biochem ch 26 [3-6
advertisement

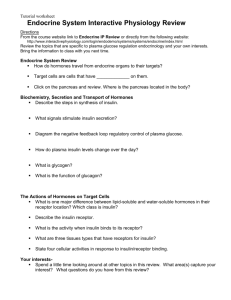
Biochem Ch 26 Metabolic Homeostasis Insulin – major anabolic hormone of body; promotes storage of fuels and use of fuels for growth Glucagon – major hormone of fuel mobilization Effects of hyperglycemia – hyperosmolar effect causes progressively severe neurologic deficits and coma o Concentration of glucose and amino acids rises above renal tubular threshold and they would be spilled over into urine o Nonenzymatic glycosylation of proteins increases, altering function of tissues in which proteins reside HbA forms HbA1c when glycosylated; high levels indicate blood glucose significantly elevated over last 12-14 weeks (half-life of Hgb in bloodstream) All membrane and serum proteins exposed to high levels of glucose can be nonenzymatically glycosylated; distorts protein structure and slows protein degradation, leading to accumulation of products in various organs, adversely affecting organ function Contributes to long-term microvascular and macrovascular complications of DM (retinopathy, nephropathy, and neuropathy, microvascular and macrovascular o Triacylglycerols in chylomicrons and VLDL rise in blood, increasing likelihood of atherosclerotic vascular disease o Can cause polyuria and subsequent polydipsia; caused by osmotic diuresis that results from high levels of glucose being excreted into urine Diuretic effect can decrease effective plasma volume, further increasing blood glucose levels o Adipose stores used, and patient loses weight despite good appetite Non-ketotic hyperosmolar coma – type 2 patients; have sufficient insulin responsiveness to block fatty acid release and ketone body formation, but unable to significantly stimulate glucose entry into peripheral tissues o Severely elevated levels of glucose causes water to leave cells and enter blood by osmosis Neuroglycopenic manifestations of severe hypoglycemia (confusion, fatigue, blurred vision) o Adrenergic response to hypoglycemic stress includes /SNS stimulation, releasing epinephrine from adrenal medulla, causing tachycardia, palpiatations, anxiety, pallor, sweating, tremulousness Major Hormones of Metabolic Homeostasis Insulin promotes storage of glucose as glycogen in liver and muscle, conversion of glucose to triacylglycerols in liver and storage in adipose tissue, and amino acid uptake and protein synthesis in skeletal muscle o Increases synthesis of albumin and other proteins by liver o Promotes use of glucose as fuel by facilitating transport into muscle and adipose tissue o Inhibits fuel mobilization Glucagon stimulates release of glucose from liver glycogen; stimulates gluconeogenesis from lactate, glycerol, and amino acids; mobilizes fatty acids from adipose triacylglycerols (in lowered insulin states); no influence on skeletal muscle metabolism because muscle cells lack glucagon receptors Release of insulin from β-cells dictated by level of glucose in blood bathing them; highest levels of insulin occur 30-45 minutes after high-carb meal; return to basal levels about 120 minutes after meal Release of glucagon from α-cells controlled principally through reduction of glucose and/or rise in concentration of insulin in blood bathing the cells; lowest levels after high-carb meal Epinephrine, norepinephrine, and cortisol oppose actions of insulin (counterregulatory hormones) by mobilizing fuels; release mediated by neuronal signals Message of insulin – glucose plentiful and can be used as immediate fuel or can be converted to storage forms of triacylglycerol or glycogen Synthesis and Release of Insulin and Glucagon Islets of Langerhans secrete hormones into hepatic portal vein via pancreatic veins Active form of insulin has A-chain and B-chain linked by 2 interchain disulfide bonds Insulin synthesized as preprohormone that is converted to proinsulin in rER o Proinsulin folds into proper conformation and disulfide bonds formed; transported in microvesicles to Golgi complex, which it leaves in storage vesicles where protease removes C-peptide and few small remnants resulting in formation of biologically active insulin C-peptide Cleavage points Cleavage points o Zinc ions transported in said storage vesicles o Cleavage of C-peptide decreases solubility of insulin, which coprecipitates with zinc o Released by exocytosis Glucose enters β-cell via GLUT2; glucose phosphorylated by glucokinase to become glucose 6-phosphate, which is metabolized through glycolysis, TCA cycle, oxidative phosphorylation o Reactions result in increase in ATP levels in β-cell, causing membrane-bound ATP-dependent K+ channel (K+ATP) to be inhibited, leading to membrane depolarization, which activates voltage-gated Ca2+ that allows Ca2+ to enter cell o Increase in Ca2+ stimulates fusion of insulin containing exocytotic vesicles with PM o Other intracellular metabolites (particularly NADPH) can support insulin release in response to glucose Susceptibility to type 1 DM can be increased by genetic defect in HLA region of β-cells that code for MHC II Rate of insulin release proportional to glucose concentration o As insulin secreted, synthesis of new insulin molecules stimulated so secretion maintained until blood glucose levels fall o Insulin removed from circulation and degraded by liver (to lesser extent kidney and skeletal muscle) Pancreatic islets innervated by ANS (CNS innervation not required for insulin secretion but can cause it) Certain amino acids can stimulate insulin secretion, but to much lower extent than carbs GIP and GLP-1 (gut hormones) released after ingestion of food aid in onset of insulin release Epinephrine secreted in response to fasting, stress, trauma, and vigorous exercise decrease insulin release MODY – results from mutations in either pancreatic glucokinase or specific nuclear transcription factors o MODY type 2 caused by glucokinase mutation that results in reduced activity; because insulin release depends on normal glucose metabolism in β-cell that yields critical ATP/ADP ratio, patients can’t significantly metabolize glucose unless glucose levels higher than normal Patients almost always in hyperglycemic state but somewhat resistant to its long-term complications Neonatal diabetes – newborns develop diabetes in first 3 months of life; may be permanent or transient o Most common mutation causing encodes subunit of K+ATP channel; gain-of-function mutation keeps channel always open; if channel can’t be closed, activation of Ca2+ channel won’t occur, and insulin secretion impaired Glucagon synthesized by cleavage of preporglucagon produced in rER and converted to proglucagon as it enters lumen of ER; proteolytic cleavage produces mature glucagon and GLP-1 and GLP-2 o Glucagon rapidly metabolized, primarily in liver and kidneys o Secretion regulated principally by circulating levels of glucose and insulin (increased glucose or insulin inhibit glucagon release) o Catecholamines and cortisol stimulate glucagon secretion o Many amino acids stimulate glucagon release (can also induce insulin secretion) Insulin release stimulates amino acid uptake by tissues and enhances protein synthesis; because glucagon levels also increase, sufficient glucagon released so gluconeogenesis enhanced at expense of protein synthesis, and amino acids taken up by tissues serve as substrate for gluconeogenesis o Synthesis of glycogen and triglycerides reduced when glucagon levels in blood rise Measuring glucagon levels – only 30-40% of measured amount is mature pancreatic glucagon; rest is larger immunoreactive fragments produced in pancreas or intestinal L-cells Direction of blood flow in islets carries insulin from β-cells in center of islets to peripheral α-cells Sulfonylurea compounds act on K+ATP channels on surface of pancreatic β-cells o K+ATP channels contain pore-forming subunits and regulatory subunits o Binding of drug to sulfonylurea receptor closes K+ channels, which increases Ca2+ movement into cell o Results in release of insulin into circulation Insulin and C-peptide secreted in equal proportions from β-cell, but C-peptide not cleared from blood as rapidly as insulin; C-peptide measurements provide way to estimate degree of endogenous insulin secretion in patients receiving exogenous insulin (lacks C-peptide) Type 2 diabetes patients’ β-cells’ capacity to secrete high levels of insulin declines over time, and patient will require exogenous insulin Mechanisms of Hormone Action Diabetes patients have inappropriately high glucagon levels (resistance to insulin includes α-cells in type 2) 3 basic types of signal transduction for hormones binding to receptors on PM o Receptor coupling to adenylate cyclase (produces cAMP) o Receptor kinase activity o Receptor coupling to hydrolysis of PIP2 Insulin binds to receptor on PM of target cell; receptor has α-subunits to which insulin binds and β-subunits that span membrane and protrude into cytosol o Cytosolic portion of β-subunit has tyrosine kinase activity; autophosphorylated on binding of insulin o Principal substrate for phosphorylation by receptor (IRS-1) recognizes and binds to various signal transduction proteins (SH2 domains); IRS-1 involved in many physiologic responses to insulin Reverses glucagon-stimulated phosphorylation Works through phosphorylation cascade that stimulates phosphorylation of several enzymes Induces and represses synthesis of specific enzymes Acts as growth factor and has general stimulatory effect on protein synthesis Stimulates glucose and amino acid transport into cell o Ability to reverse glucagon-stimulated phosphorylation occurs by lowering cAMP and stimulating phosphatases that could remove phosphates by added PKA During stress of hypoglycemia, ANS stimulates pancreas to secrete glucagon; increased activity of adrenergic nervous system through epinephrine alerts patient to presence of increasingly severe hypoglycemia Glucagon receptor coupled to adenylate cyclase; glucagon (through G-proteins) activates membrane bound adenylate cyclase, increasing synthesis of cAMP, which activates PKA, which changes activity of enzymes by phosphorylating them (either activation or inhibition) o G-proteins couple glucagon receptor to adenylate cyclase; bind GTP and have dissociable subunits that interact with both receptor and adenylate cyclase o In absence of glucagon, Gs-protein complex binds GDP but can’t bind to unoccupied receptor or adenylate cyclase o Once glucagon binds receptor, receptor also binds Gs-complex, which releases GDP and binds GTP o α-subunit dissociates from βγ-subunits and binds to adenylate cyclase, activating it o As GTP on α-subunit hydrolyzed to GDP, subunit dissociates and recomplexes with other subunits o Only continued occupancy of glucagon receptor can keep adenylate cyclase active Hormones that inhibit adenylate cyclase bind to Gi-complex Concentration of cAMP usually very low in cell (rapidly degrades to AMP), so changes in concentration can occur rapidly in response to changes in rate of synthesis; cAMP level not affected by ATP, ADP, or AMP levels in cell o cAMP transmits hormone signal by activating PKA; as cAMP binds to regulatory subunits of PKA, they dissociate from catalytic subunits, which are thereby activated o Activated PKA phosphorylates key regulatory enzymes in pathways of carb and fat metabolism o Message of hormone terminated by action of semispecific protein phosphatases that remove phosphate groups from enzymes; activity of protein phosphatases controlled through hormonal regulation CREs (cAMP response elements) in promoter regions of genes contribute to regulation of gene transcription by several cAMP-coupled hormones o CREB protein directly phosphorylated by PKA (initiates transcription) Inhibition of phosphodiesterase (as by methylxanthine) increases cAMP and has same effects on fuel metabolism as would increase of glucagon and epinephrine; increased fuel mobilization occurs through glycogenolysis and lipolysis (release of fatty acids from triacylglycerols) Signal transduction involves amplification of first message (binding of one molecule of glucagon to one receptor ultimately activates many PKA molecules, each of which phosphorylates hundreds of downstream enzymes) Glucocorticoids and thyroid hormone bind to cytosolic receptors or binding proteins; hormone-binding protein complex moves into nucleus, where it interacts with chromatin; changes rate of gene transcription o Cellular responses to hormones continue as long as target cell exposed to specific hormones o Chronic stress such as seen in prolonged sepsis may lead to varying degrees of glucose intolerance if high levels of epinephrine and cortisol persist o Effects of cortisol on gene transcription usually synergistic to those of other hormones; rates of gene transcription for some enzymes of gluconeogenesis induced by glucagon as well as by cortisol Epinephrine and norepinephrine bind to adrenergic receptors o β-receptors work through adenylate cyclase-cAMP system, activating Gs-protein β1-receptor is major adrenergic receptor in heart and primarily stimulated by norepinephrine; on activation, receptor increases rate of muscle contraction in part because of PKA-mediated phosphorylation of phospholamban β2-receptor present in liver, skeletal muscle, and other tissues; mobilizes fuels (glycogenolysis); mediates vascular, bronchial, and uterine smooth muscle contraction Epinephrine more potent agonist than norepinephrine β3-receptor found predominantly in adipose tissue and to lesser extent in skeletal muscle Activation stimulates fatty acid oxidation and thermogenesis o α1-receptors – postsynaptic receptors; mediate vascular and smooth muscle contraction; work through phospholipase C-β PIP2 system via activation of Gq-protein Mediates glycogenolysis in liver For most type 2 DM patients, site of insulin resistance is after binding of insulin to receptor (normal number and affinity of receptors); binding just doesn’t elicit most of normal intracellular effects of insulin Actions of Insulin Insulin able to antagonize actions of glucagon at level of specific induction or repression of key regulatory enzymes of carb metabolism o Rate of synthesis of mRNA for phosphoenolpyruvate carboxykinase (key enzyme of gluconeogenic pathway) increased by glucagon (via cAMP) and decreased by insulin All of effects of glucagon, even induction of certain enzymes, can be reversed by insulin o Antagonism exerted through IRE in promoter region of genes; causes repression of synthesis General stimulation of protein synthesis by insulin (mitogenic or growth-promoting effects) occur through increase in rates of mRNA translation for broad spectrum of structural proteins o Results in phosphorylation cascade initiated by autophosphorylation of insulin receptor and ending in phosphorylation of subunits of proteins that bind to and inhibit eIFs; when phosphorylated inhibitory proteins released from eIFs, allowing translation of mRNA to be stimulated Activation of insulin receptor mediates internalization of receptor-bound insulin molecules, increasing degradation; unoccupied receptors can be internalized and eventually recycled to PM, but receptor that has been occupied by insulin irreversibly degraded (receptor downregulation)