Surgical Treament for Inflammatory Bowel Disease Over
advertisement

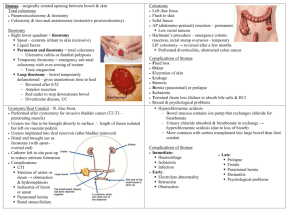
Inflammatory Bowel Disease (IBD): Evolution of Surgical Methods Charles A. Ternent, MD Associate Clinical Professor of Surgery and Director Colorectal Surgery Research, Creighton University School of Medicine, Omaha Nebraska IBD: Surgical Treatment • Indications for Surgery – Elective • • • • Intractability Risk of malignant change Growth retardation Local anorectal complications (fissures, abscesses and fistulas) • Remote or systemic complications (arthritis, skin lesions – pyoderma and erythema nodosum, eye lesions (uveitis, iritis) IBD: Surgical Treatment • Indications for Surgery – Urgent / Emergent • Deterioration patient’s condition (Fulminant colitis) • Local abdominal signs suggestive of perforation • Acute colonic dilatation (Toxic megacolon) – Surgical approach variable over the decades • Ileostomy/cecostomy alone 50% mortality (Crile and Thomas 1951) • Colectomy and ileostomy (Gardner and Miller 1951) – Subtotal colectomy and ileostomy recommended Ulcerative Colitis: Early Surgical Treatment – Operations on the Nervous System (Historical perspective only) • Schlitt 1951: operative division of the pelvic autonomic nerves (permanent sexual and bladder dysfunction) • Levy 1956: prefrontal lobotomy report in 5 patients – “Some” improved Ulcerative Colitis: Early Surgical Treatment • Appendicostomy (Keetly 1895) – Simple procedure intended for very ill colitis patients – Appendix brought up through abdominal wall and catheter passed into cecum and used to irrigate colon – Lockhart-Mummery 1934 reported on 79 cases • 12 deaths, rest “very satisfactory “results but ? cyclical disease factors • Use abandoned circa 1940 in favor of ileostomy Ulcerative Colitis: Early Surgical Treatment • Diverting Ileostomy or Cecostomy with Subsequent Excision of the Large Intestine (Brown 1913) – Adopted in US 1920s-1940s (Strauss 1924, Cattell 1935, Lahey 1941). UK 1940s (Ogilvie 1940) – Rationale: Resting colon to allow quiescence and possible reversal of stoma – Cattell 1948 reported ileostomy invariably permanent and colectomy required due to failure of recovery or because of cancer risk Ulcerative Colitis: Early Surgical Treatment • Diverting Ileostomy with Excision of the Large Intestine (Proctocolectomy) in Stages – Gabriel 1952 reported three-stage procedure in 3-month intervals • Ileostomy (initially affected bowel left in place) • Subtotal colectomy with exteriorization sigmoid colon • Abdominoperineal resection rectosigmoid colon – Additive morbidity and mortality from serial operations (not an efficient approach with present day anesthesia) Ulcerative Colitis: Early Surgical Treatment • Ileostomy with Immediate Subtotal Colectomy or Proctocolectomy (Miller 1949 and Crile and Thompson 1951) – Rationale: Minimize toxicity of septic colon left in place especially in more toxic cases – Concern: Increased mortality in toxic patients and increased morbidity from proctectomy in patients on high dose steroids and biologic agents • Toxic/compromised physiology – subtotal colectomy with ileostomy • Elective refractory – proctocolectomy with ileostomy Ulcerative Colitis Early Surgical Treatment: Colectomy with Ileostomy Early Studies of Urgent/Emergent Colectomy for UC Mortality Urgent / Emergent Mortality Elective N Urgent / Emergent Lennard-Jones 1960 31% 4.4% 32 Brooke and Sampson 1964 16% 6% 62 Goligher 1970 14% 3% 184 Ulcerative Colitis: Early Surgical Treatment • Techniques of Ileostomy • Initially ileostomy brought out 5 cm or so straight and allowed serosal surface to granulate (no eversion) • Commonly resulted in fibrosis, stenosis and partial obstruction or ileostomy dysfunction (Counsell and Goligher 1952) • Dragsted 1941 skin grafted serosal surface ileostomy above skin level – contraction and stenosis still a problem Ulcerative Colitis: Early Surgical Treatment • Techniques of Stoma Creation – Patey 1951 advocated immediate suture of stoma bowel to skin (flat stoma a problem with ileostomy) – Brooke 1952 adopted immediate mucocutaneous suture in constructing ileostomies with evertion of the last 1-2 cm of ileal wall to create projection (standard of care today) – Turnball 1953 would strip the terminal ileal portion of serosa and muscularis before eversion (technically difficult and without significant advantage) Ileostomy Appliances • Incontinent stomas require constant wearing of an appliance (early on a bag or box) • Koenig 1944 patient of Strauss in Chicago developed the adherent ileostomy bag along with Rutzen – Water tight and leak resistant arrangement • Turnbull 1975 introduced karaya gum powder to minimize leakage – Paste or wafer has soothing and efficient adhesive • Stomahesive paste further enhanced stoma care Ulcerative Colitis: Early Surgical Treatment • Continent – Reservoir Ileostomy (Koch 1969 Goteburg, Sweden) • Internal pouch created out of 45-50 cm of ileum immediately above stoma • Continent valve requires intubation through abdominal wall to evacuate • No stoma appliance required. Cover with gauze • Valve can slip and leak and complication and revision rates high Ulcerative Colitis: Early Surgical Treatment • Diverting Transverse or Left Sided Colostomy after distal proctocolectomy – Possible in very distal disease – High incidence of extending disease to involve proximal colon – Staghlgren and Ferguson 1959 reported on 18 patients with this procedure. 11 required completion colectomy and ileostomy Ulcerative Colitis: Early Surgical Treatment • Colectomy with Ileosigmoid (Lilienthal 1903, Devine 1943,1948) – Extraperitoneal technique – Gabriel 1952 reported that 4/5 required separation of anastomosis and ileostomy • Ileorectal Anastomosis (Aylett 1953-1963) – End to end ileorectal anastomosis with protecting loop ileostomy for 3 weeks • FU 1963 N=123, 5% mortality, 13% conversion to ileostomy Ulcerative Colitis Early Surgical Treatment Ileorectal Anastomosis • Jagelman 1953 Postal inquiry of 200 of Aylett’s patients • 25% had 6 or more stools per day • 90% considered surgery successful • Literature 1954-1977 (Goligher, Wangensteen…) – 20-50% failure rate requiring ileostomy – 7/350 patients followed 10-15 years developed carcinoma – Goligher: reserve for patients with lesser degrees of rectal involvement who are not interested in rectal excision or stoma – Currently mainly considered in mild rectal disease, indeterminate colitis, high risk or older patients not good candidates for IPAA Ulcerative Colitis: Early Surgical Treatment • Colectomy and Partial Rectal Excision with Ileoanal Pull-Through (Ravitch 1948) – Anal mucosectomy and straight ileoanal anastomosis – Others found great frequency of defecation and incontinence (Goligher 1951, Wangenstein 1948) – 7-8+ BMs per day – Goligher 1980: More promising proposition would be an ileoanal reservoir… Ulcerative Colitis: Modern Surgical Treatment • Proctocolectomy with Ileoanal Pouch Anal Anastomosis (IPAA) – IPAA and protecting ileostomy • Ferrari and Fonkalsrud 1978 report of successful operation • Parks and Nichols 1978 report of 5 patients with colitis treated with IPAA with encouraging results Ulcerative Colitis: Modern Surgical Treatment • Quality of life / functional issues: Proctocolectomy with permanent ileostomy vs IPAA – IPAA was associated with a significantly better perception of body image than a permanent stoma – Quality of life in general was similar in both groups – Patients with a pouch had more long-term complications than patients with an ileostomy within the same period of time (52.6% vs. 26.3%) – The median number of stages for pouch construction was two, compared to a median of one stage for an ileostomy (P<0.0001). – Counsel thoroughly preoperatively J Clin Gastroenterol. 2006 Sep;40(8):669-77. Quality of life after proctocolectomy with ileoanal anastomosis for patients with ulcerative colitis.Lichtenstein GR1, Cohen R, Yamashita B, Diamond RH Ulcerative Colitis: Modern Surgical Treatment • Restorative Proctocolectomy and IPAA • One, two or three stages? – High dose steroids / biologics, urgent/emergent surgery increase risk of infection (3 stage) – No high risk of infection (2 stage) – No steroids or biologics and elective (possible 1 stage in some centers but potential drawbacks/risks) Ulcerative Colitis: Modern Surgical Treatment • Laparoscopic approaches to Proctocolectomy with permanent ileostomy and IPAA • Is there a benefit to minimally invasive techniques? – Less blood loss – Diminished postop pain – Reduced narcotic requirement – Shorter hospital stays Ulcerative Colitis: Modern Postoperative Issues • Pouchitis after IPAA for UC – Most common long-term complication (25%) – Usually responds to PO antibiotics (Cipro/Flagyl) – 60% second episode – 20% chronic pouchitis (chronic maintenance therapy – combination therapy and Rifaximin) – Budesonide and Biologics (Infliximab), VSL-3 (probiotic) – May need pouch revision or excision Ulcerative Colitis: Modern Postoperative Issues • Crohn’s disease (CD) and IPAA: Outcomes – One of most common long-term inflammatory complications – Leading cause of pouch failure (10% if CD known preop and carefully selected / 50% if CD develops postop) – Treatment • • • • Topical / oral mesalamine or steroids Antibiotics Immunomodulators Biologics may be considered in refractory disease of IPAA particularly if extra-intestinal symptoms • Consider pouch excision - revision Crohn’s Disease: Early Reports • Non-specific enteritis descriptions – Moynahan 1907, Mayo-Robson 1908, Leeds and Dalziel 1913 – Burrill Crohn NY 1932 established the clinical and pathologic entity of regional or granulomatous enteritis • Anywhere in GI tract • Skip lesions Crohn’s Landmark Paper Crohn’s Disease: Evolution of Surgical Treatment • • • • • • Diverting stoma Bypass with or without exclusion Resection with stoma Resection with anastomosis +/- stoma Stricturoplasty +/- resection Radical vs conservative resection of bowel and mesentery (resect to grossly not microscopically normal tissue) Crohn’s Disease: Early Surgical Treatment • Bypass with exclusion advocated in mid 1930s (Mount Sinai Hospital, NY) • President Eisenhower had successful bypass without exclusion for Crohn’s (Heaton et al 1964) • Surgical resection popularized with increasing safety of surgery (Glotzer and Siren 1971) • Clear indication for bypass operation alone is duodenal Crohn’s (Fielding et al 1970) Crohn’s Disease and Fistula-in-Ano • Fistula Definition – Abnormal communication/tract between any two epithelium lined surfaces – Presence of a rectal or anal internal opening • Etiology – Most common result of cryptoglandular infections – IBD/Crohn’s, Infectious, Cancer, HIV and other immunocompromised states MRI Complex Anterior Fistula-in -Ano Classification of Anal Fistulas Anal Fistula in Ancient Greece Hippocrates (ca. 460-370 BC) • Aware of anorectal fistulas and tried to interpret mechanism of origin (first description) • Attempted to treat them conservatively using laxatives and purgative medications or surgically via anoscope • Understood importance of the surgical option but lacked appropriate tools • Numerous operations exist • Aim to decrease recurrence and incontinence rates Louis 14th 17th Century France • Had anal fistula in 1686 at age 47 after developing an abscess in the “Foundation” from riding horses • Recurrent abscesses made it impossible for the King to walk • Surgery as we know it today did not exist • Difficult for the King to adopt majestic airs Francois Felix: A Great BarberSurgeon and The Royal Anus • Born in Avignon c 1635 • Developed technique to perform an operation on the monarch after practicing with peasants/prisoners at King’s request • Found that addressing the internal fistula opening was key to the operation while preserving life and anal sphincter continence Francois Felix: A Great BarberSurgeon and The Royal Anus • SETON One or more threads or horsehairs or a strip of linen introduced beneath the skin by a knife or needle to provide drainage or to produce or prolong inflammation Francois Felix: A Great BarberSurgeon and The Royal Anus • The King required 4 operations for healing of fistula (staged fistulotomies with setons) • Back to riding horses by 3 months • Felix was knighted, bought a town (Tassy) and asked that the barber trade be separated from surgery • Became the surgeon of the Sun King • Had PTSD from ordeal and apparently was not able to touch a scalpel thereafter • Helped to establish the French Royal Academy of Surgery in 1731 under King Louis XV Crohn’s Disease: Anorectal Fistula Modern Surgical/Medical Treatment • Drain abscess if present • Drain fistulas with setons to minimize festering and abscess recurrence as immunomodulator and biologic agents started • As fistula tracts dry up and therapy effective can remove setons (may have to replace and re-drain depending on CD activity Crohn’s Disease: Modern Surgical Treatment • Fissure – Pain and bleeding can be excruciating and may be main complaints of CD – May be atypical, lateral or associated with edematous skin tags (CD) – Maximize medical management when active disease related fissures and symptoms usually improve – Surgery only if not CD related and no active CD and anal sphincter hypertonic IBD: Modern Surgical Treatment • Timing of Surgery: Immunomodulator Biologic and Steroid Therapy – Ulcerative Colitis: high dose steroids and biologics increase infection risk – stage colectomies – Crohn’s Disease: literature on biologics controversial – time surgery around biologic dose to maintain optimized medical management. Steroids and biologic combinations increase risk of infection IBD Surgery Conclusions • Extensive progress over last 100+ years • Future: Genotype-phenotype correlations may help guide surgery and medical therapy • Continued improved medical management will continue to compliment evolving surgical techniques and capabilities • The Cure…