Vital Signs

Temperature (T)
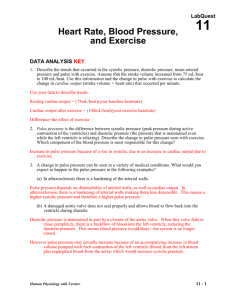
Pulse (P)
Respiration (R)
Blood pressure (BP)
Pain (often called the fifth vital sign)
Oxygen Saturation
Upon admission to a healthcare setting
When certain medications are given
Before and after diagnostic and surgical procedures
Before and after certain nursing interventions
In emergency situations
Definition: the heat of the body measured in degrees
›
›
The difference between production of heat and loss of heat
Normal temperature: 97.0ºF (36.0ºC) to 99.5ºF
(37.5ºC)
Process: heat is generated by metabolic processes in the core tissues of the body, transferred to the skin surface by the circulating blood, and dissipated to the environment
Core temperatures
› Tympanic and rectal
› Esophagus and pulmonary (invasive monitoring devices)
Surface body temperatures
› Oral (sublingual)
› Axillary
Oral: impaired cognitive functioning, inability to close lips around thermometer, diseases of the oral cavity, and oral or nasal surgery
Rectal: newborns, small children, patients who have had rectal surgery, or have diarrhea or disease of the rectum, and certain heart conditions
Tympanic: earache, ear drainage, and scarred tympanic membrane
Pulse rate
› Measured in beats per minute
Pulse quality (amplitude)
› The quality of the pulse in terms of its fullness
Pulse rhythm
› Pattern of the pulsations and the pauses between them
Normally regular
Palpating the peripheral arteries
Auscultating the apical pulse with a stethoscope
Using a portable Doppler ultrasound
Temporal
Carotid
Brachial
Radial
Femoral
Popliteal
Posterior tibial
Dorsalis pedis
Indications
›
›
Patient is receiving medications that alter heart rate and rhythm
A peripheral pulse is difficult to assess accurately because it is irregular, feeble, or extremely rapid
Method
›
›
Count the apical rate 1 full minute by listening with a stethoscope over the apex of the heart
Most reliable method for infants and small children; can be palpated with fingertips
Rate
› Adults: 12 to 20 times per minute
› Infants and children breathe more rapidly
Depth
› Varies from shallow to deep
Rhythm
› Regular: each inhalation/exhalation and the pauses between occur at regular intervals
Method
› Inspection (observing and listening)
›
›
Listening with the stethoscope
Counting the number of breaths per minute
Considerations
›
›
If respirations are very shallow and difficult to detect visually, observe sternal notch
Patients should be unaware of the respiratory assessment to prevent altered breathing patterns
Exercise
Medications
Smoking
Chronic illness or conditions
Neurologic injury
Pain
Anxiety
Retractions
Nasal flaring
Grunting
Orthopnea (breathing more easily in an upright position)
Tachypnea (rapid respirations)
Ineffective Breathing Pattern
Impaired Gas Exchange
Risk for Activity Intolerance
Ineffective Airway Clearance
Excess Fluid Volume
Ineffective Tissue Perfusion
Definition
› The force of the blood against arterial walls
Systolic pressure
› The highest point of pressure on arterial walls when the ventricles contract
Diastolic pressure
› The lowest pressure present on arterial walls during diastole (Taylor, 2007).
Blood pressure is measured in millimeters of mercury (mm Hg)
Blood pressure is recorded as a fraction
› The numerator is the systolic pressure
› The denominator is the diastolic pressure
Pulse pressure
› The difference between the systolic and diastolic pressure
Using a stethoscope and sphygmomanometer
Using a Doppler ultrasound
Estimating by palpation
Assessing with electronic or automated devices
Use a cuff that is the correct size for the patient
Ensure correct limb placement
Use recommended deflation rate
Correctly interpret the sounds heard
Age
Exercise
Position
Weight
Fluid balance
Smoking
Medications
Purpose
› Measure the arterial oxyhemoglobin saturation of arterial blood
Method
› A sensor or probe, uses a beam of red and infrared light which travels through tissue and blood vessels
›
›
The oximeter calculates the amount of light absorbed by arterial blood
Oxygen saturation is determined by the amount of each light absorbed
Monitoring patients receiving oxygen therapy
Titrating oxygen therapy
Monitoring those at risk for hypoxia
Monitoring postoperative patients