Unit 1 fetal development case study
advertisement

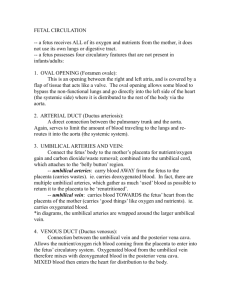
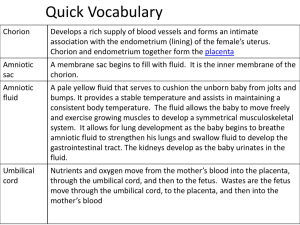
Unit 1 fetal development case study Elizabeth Kelley Buzbee AAS, RRT-NPS, RCP Case study # 1 • Your patient is in L & D. She is a 48 year old LAF. What else do you want to know about this patient? Answer: • Her vital signs: HR 125 sinus tachycardia, RR 18 bpm without retractions, BP 158/90 mmHg she is afebrile • Her Sp02: 99% on room air • Her BS: clear to all lobe, diminished in the basal areas. • Pregnancy history: week 28 • Prior medical History: She is G4, P3 A1 • Hx of Gestational diabetes with the last two pregnancies • What is the significance of her past history? answer • Her VS are ok, and she doesn’t seem to have an infection • She has had 4 pregnancies, and 3 live births and one miscarriage. This puts her at risk for premature labor • She is older, which makes her infant at risk • The gestational diabetes puts the baby at risk • If born today, the infant will be premature, but will be viable • What is the status of her fetus at 28 weeks? What are it’s chances of survive at this point? answer • At 28 weeks the fetus should have enough pulmonary capillary bed to exchange gas • There should be enough alveoli for gas exchange • The surfactant will be started but may not be at sufficient levels to prevent respiratory distress—the maternal diabetes will slow down surfactant production • The CNS may not be developed enough to handle hypoxemia and hypercapnia appropriately • What is the blood flow from umbilical vein to umbilical artery? Answer: • Blood from the placenta gets to the single umbilical vein that goes to the belly and enters the liver where part of the blood goes to the portal circulation and the rest goes into the IVC via the D. Venosus where it enters the RA and goes into the Foreman Ovale & into the LA and LV to go out into the fetal body • What happens to the blood in the SVC? answer • The blood in the SVC drains the head and shoulders and this Desaturated blood enters the RA goes to the RV and into the pulmonary trunk where it is shunted away from the lung into the D. Arteriosus to the Aorta • In the descending Aorta, this Desaturated blood mixes with the saturated blood from the IVC and drops the fetal P02 from the mid 30-40s to the mid 20s • Labor started with the water breaking [ruptured membranes] at midnight on Sunday. The labor was spontaneous, vertex, vaginal delivery. There were some early decells • The baby is born at 0800 on Tuesday. He is a little boy. • What if anything is significant about this series of events? answer • The time between the rupture of membranes and the birth of the baby exceeds 24 hours. This is called Premature rupture of membranes PROM which places the baby at risk for infection. • SVVD is normal, but the delivery is premature • early decells are not as serious as late decell. The HR rises back to baseline after each contraction The umbilical cord is attached to what? answer • To the baby’s belly and to the placenta • How many blood vessels should be present in the umbilical cord? answer • Three vessels: • Two umbilical arteries • One umbilical vein • Which of these vessels carries blood with the most 02 [to the fetus]? answer • The umbilical vein carries blood to the fetus from the placenta • How do gases and waste product exchange between the mother and fetus? answer • The maternal blood flow goes to the maternal side of the placenta. The Pa02 is 80-100 mmHg. • The maternal blood is sent into the spaces around the chonrion villi where gases diffuse into the fetal blood. • fetal capillaries in the placenta regroup into veins that drain into the single umbilical vein which carries the saturated blood to the fetus at a P02 of 31-42 mmHg • At the OB gyn’s request, you draw and run a cord gas from the umbilical vein . You get the following data: • pH 7.34 • P02 40 • PC02 35 • What do you think about these gases? answer • This is wnl for cord gases for fetus between 25 weeks and term • As soon as the infant starts to breath these data will change • The baby takes his first breath. If all goes well what happens? answer • The first few breaths will increase the RV so that [1] PA02 rises [2] lung Compliance rises • The rising PA02 will reverse the longstanding pulmonary HTN and the RV pressure will drop which lowers RA pressure. • The rising PA02 will raise the Pa02 and that will close the D. Arteriosus • Once the cord is clamped the systemic blood pressure rises so that the RA pressure is lower than the LA pressure and the Foreman Ovale will close. • At 1 minute of life the baby has the following: • Flaccid • Extremities blue, central cyanosis • HR 135 • Regular at 55 bpm • Grimaces with catheter to nose • What is this infant’s APGAR score at 1 minute? What intervention is needed? answer • 0 for muscle tone • 0 for color • 2 for HR • 2 for respiratory effort • 1 for reflex • APGAR at 1 minute is 5 What intervention is needed at this point? answer 1. Warm and stimulate the baby by rubbing him down with towel. 2. Attach pulse oximeter to right hand [post-ductal] 3. Continue to monitor HR and RR 4. Assess the respirations for s/s of respiratory distress [Silverman score] • You are blowing 02 to his face. His Sp02 rises from 75% to 91% • In 5 minutes, he has the following data: • HR 140 • Crying loudly [respiratory rate 48 bpm] • Extremities blue but lips pink • Arms and legs flexed • What is his APGAR and what is his prognosis? answer • His APGAR at 5 “ is 7 and his prognosis is excellent, although he might need supplementary 02 for a day or so