s position C &DB Change dressing (usually off in 24 hrs) IV fluids/NPO Advance from low fat clear liquids to low fat bland diet as tolerated; many clients don’t need special diet • Antiemetics • Surgical drain for 24 hours • T-tube (placed to keep the common bile duct open) COMPLICATIONS OBSTRUCTION: • Clay colored stool or steatorrhea means no bile in intestinal track • CALL SURGEON! HEMORRHAGE: • Check VS, incisions, tubes, increased tenderness or rigidity of abdomen • CALL SURGEON! COMPLICATIONS INFECTION • Pain • fever DISRUPTION OF GI TRACT FUNCTION: • Vomiting, abdominal distension, increased pain PATIENT EDUCATION • Care of T-tube When to call MD: • Jaundice, dark urine, pale colored stools, pruritus (signs of obstructed bile flow) • Pain or fever (signs of infection) PATIENT EDUCATION • Teach patient to expect loose bowel movements for a few weeks to several months • Teach about low fat diet: trim fat from food, lean meats, remove skin from poultry, limit use of eggs, no frying goods, use skim milk, low fat cottage cheese, no sauces, gravies or rich desserts, increase fish and seafood. T TUBE • T-tube: biliary drainage tube Avoid tension and obstruction of tubing • Keep pt in semi Fowler’s position • Drains to bile bag kept below the level of the GB • Initially blood tinged immediately postop, then changes to green-brown bile • Assess q 2-4 hours initially then q 8 hours after 1st 24 hrs T TUBE • BILE OUTPUT: about 400 + ml/day with gradual decrease in output • REPORT DRAINAGE AMOUNTS IN EXCESS OF 1000 ml/DAY TO MD • REPORT SUDDEN INCREASES IN BILE OUTPUT AFTER NORMALLY DECREASING PATTERN T TUBE • Collect and administer excess bile output to the client via NGT (uncommon) or five synthetic bile salts (dehydrocholic acid (Decholin) • Check for infection, inflammation, irritation • NEVER IRRIGATE, ASPIRATE, CLAMP a T tube without a MD order T TUBE • Observe for pulling, kinking, tangling • When client allowed to eat, clamp T-tube for 1-2 hours before and after meals AS MD ORDERS • Assess client’s response to determine tolerance of food • Change dressing: remove dressing once a day, clean skin around tube, apply precut dressing around catheter and tape in place • Empty T tube same time each day PANCREATITIS NORMAL Pancreas has two functions: endocrine and exocrine • ENDOCRINE FUNCTION: • EXOCRINE FUNCTION: ENZYMES: trypsin, chymotrypsin, amylase, lipase PANCREATITIS DEFINED • An acute or chronic inflammation of the pancreas • Caused by autodigestion PATHOPHYSIOLOGY: 4 PROCESSESS OCCUR • • • • LIPOLYSIS PROTEOLYSIS NECROSIS OF BLOOD VESSELS INFLAMMATION LIPOLYSIS • • • • What happens to the lipase What happens to Fatty acids What do they combine with What do they form after combining • What is the end result? PROTEOLYSIS • After the trypsin is activated what happens to the pancreas? • What is the end result of this to the pancrease NECROSIS OF THE BLOOD VESSELS • What happens after elastase is activated by trypsin? • What happens with the necrosis of the blood vessels? • What happens when the client starts to hemorrhage? • What is the risk to the client? INFLAMMATION • leukocytes cluster around – hemorrhagic areas of pancreas – necrotic areas • What happens next? COMPLICATIONS:JAUNDICE Jaundice • CAUSED BY: COMPLICATIONS: BLOOD SUGAR Transient Hyperglycemia Diabetes COMPLICATIONS: OXYGENATION • Left lung pleural effusion • Atetelectasis & pneumonia • ARDS COMPLICATIONS: • Multisystem Organ Failure COMPLICATIONS: coagulation problems • DIC (disseminated intravascular coagulation) • CAUSED BY: release of necrotic tissue and enzymes into blood leads to altered coagulation COMPLICATION: • acute renal failure • CAUSED BY: COMPLICATION: • paralytic ileus • CAUSED BY TEACHING ABOUT CAUSE • Inherited • Alcohol and drug abuse • Ask about history of : – Gall Bladder Disease – Gastric/duodenal ulcer disease – Abdominal trauma – Drug toxicity – Complication of ERCP ASSESSMENT: PAIN • LOCATION: • INTENSITY: • DURATION: • WHAT CAUSES PAIN: • WHAT RELIEVES PAIN: ASSESSMENT: abdominal • 1. Jaundice • 2. Cullens Sign: • 3. Turner’s sign: • 4. Absent/decreased bowel sounds • 5. Rigidity/guarding: DIAGNOSTIC TESTS • • • • • Abdominal xray Chest xray CT scan MRI Ultrasonography NURSING DIAGNOSIS: complete the cause • Acute pain RT • Imbalanced nutrition RT • Nausea RT • Risk for infection RT • Ineffective breathing pattern RT • Risk for activity intolerance • Disturbed sleep pattern RT LABORATORY TESTS: which are elevated/lowered and why? • • • • • • • Serum amylase Serum lipase******* Serum trypsin Serum elastase WBC Serum glucose Serum ALT (alanine aminotransferase) • Bilirubin • Alkaline phosphatase • Serum calcium • Serum magnesium IMPLEMENTATION GOAL: • Decrease GI pain • Decrease GI tract activity • Decrease pancreatic stimulation HOW? 1.Fasting 2.Drug Therapy 3.Comfort 4.Manage life threatening complications WHAT WILL BE ORDERED TO MEET THE GOALS? 1.Fasting 2.Drug Therapy 3. Activity 3.psychosocial MEDICATIONS: PAIN • Demerol (meperidine) • Transdermal fentanyl (Duragesic) • Epidural morphine with bupivacaine MEDICATIONS: GOAL: To decrease vagal stimulation To decrease GI motility To inhibit pancreatic secretions WHAT DRUGS: • Anticholinergics: atropine (Urised) • Calcium gluconate IV • Antibiotics: cefuroxime (Zinacef), ceftazidime (Ceptaz), imipenem cilastin (Primaxin) • Antacids and Histamine blockers (ranitidine (Zantac) MEDICATIONS ENZYME REPLACEMENT contains what? • EXAMPLES: – pancreatin(Donnazyme, Creon) – Pancrelipase (Cotazym, Viokase, Pancrease) • What is the PURPOSE: What to teach client about ENZYME REPLACEMENT: • • • • • • • When to take around meals? What to take it with? Can the drug be broken, crushed, chewed? What can be done with capsules? What foods shouldn’t be mixed with? What precautions should be told to client? What is the therapeutic outcome? REFERRALS • Counselor • Self help group • Alcoholics Anonymous if appropriate