The Immune Response
advertisement

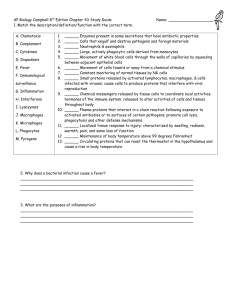
The immune response Anca Bacârea, Alexandru Schiopu The importance of immune system The immune system is clearly essential for survival. It constantly defends the body against bacteria, viruses, and other foreign substances it encounters. It also detects and responds to abnormal cells and molecules that periodically develop in the body so that diseases such as cancers do not occur. An essential aspect of the immune response is the ability to recognize almost limitless numbers of foreign cells and nonself substances, distinguishing them from self molecules that are native to the body – it distinguishes self from nonself. Definitions The immune system consists of the central and peripheral lymphoid tissues. The individual components of the substance that the immune system recognizes as foreign are called antigens. The interaction of the collective and coordinated components of the immune system and the antigens of a foreign agent is called the immune response. The immune system The central lymphoid organs the bone marrow and the thymus provide the environment for immune cell production and maturation The peripheral lymphoid organs Lymph nodes, spleen, tonsils, appendix, Peyer’s patches in the intestine, and mucosaassociated lymphoid tissues in the respiratory, gastrointestinal, and reproductive systems function to trap and process antigen and promote its interaction with mature immune cells The immune system - classification The immune system Nonspecific or innate defense system Cellular Humoral Specific or acquired immune system Cellular Humoral Nonspecific or innate defense system First line of defense system It distinguishes self from non-self but does not distinguish one type of pathogen from another. Components: skin and mucous membranes inflammatory response phagocytic and non phagocytic leukocytes cells Nonspecific defense system 1. Mechanical factors The epithelial surfaces form a physical barrier that is very impermeable to most infectious agents. The skin acts as our first line of defense against invading organisms. The desquamation of skin epithelium also helps remove bacteria and other infectious agents that have adhered to the epithelial surfaces. Movement due to cilia or peristalsis helps to keep air passages and the gastrointestinal tract free from microorganisms. The flushing action of tears and saliva helps prevent infection of the eyes and mouth. The trapping effect of mucus that lines the respiratory and gastrointestinal tract helps protect the lungs and digestive systems from infection. Nonspecific defense system 2. Chemical factors Fatty acids in sweat inhibit the growth of bacteria. Lysozyme and phospholipase found in tears, saliva and nasal secretions can breakdown the cell wall of bacteria and destabilize bacterial membranes. The low pH of sweat and gastric secretions prevents growth of bacteria. Defensins (low molecular weight proteins) found in the lung and gastrointestinal tract have antimicrobial activity. Surfactants in the lung act as opsonins (substances that promote phagocytosis of particles by phagocytic cells). 3. Biological factors The normal flora of the skin and in the gastrointestinal tract can prevent the colonization of pathogenic bacteria by secreting toxic substances or by competing with pathogenic bacteria for nutrients or attachment to cell surfaces. Nonspecific defense system The anatomical barriers are very effective in preventing colonization of tissues by microorganisms. However, when there is damage to tissues the anatomical barriers are breached and infection may occur. Once infectious agents have penetrated tissues, another innate defense mechanism comes into play, namely acute inflammation. Humoral factors play an important role in inflammation, which is characterized by edema and the recruitment of phagocytic cells. Nonspecific humoral immune system The complement system The complement system is a primary mediator of the humoral immune response that enables the body to produce an inflammatory response, lyse foreign cells, and increase phagocytosis. The complement system, like the blood coagulation system, consists of a group of proteins that normally are present in the circulation as functionally inactive precursors. These proteins make up 10% to 15% of the plasma protein fraction. For a complement reaction to occur, the complement components must be activated in the proper sequence. Uncontrolled activation of the complement system is prevented by inhibitor proteins. Complement activation The classic pathway of complement activation is initiated by antibody bound to antigens on the surface of microbes or through soluble immune complexes. The alternate and the lectin pathways do not use antibodies and are part of the innate immune defenses. The alternate pathway of complement activation is initiated by the interaction with certain polysaccharide molecules characteristic of bacterial surfaces. The lectin-mediated pathway is initiated following the binding of a mannose-binding protein to mannose-containing molecules commonly present on the surface of bacteria and yeast. The activation of the three pathways produces similar effects on C3 and subsequent complement proteins. Complement activation Immune Cells Nonspecific immune cells Phagocytes: Neutrophyles – bacteria Eosinophyles – enzymes that kills parasites Macrophages - "big eaters" Non phagocytic leukocytes: Basophiles – role in allergic response Mastocytes Natural killer lymphocytes – antiviral and anti-tumor activity Nonspecific immune cells Macrophages have important functions in both innate and antigenspecific immune responses. As phagocytic cells with antigen nonspecific activity, they help to contain infectious agents until specific immunity can be marshaled. In addition, early in the host response, the macrophage functions as an accessory cell to ensure amplification of the inflammatory response and initiation of specific immunity. Macrophages are activated by the presence of antigen to engulf and digest foreign particles. Activated macrophages act as antigen presenting cells (APCs) that break down complex antigens into peptide fragments that can associate with class I or II Major Histocompatibility Complex (MHC) molecules. Macrophages can then present these complexes to the helper T cell so that nonself-self recognition and activation of the immune response can occur. Presentation of antigen to helper T cell by an antigen-presenting cell (APC) NK cells The NK cell is a nonspecific effector cell that can kill tumor cells and virus-infected cells. They are called natural killer cells because, unlike T cytotoxic cells, they do not need to recognize a specific antigen before being activated. NK cells kill after contact with a target cell. The NK cell is programmed automatically to kill foreign cells. Programmed killing is inhibited if the NK cell membrane molecules contact MHC self-molecules on normal host cells. The mechanism of NK cytotoxicity depends on production of poreforming proteins (i.e., NK perforins), enzymes, and toxic cytokines. Specific Immunity Specific or acquired immunity develops during an individual’s lifetime. It distinguishes self from nonself, and responds specifically to different pathogens and foreign molecules. Components: Lymphocytes are key players in the specific or acquired immune response: Lymphocytes represent 20% to 40% of blood leukocytes; T lymphocytes (also called T cells), which participate in cell-mediated immunity (60-70%); B lymphocytes (also called B cells), which participate in humoral immunity (10-20%); Cell-mediated immunity involves the production of cytotoxic T cells, which have the ability to destroy antigen-bearing cells. Humoral immunity is characterized by the transformation of B cells into plasma cells, which secrete immunoglobulins (antibodies) that have specific activity against the inciting antigen. T cells T cells are maturated in the thymus. There, they learn how to distinguish self from nonself. Only the T cells that ignore self antigen molecules are allowed to mature and leave the thymus. Without this training process, T cells could attack the body's cells and tissues. Mature T cells are stored in secondary lymphoid organs (lymph nodes, spleen, tonsils, appendix, and Peyer's patches in the small intestine). These cells circulate in the bloodstream and the lymphatic system. After they first encounter a foreign or abnormal cell, they are activated and search for those particular cells. Immune Cells Pathway for Tcell differentiation Types of T cells Helper T (CD4) cells help other immune cells. Some helper T cells help B cells produce antibodies against foreign antigens. Others help activate killer T cells to kill foreign or abnormal cells or help activate macrophages enabling them to ingest foreign or abnormal cells more efficiently. The Th1 response is characterized by the production of interferon gamma, which activates the bactericidal activities of macrophages, and induces B-cells to make opsonizing (coating) antibodies, and leads to cell mediated immunity. The Th2 response is characterized by the release of interleukin 4, which results in the activation of B-cells to make neutralizing (killing) antibodies, leading to humoral immunity. Generally, Th1 responses are more effective against intracellular pathogens (viruses and bacteria that are inside host cells), while Th2 responses are more effective against extracellular bacteria, parasites and toxins. Types of T cells Th1 cells: secrete IL-2, IL-12, IFN gamma, TNF-beta; activate macrophages, amplifying their cytokine secretion capacity and potential for presentation of antigens; activate synthesis of IgG but not IgE; are involved in delayed hypersensitivity reactions; are activated by signals from intracellular bacteria and viruses; Th2 cells: secrete IL-4, IL-5, IL-6, IL-10; activate the synthesis of IgE; stimulate proliferation and activation of eosinophils; are stimulated by allergens or parasite components. Types of T cells Killer (cytotoxic) T cells (CD8) attach to particular foreign or abnormal (for example infected) cells because they have encountered them before. Killer T cells may kill these cells by making holes in their cell membrane and injecting enzymes into the cells or by binding with certain sites on their surface called death receptors. Suppressor (regulatory) T cells produce substances that help end the immune response or sometimes prevent certain harmful responses from occurring. Sometimes T cells—for reasons that are not completely understood - do not distinguish self from nonself. This malfunction can result in an autoimmune disorder, in which the body attacks its own tissues. Types of T cells Γδ T cells (gamma delta T cells) represent a small subset of T cells, which possess a different receptor on the surface (TCR). Most T cells receptor consists of two chains α-and β-gp. Unlike T cells, γδ cells have a TCR composed of gamma and a delta chains. This group is more poorly represented than beta alpha cells. They are abundant in the intestinal mucosa. Natural killer T cells (NKT) are a heterogeneous group of T cells, which have properties of both NK cells and T cells and represents only 0.2% of all circulating T lymphocytes in the blood. The central role of Thelper cells (CD4) B cells B cells are formed in the bone marrow. B cells have particular sites (receptors) on their surface where antigens can attach. B cells are the major cells involved in the creation of antibodies that circulate in blood plasma and lymph, known as humoral immunity. In mammals there are five types of antibody IgA, IgD, IgE, IgG, and IgM, differing in biological properties. Each has evolved to handle different kinds of antigens. Upon activation, B cells produce antibodies, each of which recognizes a unique antigen, and neutralize specific pathogens. B cells The B-cell response to antigens has two stages: Primary immune response: When B cells first encounter an antigen, the antigen attaches to a receptor, stimulating the B cells. Some B cells change into memory cells, which remember that specific antigen, and others change into plasma cells. Helper T cells help B cells in this process. Plasma cells produce antibodies that are specific to the antigen that stimulated their production. After the first encounter with an antigen, production of enough of the specific antibody takes several days. Thus, the primary immune response is slow. Secondary immune response Whenever B cells encounter the antigen again, memory B cells very rapidly recognize the antigen, multiply, change into plasma cells, and produce antibodies. This response is quick and very effective. B cells Primary and secondary phases of the humoral immune response to the same antigen. Antigens Antigens or immunogens are substances foreign to the host that can stimulate an immune response. Most antigens are macromolecules such as proteins and polysaccharides, although lipids and nucleic acids occasionally can serve as antigens. Antigens include: bacteria fungi viruses protozoans parasitic worms substances such as pollen venom transplanted organs Antigens Antigens, which in general are large and complex, are biologically degraded into smaller chemical units or peptides. These discrete, immunologically active sites on antigens are called antigenic determinants or epitopes. It is the unique molecular shape of an epitope that is recognized by a specific receptor found on the surface of the lymphocyte or by the antigen-binding site of an antibody. A single antigen may contain several antigenic determinants; each can stimulate a distinct clone of lymphocytes to respond. Smaller substances (molecular masses <10,000 daltons) usually are unable to stimulate an adequate immune response. Low–molecular-weight compounds, known as haptens, combine with larger protein molecules they function as antigens. Antigens Multiple epitopes on a complex antigen being recognized by their respective (A, B, C) antibodies Immunoglobulins - structure Classes and Characteristics of Immunoglobulins Class Percentage of Total Characteristics Ig G 75% • Ig A 15% • Ig M 10% • Ig D 0.2% • Ig E 0.004% • Displays antiviral, antitoxin, and antibacterial properties • Only Ig G crosses the placenta • Responsible for protection of newborn • Activates complement and binds to macrophages Predominant in body secretions, such as saliva, nasal and respiratory secretions, and breast milk • Protects mucous membranes Forms the natural antibodies such as those for ABO blood • Antigens • Prominent in early immune responses • Activates complement Found on B lymphocytes • Needed for maturation of B cells Binds to mast cells and basophils • Involved in parasitic infections, allergic and hypersensitivity reactions Active Versus Passive Immunity Active or acquired immunity Can be achieved through exposure to a specific antigen. It is acquired through immunization or actually having a disease. Active immunity, although long lasting once established, requires a few days to weeks after a first exposure to become sufficiently developed to contribute to the destruction of the pathogen. Active Versus Passive Immunity Passive immunity Is immunity transferred from one source to another source. (e.g. An infant receives passive immunity naturally from the transfer of antibodies from its mother in utero and through a mother’s breast milk.) Passive immunity also can be artificially provided by the transfer of antibodies produced by other people or animals. Some protection against infectious disease can be provided by the injection of hyperimmune serum, which contains high concentrations of antibodies for a specific disease, or immune serum or gamma globulin, which contains a pool of antibodies for many infectious agents. Passive immunity produces only short-term protection that lasts weeks to months.