Precipitous Delivery
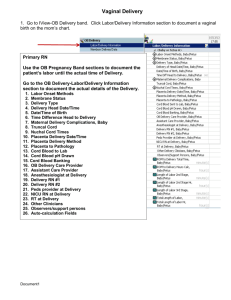
advertisement

Precipitous Delivery Renae Buehner RNC, BSN Labor and Delivery Unit Supervisor Avera McKennan Hospital Definition: Precipitous Delivery, aka Precip Occurs when cervical dilatation is faster than 5 cm per hour (or 1 cm every 12 minutes) in nulliparas and 10cm per hour (1cm every 6 minutes) in multiparas. (Kennedy, Ruth, & Martin, 2009) The term precipitate or precipitous labor has been defined as a labor that lasts no more than three hours from onset of regular contractions to delivery. (Barss, 2014) Treatment • The best action for precipitous labor is to anticipate a rapid descent of the fetus and a spontaneous delivery. • Prepare for the potential of a stressed newborn What do you do first? PANIC!!! No really… • Call for help. There are two patients in a delivery, the mother and the infant; each should have at least one health care provider. An obstetrician and pediatrician or family practitioners should be summoned, if available. • Ask the woman her gravidity and parity. Find out if she has any obstetrical or medical problems, such as twin gestation, preterm fetus, previous cesarean delivery, fetal anomalies, or other medical conditions. Also ask if she has a headache, or epigastric pain, or vision changes which are signs of preeclampsia. • Perform a brief assessment: Is the fetus visible and beginning to emerge from the vagina (ie, crowning)? Is the presenting part the scalp, buttocks, or foot? In 95 percent of pregnancies, the presenting part is the fetal head. Is the amniotic sac intact? If it is, leave it alone until it ruptures naturally. Assess the situation •If there is time and equipment is available, check the maternal temperature and blood pressure. •Fever suggests chorioamnionitis. •Maternal hypertension (systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg). •Preeclampsia can progress to eclampsia (seizures) and can be associated with life-threatening complications (hepatic rupture, pulmonary edema, stroke, renal failure) Patient Preparation • Insert an IV, 16-20 gauge. This can be used for oxytocin infusion after delivery and fluid volume replacement. • Collect blood tubes for CBC,T&S, and RPR What to expect • Shaking is normal. It is usually a sign of transition. Comes from surge of hormones including adrenaline. • As the baby comes down the birth canal you will see the perineum flatten, then bulge. Often you will see rectal bulging. • Cervical change usually brings bloody show. • Often the patient will need guidance on how to breathe and get control. She’s Pushing! What you need: • Sterile gloves and gowns • Bulb syringe to remove fluid and mucus from the infant's mouth and nose • Two sterile clamps to clamp the umbilical cord • Sterile scissors or knife to cut the umbilical cord between the clamps • A red top tube to collect fetal blood from the end of the cut umbilical cord • Clean towels, sheets, and/or blankets to dry and swaddle the infant • Blankets to keep the mother warm • Suitable containers for the placenta and wet, bloody clothing and sheets, etc. • A diaper and infant hat What to expect cont • The uterus should relax between contractions. • FHTs should be checked by a Doppler device, by auscultation with stethoscope, or with use of a portable ultrasound unit, if available. • Normal FHR is 110-160 bpm • FHR may decrease with the contraction. This is a sign of head compression. When the contraction is letting up the FHR should come back up. Cardinal Movements • Cardinal Movements. This refers to the movements made by the fetus during the first and second stage of labor. As the force of the uterine contractions stimulates effacement and dilatation of the cervix, the fetus moves toward the cervix. When the presenting part reaches the pelvic bones, it must make adjustments to pass through the pelvis and down the birth canal Delivery • Before the fetus is visible, the mother will want to bear down and push in response to the pain of contractions and the pressure felt from descent of the fetal head. • Ask her to pant through the peak of her contractions and try to rest and breathe normally between them. This helps to keep her from bearing down and delivering before additional help is available. • If the head is crowning, ask her to pant or make only small pushes in an attempt to achieve a controlled delivery, which is less likely to cause maternal or fetal trauma. Large crown, note bulging of perineum Delivery • Place gentle pressure on the head as it emerges. Don’t press hard against it, only enough to allow controlled birth. Gentle pressure on head and perineum support Delivery • Once the head is delivered, allow the fetus to restitute to a side. • Feel for a cord loop around the fetal head. If there is cord noted, reduce over head if loose. If it resists, either doubly clamp and cut the cord or leave it alone. • Give gentle downward pressure for anterior shoulder • Gentle upward pressure for posterior shoulder. Delivery • If you have resistance with the shoulders or see the “turtle sign” have an assistant flex the patient’s thighs back. This should open the pelvis to it’s maximum dimension. • If resistance continues, have your assistant apply suprapubic pressure. McRoberts/Suprapubic Pressure Delivery • Once the shoulders deliver, the rest will slide out. • Double clamp the cord and cut the cord between the clamps. • Bring baby to mother’s chest and dry off the baby in mother’s arms Immediately After Delivery • Start IV infusion of pitocin 30units in 500cc normal saline at 250cc/hr. Allow to run for 2 hours or until empty. Increase the rate as needed for boggy uterus or increased bleeding. • Precip deliveries are a higher risk for post partum hemorrhage. Consider pitocin 10 units IM in addition to the IV Placenta Delivery • Wait for it… The placenta can deliver immediately after the baby or can take up to 30 minutes. • Signs of placenta seperation: gush of blood, lengthening of the cord, change in the shape of the uterus. • Control the delivery of the placenta by providing gentle downward traction of the cord with one hand and the other hand supports the fundus. The mother can assist by gentle bearing down with a contraction. • Note if there is a 3 vessel cord. Placenta retention • If it has been 30 minutes and the placenta shows no sign of delivering, consider manual removal and/or possible d&c. Post Partum Hemorrhage • Cumulative blood loss of >=1000ml OR blood loss accompanied by signs/symptoms of hypovolemia within 24 hours following the birth process (includes intrapartum loss). • Signs/symptoms of hypovolemia may include tachycardia, hypotension, tachypnea, oliguria, pallor, dizziness, or altered mental status • Cumulative blood loss of 500-999ml alone should trigger increased supervision and potential interventions as clinically indicated Post Partum Hemorrhage • Interventions: 1. Pitocin infusion 2. Methergine- use cautiously in patients with hypertension 3. Hemabate-use cautiously in patients with asthma 4. Fundal massage 5. Manual evacuation of the uterus, bimanaul massage. 6. Last resort- apply aortic pressure until more help is available. Post Partum Hemorrhage • Where is the bleeding coming from? • Uterine atony? Cervical laceration? Labial laceration. • Inspect the vaginal walls, labia and cervix Baby is delivered, what do we do with it? • If the baby is crying and moving, go straight to mother’s chest. Direct skin to skin with mom and baby improves outcomes including breastfeeding, post partum depression, and bonding (www.nbci.ca) Apgar Scores • If able, start the apgar timer at birth. It will alarm at 1 minute, 5 minutes, and 10 minutes. Sign 0 1 2 Heart Rate not detectable <100 >100 Respiratory Rate absent slow, irregular good, crying Muscle tone flaccid some extremity flexion active motion Reflex Irritability no response grimace grimace, cough, sneeze, gag Color blue, pale body pink, extremities blue completely pink Apgar Score • Useful for a quick evaluation of newborn. May helpful in the initial evaluation for resuscitation • 7-10: doing well, no assistance is usually needed • 4-6: may need some resuscitation • 0-3: resuscitation needed immediately Apgar Scores • Remember: the apgar score is a clinical evaluation of the need for newborn resuscitation. It does not determine newborn hypoxia, acidosis, or neurologic impairment, nor does it predict long-term outcomes. (Kennedy, 2009) Newborn Resuscitation Newborn Assessment • Initial assessment at birth includes: Head- shape, bruising, fontanelles- soft, bulging, sunken- sutures- overriding, seperated Heart- rate, rhythm, murmur? Lungs- rate, rhythm, clear or coarse- if coarse encourage crying Bowel sounds- present or absent Skin- color, rash, petechia, birth marks, skin tags Limbs- all 10 fingers and toes Genitalia- normal, ambiguous Newborn Assessment • Along with initial assessment, obtain vital signs. • Recheck after 1 hour, 3 hours, 6 hours, and PRN • Normal heart rate 110-160 • Normal respirations 40-60 • Normal temp 97.6-99.5 Maternal Assessment • Initial assessment includes: Head to toe assessment, including high risk assessment-ha, vision changes, reflexes, pain Fundus- firm, boggy, firms with massage, midline, deviated to right or left, height Lochia- small to moderate, rubra, small clots Abnormal lochia- no flow, constant moderate trickle, clots plum size or bigger, foul odor Maternal Assessment • Breast/nipple assessment- nipples everted, flat, inverted- breasts soft, filling, tender • Assessment and vital signs of the mother should be performed at least every 15 minutes x4, every 30 minutes x2, then BID and PRN. • Encourage breastfeeding if mother and baby status allow. Note latch, swallow, and duration Questions? References • Barss, V. (2014, Mar). Up to Date. Retrieved Apr 2014, from Up to Date, Inc: www.uptodate.com • Kennedy, B., Ruth, D., & Martin, E. J. (2009). Intrapartum Management Modules. Philadelphia: Wolters Kluwer Lippincott Williams & Wilkins. • http://www.nbci.ca/index.php?option=com_cont ent&id=82:the-importance-of-skin-to-skincontact-&Itemid=17