AP immune
advertisement

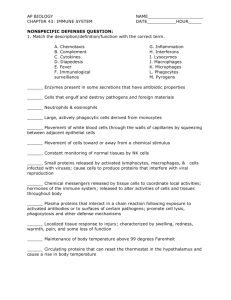
Immunity Chapter 39 Innate vs Acquired -All animals have innate systems, only vertebrates have acquired (we will look at mammal aquired) -acquired develops over a lifetime and is specific Three Lines of Defense • Barriers at body surfaces (which technically is nonspecific) • Nonspecific responses • Immune responses - specific I. Surface Barriers – 1st line of defense A. skin i. pathogens can’t get through, not good conditions for growth of pathogens (low moisture, low pH and thick layer of dead cells) and harmless bacteria present - pathogens can’t compete B. Mucous membranes i. Sticky, helpful bacteria found here, chemicals (like lysozyme that digest cell wall of bacteria) are present C. lungs i. air rushes in and flings pathogens into mucus coated walls, chemicals (like lysozyme, digest cell wall of bacteria), and cilia to move pathogens out D. flushing effect – most of these fluids also contain chemical like lysozyme or have a non-neutral pH i. tears, saliva, gastric fluid, urine, etc The first line of defense in the respriratory tract (trachea). The orange cells produce mucus that that traps micro-organisms that enter. The yellow cells are cilliated which beat in unison to expel mucus and trapped microorganisms upward to pharynx. Nonspecific Responses • Lymph nodes trap and kill pathogens • Natural killer cells attack a range of targets • Inflammation • Complement proteins Acute Inflammation • Nonspecific response to foreign invasion, tissue damage, or both • Destroys invaders, removes debris, and prepares area for healing • Characterized by redness, swelling, warmth, and pain (see chart, page 690) – Caused by the release of histamine from mast cells which triggers vasodilation and capillary permeability Inflammation • • • • Mast cells and basophils release histamine Capillaries dilate and leak Complement proteins attack bacteria White cells attack invaders and clean up Figure 39.5 Page 691 The Inflammatory Response Complement System • Plasma proteins that take part in both specific and nonspecific response • Activation of one triggers cascade of reactions that activate others • some insert into plasma membranes of pathogens and initiate lysis • some promote inflammation • some form concentration gradients that phagocytic white blood cells follow • some bind to the surface of invaders, marking them for phagocytosis 3. Complement proteins(approx. 20-30 proteins) a.) Directly- form protein rings on bacteria membranes forming pores, water rushes in, bursts cells b.) Indirectly- The complement protein coats the surface bacteria. There are recognition sites on the phaggocytes that bind with proteins coating the bacteria. The phagocytes engulf the bacteria in a process called opsonization- Features of Specific Immune Responses • self/nonself recognition – B and T cells ignore the bodies own cells, self markers on the organisms own cells • specificity – B and T cells attack specific foreign agents • diversity - B and T cell receptors have the potential to respond to a billion specific threats • memory – a portion of B and T cells are set aside for future battles with specific agent Cells of the Immune System • B-lymphocytes – Carry out the humoral immune response – Circulate in body fluids – Mature in the bone marrow • T-lymphocytes – Carry out the cell-mediated immune response – Guards against invaders within the cell – Mature in the thymus Antigens • “Nonself” markers on foreign agents and altered body cells such as tumors • Trigger division of B and T cells • When a B or T cell is stimulated to divide, it produces more than one cell type • Memory cells - set aside for future use • Effector cells - engage and destroy the current threat Steps in Immune Response • Recognition of an antigen • Rounds of cell division that form huge populations of lymphocytes • Specialization of lymphocytes into effector and memory cells that have receptors for one kind of antigen • 2 types of responses – Antibody mediated – extracellular targets, B cell – Cell mediated – intracellular or altered body cell targets, cytotoxic T cells • Both are triggered by helper T cells Lymphocyte Battlegrounds • Lymph nodes filter antigens from body fluids • Macrophages, dendritic cells, B and T cells in nodes and spleen mount a defense Humoral and Cell-Mediated Immunity • Humoral Immunity – Antibodies circulate as soluble proteins in blood plasma and lymph – Defend against toxins, free bacteria, viruses in body fluids • Cell-mediated Immunity – White blood cells are active against bacteria and viruses inside the host’s cells and against fungi, protozoa, and worms Antibody-Mediated Response • Carried out by B cells • Targets are extracellular pathogens and toxins • Antibodies bind to target and mark it for destruction by phagocytes and complement Antibody-Mediated Response • B cell becomes antigen-presenting cell • Helper T cell binds to antigen-MHC complex • Interleukins stimulate B cell division and differentiation • Effector cells secrete antibodies antigen naïve B cell Figure 39.14 Page 697 MHC molecule antigenMHC complex helper T cell antigenpresenting B cell interleukins memory B cell antibody effector B cell Antibodies are proteins made of 4 polypeptides. 2 identical, heavy, polypeptide chains and 2 identical, light polypeptide chains. A light chain is bonded to a heavy chain by disulfide bonds. Five Different Classes of AB -IgG- monomer- found late in response crosses placenta -IgA- Dimer and monomer form -IgM- pentamermonomer form helps with virgin B cells -IgD- monomers found surface B cells -IgE- monomer found in area with connective tissue helps with release histamine Cell-Mediated Response one macrophage another macrophage • Carried out by T cells • Stimulated by antigenpresenting macrophages • Main target is antigenpresenting body cells (cells with intracellular pathogens) or tumor cells interleukins cytotoxic interleukins T cell helper T cell infected body cell Figure 39.15 Page 698 Recognition Each of us are unique because of differences on surface proteins. Chromosome 6 (Major Histocompata-bility Complex or MHC genes) has several hundred genes that code for these surface proteins or MHC proteins (classes I &II) There are 3 major groups of MHC proteins Class I, II, and III: Class I MHC proteins are on all cells Class II MHC proteins are found on 1. macrophages, 2. B cells ,3. T cells Class III MHC proteins form the complement proteins During fetal development cells will be labeled Class I and/or Class II proteinsthe MHC proteins act like a badge to identify you as you. These MHC proteins makes sure that your immune system does not attack you. Role of T cells T- have two receptor sites one for the MHC protein and one for an AG During development T-cells get their MHC recognition site- must match the body's own MHC proteins. If they do not make a match they die. If they do, they become MHC restricted. Now, if recognition site matches a Class I protein (found on all cells) the T- cell becomes cytotoxic (killer) cell. If recognition site matches a Class II protein (T cells or macrophage), the Tcell will become a helper-T-cell. These cells are MHC restricted and are called virgin-T-cells. Clonal Selection • Each antigen, by binding to specific receptors, selectively activates a tiny fraction of cells from the body’s diverse pool of lymphocytes • This relatively small number of selected cells gives rise to a clone of millions of effector cells, all dedicated to eliminating the specific antigen that stimulated the immune response Clonal Selection Colonal selection works 2 ways I. Arousal of T cells II. Direct arousal of B cells by AG I. Arousal of T cells 1. Macrophages(have both MHCI and MCHII proteins) 2. Macrophage goes to the site of infection 3. The macrophage devours virus, AG, or bacteria and the macrophage then puts bits and pieces of invader on cell membrane(assoc. w/MHCI and MHCII proteins) Now the macrophage goes to the virgin Tcells looking for a match between the the MHC receptor and antigen receptor on the Tcell and the MCH protein and antigen on the macrophage. When the macrophage binds with virgin Tcell a substance called interluken is secreted. Interluken causes T-cells to reproduce making either cytotoxic T-cells, T-memory cells, or helper T-cells. Activated cytotoxic cells go around frisking cells with its dual receptor site. If cell is healthy, then it will only have MHCI protein on surface, and the cytotoxic cell will ignore it, going on its way. However, if cell is infected, the cell will have bits of AG on its surface with the MHCI receptor site. The cytotoxic T cell will put holes in infected cells water rushes in and kills the cell. The cell dies and phagocytes appear to clean up mess. *Cytotoxic cells also kill cancer cells because cancer cells change and have new surface proteins. Every once in a while the cells will escape the cytotoxic-T-cell because the MHCI protein has also changed *There is no longer a dual match and cells replicate or metastisize A cytotoxic cell (orange) destroying a cancer cell (purple). II. Arousal of B cells and antibody formation. Activated helper-T- cells act much like the macrophage did in activating virgin B cells 1. Virgin B cells has AB on surface. It captures free floating AG. 2. The B-cell puts AG next to MHCII protein. 3. Helper-T-cell with its MCH II recognition site and antigen recognition site finds B-cell with AG and MHCII protein 4. The two join and the helper-T-cell secretes interleuken. This causes the B-cell to reproduce. 5. The B-cells fall into 2 types a. Memory-B-cells for the secondary immune response b. Plasma cells which will produce REMEMBER WHAT ANTIBODIES CAN DO!!!!!!!!!!!!!!!!!!!!!!!!!! They are AG specific. *AB 1. Bind to several AG 2. Can trigger complement holes in the cell 3. Opsonization - to increase the susceptibility of (bacteria) to ingestion by phagocytes. monoclonal antibody antibody produced by a laboratory-grown cell clone, either of a hybridoma (a hybrid cell made in the laboratory by fusing a normal cell with a cancer cell) or a virus-transformed lymphocyte, that is more abundant and uniform than natural antibody and is able to bind specifically to a single site on almost any chosen antigen or reveal previously unknown antigen sites: used as an analytic tool in scientific research and medical diagnosis and potentially important in the treatment of certain diseases. Abbreviation: Mab Immunization • Process that promotes immunity • Active immunization – Antigen-containing material is injected – Confers long-lasting immunity • Passive - – Purified antibody is injected – Protection is short lived •Allergies A. a normally harmless substances provoke inflammation, excess mucus secretion and sometimes and immune reponse •Disorders A. Autoimmune – self-recognition fails and the immune system attacks it own body components B. Deficient Immune Response – loss of immune function i. primary – present at birth, due to altered genes or abnormal development ii. secondary – loss of immune function following exposure to outside agents (AIDS) -AIDS/HIV – attacks helper T cells A T-cell being infected by the aids virus (blue particles) -nonspecific -Barriers movie -2nd line of defense (part a) -2nd line of defense (part b) -specific defense -3rd line part a -3rd line part b -3rd line part c -3rd line part d -cell mediated response animation -humoral (antibody) response