Gynecological Sonography. A Primer
advertisement
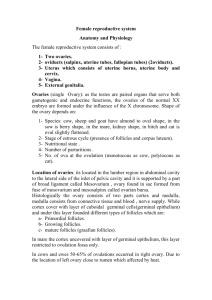
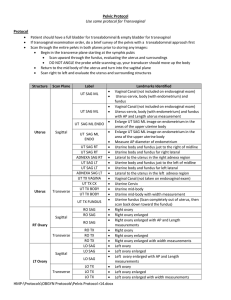
hhholdorf The uterus is a thick-walled, pear shaped, muscular organ lying posterior to the bladder and anterior to the rectum. A central echogenic line represents the endometrial cavity. Small cysts in the cervical region are a common normal variant and are known as Nabothian cysts. The uterus is composed of four parts: the fundus, the corpus (body), the isthmus, and the cervix. Normal uterine measurements in nulliparous menstruating women are 6 to 9 cm in length and up to 4 cm in anterior posterior diameter and width. The uterus of parous women will have slightly larger dimensions. Before puberty the uterus is about 3 cm long and more or less tubular in shape. After menopause the uterus shrinks in size but retains the shape it adopted with the onset of puberty. The menstruating uterus widens toward the fundus and the cornua, the bilateral somewhat triangular regions where the fallopian tubes insert. It is tubular in the part near the vagina known as the cervix. Usually the uterus is tilted anteriorly (Anteversion); but may be normally tilted posteriorly (retroversion). An acute angulation in the midportion is known as anteflexion or Retroflexion. Although usually in a midline position, the uterus may lie obliquely to the left or the right. Uterine positional variations ◦ Anteversion: Refers to the cervix, which is anchored at the angle of the bladder and less freely movable than the corpus (body) and Fundus (top), forming a 90-degree angle with the vagina ◦ Retroversion: refers to the cervix oriented more linearly in relation to the vagina. The lining of the endometrial cavity is partially shed each month at menstruation, with consequent changes in cavity appearance during the course of the cycle. During the pre-ovulatory (Proliferative) phase, the endometrial cavity echo is only about 3mm thick and surrounded by an echopenic halo. Shortly before ovulation, two additional linear echoes outline the echopenic are (the “three line sign”). The echopenic area becomes more echogenic so that in the postovulatory (secretory or luteal) phase, the cavity echo becomes brighter and thicker. At this point, the width of the canal is between 9mm and 1.3 cm thick. The lumen of the normal fallopian tubes cannot be seen. The fallopian tubes lie within the broad ligament. They can often be traced from the uterine fundus to the ovaries on endovaginal view. This is especially easy if there is cul-de-sac fluid. The ovaries are usually found at the level of the uterine fundus where the uterus becomes triangular (the cornu). Often the broad ligament can be traced laterally to the ovary. The ovaries often lie adjacent to the Iliopsosas muscle, within which lies an echogenic focus that is due to the femoral nerve sheath. The iliac vessels usually lie laterally to the ovary. In the menstruating woman, ovaries normally measure approximately 2 x 2.5 x 3cm. There is variation, so 5 x 2 x 1.5 cm or 4 x 3 x 1.5 cm, for example, are measurements that may be within normal limits. The ovaries are about 1 cubic centimeter in young girls, gradually increasing in size as puberty approaches. In menopausal women, the size of the ovary gradually decreases. Normally, one follicle grows to a size of between 1.4 and 2.5cm, alternating sides each menstrual cycle. Hormonal stimulation with drugs such as Pergonal or Clomid increases the number of dominant follicles, which may number as many as six or more in each ovary. Follicles are not seen in menopausal women, but are often seen in young girls before puberty. A dominant follicle normally bursts and disappears at mid-cycle. It is replaced by a corpus luteum. Typically, a corpus luteum has a thick, slightly echogenic vascular rim (the rim of fire on color Doppler) and an echopenic center. The central echopenic area may be large if there is much bleeding at the time of ovulation. The corpus luteum will usually disappear within a week or so. The ovarian arteries should be demonstrated using color Doppler. Uterine artery should be demonstrated using color Doppler. Small amounts of fluid may normally collect behind the uterus in the poster cul-de-sac; also know as the pouch of Douglas. The fluid may result form normal ovulation. The anterior cul-de-sac is anterior and superior to the uterine fundus. Bands of muscle tissue play an important role in maintaining the position of the uterus and ovaries. The broad ligament extends from the lateral uterine walls to the pelvic sidewalls. The obturator internus muscles lay alongside the bony wall, lateral to the ovaries. The Iliopsoas muscles are lateral and anterior to the iliac crest; the femoral nerve sheath is seen as an echogenic area within the muscle. The levator ani, piriformis, and coccygeus muscles make up the pelvic floor and are located posterior to the uterus, vagina, and rectum. Distention of the urinary bladder is essential for a high-quality transabdominal pelvic sonogram. The full bladder displaces bowel and repositions the uterus in a more longitudinal fashion that allows the US beam to transect the uterus perpendicularly. The urinary bladder provides an acoustic window for better visualization of the pelvic structures. Over-distention or underdistention of the bladder can distort or obscure the view. A sufficiently full bladder will extend just over the uterine fundus. If the bladder is too full, encourage the patient to void into a paper cup so she does not empty her bladder completely. The sonographic examination should begin in a longitudinal fashion by attempting to align the uterus with the vagina. The uterus can be recognized by the central line of the endometrial cavity and by its alignment with the vagina. The vagina is visualized as an echogenic line with relatively sonolucent walls. The uterus is normally located in the midline, but it may be deviated to either side in an oblique axis. Make sure that the bladder is full enough to show the fundus when the uterus is examined. An Anteflexed or retroverted uterus may become more normal in position and shape if the bladder is filled. Scanning at right angles to the axis of the uterus should demonstrate the ovaries. The ovaries are usually close to the triangular cornual regions near the uterine fundus. Caudal angulations are helpful for visualizing the pelvic musculature and retroverted uteri. Cranial or caudal angulations may be necessary to see the ovaries. A water enema can be helpful in the positive identification of bowel. Only a small amount of fluid need be run into the rectum through a small enema tube during observation with real-time. A flickering motion is visible when the water is running through the bowel. Do not mistake aortic pulsation or respiratory motion for peristalsis. This technique is rarely used now that endovaginal Sonography is available. Transverse Lower uterine segment Mid uterine segment Upper uterine segment Left adnexae to show left ovary and ligaments Right adnexae to show right ovary and ligaments Longitudinal Mid line to show endometrial strip concurrent with the vaginal stripe Fundus must be delineated via a full urinary bladder RT adnexae to show ovary and ligaments Left adnexae to show ovary and ligaments Rectus abominis Psoas Major Iliacus Levantor ani and coccygeus Obturator Internus Piriformis HomeworkSubmit ultrasound images and diagrams of the above pelvic musculature ESPECIALLY the Psoas Major and Levantor ani muscle groups. HOMEWORK Create a story board outlining the technique of examining the uterus with a Transabdominal approach.