The cardiovascular system
advertisement
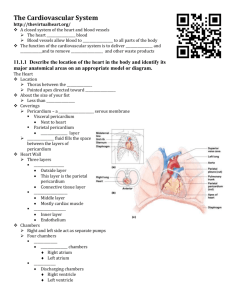
THE CARDIOVASCULAR SYSTEM Honors Anatomy Chapter 18 Heart a Pump Left Side receives O2-rich blood from lungs -- > pumps it to tissues Right Side receives O2-poor blood from tissues pumps it to lungs Heart Anatomy ~ fist size 250 – 350 g mass (<1 lb) in mediastinum: Heart Anatomy - 2 Heart rests on superior surface of diaphragm anterior to vertebral column posterior to sternum just left of midsternal line Base & Apex of Heart Coverings of the Heart 1. Pericardium: dbl-walled sac that heart is in 2 layers: Fibrous Pericaridum: dense CT 2. protection anchors heart to surrounding structures prevents overfilling of heart with blood Serous Pericardium:2 layers Parietal layer: lines internal surface of fibrous pericardium Visceral layer = epicardium Coverings of the Heart - 2 2. Serous Pericardium: 2 layers forms closed sac around heart = pericardial cavity contains serous fluid: lubricates, decreasing friction of moving pumping heart Parietal layer: lines internal surface of fibrous pericardium Visceral layer = epicardium covers heart Layers of Heart Wall 1. 2. 3. 3 layers: Epicardium = visceral layer of serous pericardium Myocardium: cardiac muscle Endocardium : squamous epithelium lining chambers of the heart Chambers of the Heart 2 superior atria separated by interatrial septum 2 larger ventricles separated by interventricular septum 2 grooves seen on exterior view of heart: 1. Coronary sulcus between upper & lower chambers 2. Anterior/Posterior Interventricular Sulcus between ventricles Atria right & left both have wrinkled, protruding appendages = auricles “little ear” Right Atrium: 2 internal features: 1. posterior wall is smooth 2. anterior wall has ridges of muscle = pectinate muscles Left Atrium: pectinate muscles only in its auricle Fossa Ovalis depression in interatrial septum marks opening of foramen ovale =“oval window” an opening in fetal heart that shunted blood from right left atrium (blood does not go to lung for oxygenation until birth) Functions of Atria receiving chambers of the heart Right: forms anterior surface of heart deoxygenated blood from all parts of body through inferior & superior vena cavas and from the coronary sinus = venous blood from myocardium Left: oxygenated blood from lungs through pulmonary veins Ventricle Features Trabeculae Carnae: irregular ridges of muscle on internal walls Papillary Muscles: conelike muscle bundles attached to heart valves via cordae tendinae Functions of the Ventricles receive blood from atria Right Ventricle: pumps deoxygenated blood to lungs through pulmonary trunk pulmonary arteries Left Ventricle: pumps oxygenated blood to entire body through aorta Heart Valves blood flows through the heart in one direction: atria ventricle valves connected to papillary muscles by chordae tendinae 1 way direction due to 4 heart valves open/close in response to differences in BP on their 2 sides https://www.youtube.com/watch?v=y5maHDAk zUs Atrioventricular Valves Tricuspid Valve right AV valve 3 flexible cusps both AV valves close when ventricles contract/open when ventricles relax Mitral Valve left AV valve Bicuspid valve: 2 cusps Semilunar (SL) Valves Pulmonary Valve right side SL valve between right ventricle & pulmonary trunk SL valves open when ventricles contract Aortic Valve left side valve between left ventricle & aorta SL valves close when ventricles relaxed Valves https://www.youtube.com/watch?v=2jPTt23 lRB8 https://www.youtube.com/watch?v=AO_aIs WpSkI https://www.youtube.com/watch?v=1hrhPww 5jKY https://www.youtube.com/watch?v=AHBzu5 zhFuA Coronary Circulation Base of Aorta Left Right Coronary A Coronary A Anterior InterventricularA Circumflex Artery Rt Marginal Posterior Interventricular A Coronary Circulation Angina Pectoris chest pain caused by fleeting deficiency in blood delivery to myocardium cardiac muscle fibers weakened by temporary lack of O2 but do not die Myocardial Infarction MI prolonged coronary blockage cardiac fibers do die dead tissue scar tissue http://www.dnatube.com/video/1708/Myocardi al-infarction-pathology Energy Requirements of Cardiac Muscle cardiac muscle fibers have more mitochondria than other muscle fibers depend almost exclusively on aerobic respiration so cannot tolerate hypoxia for long cardiac fibers can use glucose or fatty acids as a fuel source Heart Physiology cardiac muscle has intrinsic ability to depolarize & contract (does not require nervous system) Autonomic fibers do alter basic rhythm Coronary Conduction System 1. 2. independent, coordinated activity of the heart is function of: gap junctions intrinsic conduction system noncontractile cardiac cells specialized to initiate & distribute impulses throughout the heart Arrhythmias irregular heart rhythms due to abnormal electrical activity https://health.sjm.com/arrhythmiaanswers/videos-and-animations.aspx http://www.nhlbi.nih.gov/health/healthtopics/topics/arr/types Extrinsic Innervation of the Heart 1. 1. Medulla Oblongata: cardioacceleratory center sympathetic fibers SA & AV nodes Cardioinhibitory center parasympathetic fibers SA & AV nodes ECG Electrocardiography: a graphic record of heart activity tracing the composite of all action potentials generated in nodal & contractile cells at a given time http://www.getbodysmart.com/ap/circulato rysystem/heart/electricalevents/ecg/tutori al.html Heart Sounds Auscultating thorax with stethoscope reveals 2 sounds during each heartbeat lub-dub, pause, lub-dub pause = heart is relaxed “lub” = AV valves closing louder & longer than the dub “dub” = SL valves snap shut @ beginning of ventricular relaxation Heart Sounds -2 left side valves (mitral & aortic) close slightly quicker =S1 right side valves (tricuspid & pulmonary) close ~1/4 s slower = S2 so can listen to individual valve sounds by auscultating 4 specific regions of thorax Heart Sounds affected by valves closing + flow of blood http://www.dnatube.com/video/9217/Reviewof-heart-sounds http://familymedicine.osu.edu/products/physi calexam/exam/flash/heart/heart2.cfm http://www.blaufuss.org/tutorial/index1.html Heart Murmurs abnormal heart sounds occur when blood flow strikes obstructions flow becomes turbulent can be normal in young children & elderly heart flow wall thinner & vibrate with rushing blood often indicate valve problems insufficiency or incompetence: valves not closing all the way blood regurgitates stenotic: valve not opening all the way restricts blood flow Heart Murmurs https://www.youtube.com/watch?v=6YY3O OPmUDA Valve Problems Insufficieny Stenosis Cardiac Output (CO) amount of blood pumped out by each ventricle in 1 min. Stroke Volume (SV) = vol of blood pumped out by 1 ventricle with each beat correleates contraction with force of ventricular CO = HR x SV HR = Heart Rate (pulse) average adult: SV = 70 mL, HR = 75 * CO = ~ 5.25 L/min Cardiac Reserve difference between resting & maximal CO nonathletic adult = 4-5x resting CO athletic adult = 7x resting CO Tachycardia >100 beats/min may 1. 2. 3. 4. promote fibrillation Causes: Fever Stress Drugs Heart disease Bradycardia 1. 2. 3. 4. <60 beats/min Causes: Hypothermia Drugs Parasympathetic activation well-trained athlete: endurance training hypertrophy of cardiac muscle increases SV allows lower resting HR w/out changing CO CHF 1. 2. 3. 4. Congestive Heart Failure Heart inefficient pump so circulation inadequate Causes: Coronary Atherosclerosis high BP over long period of time MIs DCM: dilated cardiomyopathy Heart Failure 1 or both sides of heart may fail left side failure pulmonary congestion right side failure peripheral congestion 1. 2. 3. 4. if 1 side fails greater strain on other side whole heart fails Treatment: removing excess fluid: diuretics reducing BP increasing contractility with digitalis Heart transplant Cardiac Tamponade fluid build-up in pericardial cavity can lead to inability of ventricles to fill fully heart cannot pump normally death if not tx’d Causes: 1. 2. 3. 4. infection (bacterial or viral) causing pericarditis MI dissecting aortic aneurysm heart surgery/ trauma Development of the Heart https://www.youtube.com/watch?v=5DIUk9 IXUaI