Order_writing_OSCE
advertisement
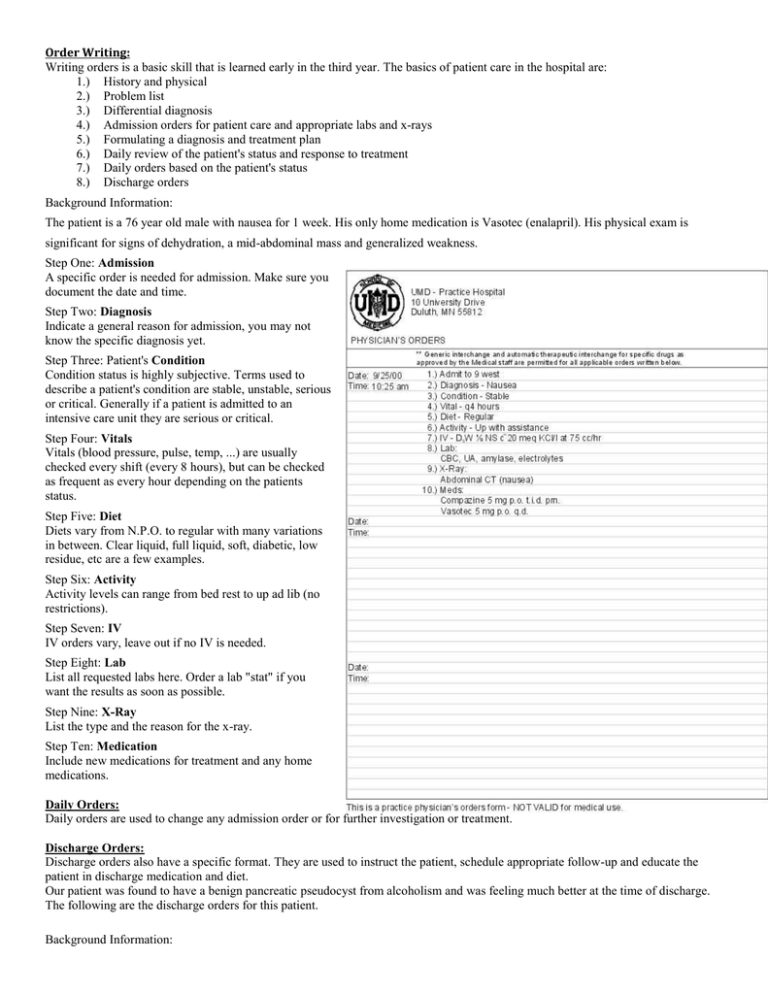
Order Writing: Writing orders is a basic skill that is learned early in the third year. The basics of patient care in the hospital are: 1.) History and physical 2.) Problem list 3.) Differential diagnosis 4.) Admission orders for patient care and appropriate labs and x-rays 5.) Formulating a diagnosis and treatment plan 6.) Daily review of the patient's status and response to treatment 7.) Daily orders based on the patient's status 8.) Discharge orders Background Information: The patient is a 76 year old male with nausea for 1 week. His only home medication is Vasotec (enalapril). His physical exam is significant for signs of dehydration, a mid-abdominal mass and generalized weakness. Step One: Admission A specific order is needed for admission. Make sure you document the date and time. Step Two: Diagnosis Indicate a general reason for admission, you may not know the specific diagnosis yet. Step Three: Patient's Condition Condition status is highly subjective. Terms used to describe a patient's condition are stable, unstable, serious or critical. Generally if a patient is admitted to an intensive care unit they are serious or critical. Step Four: Vitals Vitals (blood pressure, pulse, temp, ...) are usually checked every shift (every 8 hours), but can be checked as frequent as every hour depending on the patients status. Step Five: Diet Diets vary from N.P.O. to regular with many variations in between. Clear liquid, full liquid, soft, diabetic, low residue, etc are a few examples. Step Six: Activity Activity levels can range from bed rest to up ad lib (no restrictions). Step Seven: IV IV orders vary, leave out if no IV is needed. Step Eight: Lab List all requested labs here. Order a lab "stat" if you want the results as soon as possible. Step Nine: X-Ray List the type and the reason for the x-ray. Step Ten: Medication Include new medications for treatment and any home medications. Daily Orders: Daily orders are used to change any admission order or for further investigation or treatment. Discharge Orders: Discharge orders also have a specific format. They are used to instruct the patient, schedule appropriate follow-up and educate the patient in discharge medication and diet. Our patient was found to have a benign pancreatic pseudocyst from alcoholism and was feeling much better at the time of discharge. The following are the discharge orders for this patient. Background Information: The patient is a 76 year old male with nausea for 1 week. His only home medication is Vasotec (enalapril). His physical exam is significant for signs of dehydration, a mid-abdominal mass and generalized weakness. Our patient was found to have a benign pancreatic pseudocyst from alcoholism and was feeling much better at the time of discharge. Step One: Discharge to _____ A specific order is needed for discharge. You need to specify where the patient is being discharged to - home, nursing home, board and care home, etc. Step Two: Diet List the type of diet the patient should be following after being discharged. Step Three: Physical Activity List the level of activity for the patient. Activity levels can range from bed rest to no restrictions. Step Four: Medication List all the medications the patient will be on, not just the new medications. Step Five: Follow-up List any follow-up visit the patient needs. Practice Discharge order form: Background Information: The patient was found to have pneumonia in the left lower lobe. He was treated with IV Levaquin then was switched to oral Levaquin 250 mg po qd before discharge. He will need antibiotics for 6 more days after discharge. He should see Dr. Smith three weeks after discharge with a chest X-ray that day. He was discharged on October 3rd at 9:00 am.