Immunology overview notes
advertisement

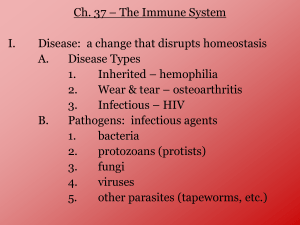
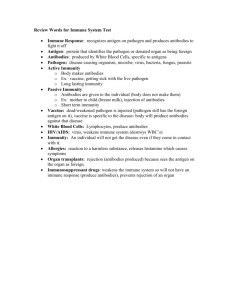
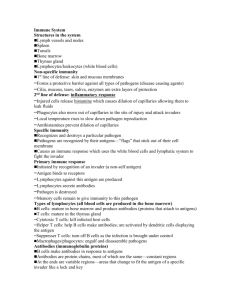
KEY CONCEPT The immune systems consists of organs, cells, and molecules that fight infections. Immunology- Three lines of defense Barriers, Nonspecific responses, specific-targeted response First line of defense-Barriers Physical and chemical barriers Nonspecific-doesn’t distinguish, same for all invaders Skin-outer layer of tough,dead cells Mechanical barrier Constantly shedding Bacteria can’t enter. Sweat and oil glands- chemical barrier secrete acids Sweat has lysozyme- breaks down cell walls. Barriers continued Mucous membranes Mechanical barrier Mucous traps pathogens Cilia moves trapped particles out of body Secretions Saliva and tears washing action Lysozyme enzymes breaks down cell walls. Stomach acids, enzymes Destroy pathogens Microorganisms in foods,drinks Second line of defense Nonspecific- doesn’t single out a specific pathogen. When pathogens get through primary first line of defense. Includes Pathogen destroying white blood cells Inflammatory response Specialized proteins White Blood Cells-wbcs bloodstream, interstitial fluid, and lymphatic system attacking invaders Macrophages ( big eaters) mainly in interstitial fluid. macrophage engulfs the organism. the pathogen is drawn into the macrophage, where enzymes such as lysozyme kill the pathogen. Neutrophiles-smaller and more numerous 60-70% of wbcs. Multilobed- PMNs Neutrophils also kill by phagocytosis neutrophil releases chemicals - kill the invading pathogen. Chemicals also kill the neutrophil. White blood cells can identify certain proteins and carbohydrates on the surface of an invading pathogen. These "foreign" molecules triggers the cells' responses. Pus- fluid containing wbcs and debri from dead tissue Natural killer cell (NK) Do not kill pathogens directly Recognize body cells that have become infected by a virus Release chemicals to break infected cell’s membrane Also attack cancer cells/ abnormal cells before a tumor is formed. Inflammatory Response Nonspecific defense characterized by 6 characteristics redness, heat, swelling, pain, fever phagocytosis. mast cells release histamine nearby blood vessels to dilate (expand). Increases the volume of blood flowing to the injured tissue. Other chemicals attract additional phagocytes and other white blood cells to the area, where they pass through the leaky blood vessel walls into the interstitial fluid Local increase of blood flow, fluid, and white blood cells produces the redness, heat, swelling, and pain at the injured area. In fever, body temperature increases. – Low fevers stimulate white blood cells to mature. – High fevers can cause seizure, brain damage, and even death. During an inflammatory response, chemical signals trigger changes in blood vessels and attract white blood cells that help destroy the invaders. Specialized Proteins Interferon a family of proteins produced by T-cells or virusinfected cells. The infected cell may die, but its interferon reaches healthy cells in the area, stimulating them to produce proteins that interfere with virus reproduction. Interferon is effective against many viruses and is therefore nonspecific. Interferon seems to be effective against viruses that cause the flu and the common cold. Genetically engineered Infected cells produce interferon, which stimulates non-infected cells to manufacture substances that block virus reproduction. Third line of defense Immune system Specific Recognizes specific pathogens, cancer cells,certain chemicals Immune system must recognize self from nonself. Cells of the immune system produce specific responses. Specific immune responses begin with the detection of antigens. Antigens are surface proteins on pathogens. Means antibody generating. Each pathogen has a different antigen. antigens virus There are two specific immune responses. 1. Humoral immunity - B cells to produce antibodies. antibodies B cell pathogen T cell memory B cells activated B cells 2. Cellular immunity -T cells -destroys infected body cells. pathogen antigens antigens T cell receptors memory T cells activated T cells Both responses produce memory cells. B cell T cell – specialized T and B cells – provide acquired (active) immunity Immunity Resistance to a pathogen that causes disease. Antigens- large molecules of protein or polysaccharides that induce a specific response. Rarely can be lipids or nucleic acids Small molecules are poor antigens They are not attracted to macrophages. Examples of antigens Bacterial capsules Lipopolysaccharides of gram neg. bacteria Glycoproteins in cell membranes Attachment sites on viruses that interact with mammalian cells. Soluble bacterial toxins,venoms Pollens, food, house dust Properties of antigens Foreign to host Capable of inducing an antibody response Large Antibody must bind to the antigen Epitope- Specific location on antigen that combines with antibody Hapten- if molecule is too small to induce an antibody response by itself it combines with a carrier molecule (protein). Ex. penicillin Antibodies Antibodies- proteins found on the surface of certain white blood cells, or in blood plasma, that attach to particular antigens. Also known as immunoglobulins- Ig Specific B-Cell Receptor: Immunoglobulin Composed of 4 polypeptide chains: Y shaped arrangement – 2 identical heavy chains (H) 2 identical light chains (L) ends of the forks formed by light and heavy chains contain a wide range of variable antigen binding sites Variable regions Constant regions T-Cell Receptors for Antigen Formed by genetic recombination, with variable and constant regions 2 parallel polypeptide chains small, without humoral functions Classes of Immunoglobulins 5 classes of Immunoglobulins (Ig): 1. IgG - long term immunity- crosses placenta 2. IgA – secretory antibody- mucous 3. IgM – immediate response 4. IgD – receptor on B cells 5. IgE – allergic response Classes of Antibodies(Ab) IgG 2 antigen binding sites Crosses placenta 80% of all immunoglobulins IgM 5 or more binding sites Largest Found in plasma 1st Ab after injection of antigen Especially effective against gram negative bacteria Immunity Titers IgA IgD Secretions of exocrine glands- mother’s milk Saliva, tears Effective against bacteria and viruses 2 sites On B cells that recognizes antigens Function difficult to determine IgE Least amount In allergic reactions Allergen- IgE- mast cells- histamine. Lymphocytes Lymphocytes- special wbcs that recognize specific invaders. In bone marrow, lymphocytic stem cells differentiate into either T or B lymphocytic cells. B cells mature in the bone marrow B- bursa of birds T cells migrate to thymus gland to mature. Mature T and B cells migrate to lymph nodes and other parts of the lymphatic system. All lymphocytes begin development in the bone marrow. B cells complete their development there (think "B for bone"). T cells are transported to the thymus gland where they mature (think "T for thymus"). B Cells and Humoral Immunity Antibody proteins on the surface of B cells act as specific receptors for antigens. ~ 100 million different B cell surfaces B Cells act primarily against bacteria and viruses in body fluids outside of cells. Humoral Immunity Figure 31-12 A particular type of antigen activates a specific B cell. The activated B cell produces a clone of millions of plasma cells that produce antibodies to the specific antigen. Steps: Activation occurs: B cell with matching antigen receptor binds to the antigens of the pathogen. B cell grows and clones itself, forming millions of identical cells. Each cell can become a plasma cell, which produces and secretes antibodies specific to the original antigen that activated the original B cell. Plasma cells are carried by lymph and blood to sites of infection in the body. Termed humoral immunity since antibodies travel in the blood and other body fluids once called “humors”. T cells and Cell-Mediated Immunity T cells directly attack infected host cells that contain bacteria or viruses. Each T cell has a receptor for a specific antigen. Steps: 1. The infecting pathogen’s antigens are displayed on the host body cell. 2. Activation occurs- the antigens on the host body cell bind to receptors on the matching T cell, activating the T cell. 3. Activated T cell divides producing clones. 4. T cell clones become cytotoxic T cells- 5. Cytotoxic T cells attack infected cells. bind to infected cell membranes secrete perforin - pokes holes in the membrane-leakage and cell death. Macrophages display the antigens of pathogens they have "eaten." This display activates a specific version of helper T cells. The activated helper T cells in turn stimulate cytotoxic T cells and B cells. Role of Helper T Cells Role in both humoral and cellular immunity. Helper T cells are activated by binding to macrophages that display antigens of a pathogen. Helper T cells then secrete chemicals that activate both cytotoxic T cells and B cells How the Immune System Remembers Pathogens Memory B and T cells The first formation of T and B cells is called the primary immune response. After the first exposure of a pathogen some of the B and T cells remain in your body. A slower and weaker response- requires time Second exposure to the same pathogenSecondary immune response. Quicker and stronger response- don’t develop symptoms Memory T cells produce cytotoxic T cells Memory B cells produce plasma cells that secrete Ab Passive and Active Immunity Passive immunity- receive antibodies from another source Antibodies to fetus from mother. Travelers receive antibodies rather than antigens. hepatitis A Lasts a short time- weeks or months Active Immunity- your body produces antibodies Get disease. Vaccines Heat killed dose of pathogen (antigen) Attenuated (very low, nonvirulent) dose of pathogen Booster shot- tetanus- additional dose of antigenneeded because initial memory cells have died A vaccine stimulates the production of antibodies and memory cells that protect against future exposure to the pathogen.