Clinical Documentation Integrity Fact Sheet – Discharge Summary
advertisement
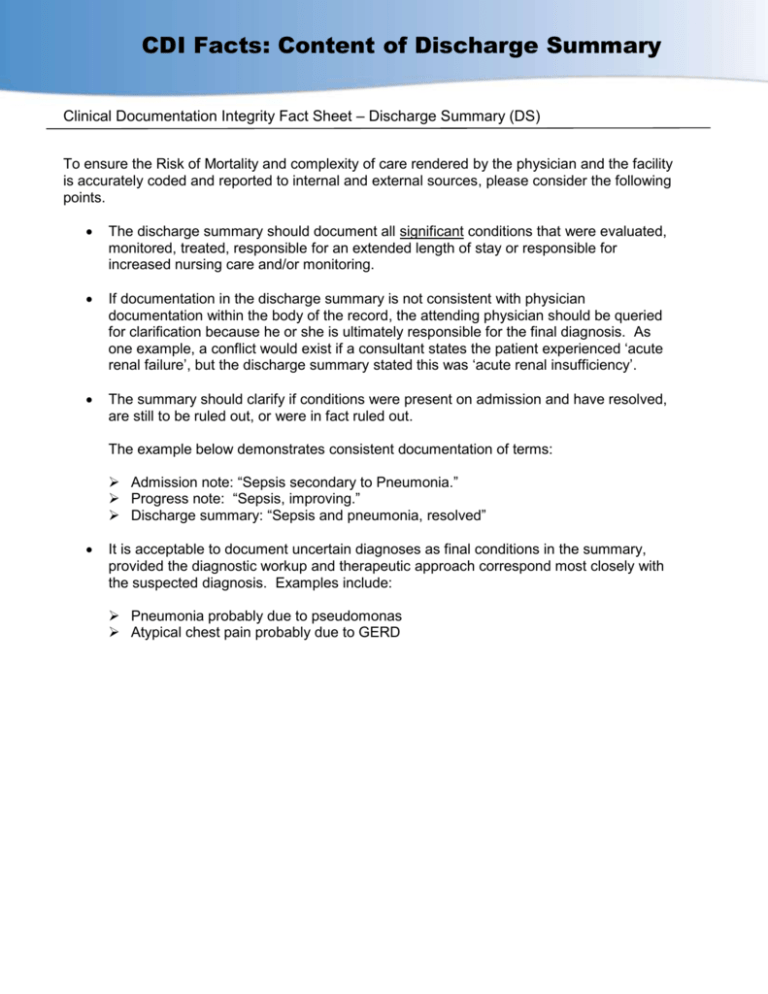
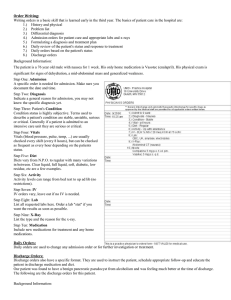
CDI Facts: Content of Discharge Summary Clinical Documentation Integrity Fact Sheet – Discharge Summary (DS) To ensure the Risk of Mortality and complexity of care rendered by the physician and the facility is accurately coded and reported to internal and external sources, please consider the following points. The discharge summary should document all significant conditions that were evaluated, monitored, treated, responsible for an extended length of stay or responsible for increased nursing care and/or monitoring. If documentation in the discharge summary is not consistent with physician documentation within the body of the record, the attending physician should be queried for clarification because he or she is ultimately responsible for the final diagnosis. As one example, a conflict would exist if a consultant states the patient experienced ‘acute renal failure’, but the discharge summary stated this was ‘acute renal insufficiency’. The summary should clarify if conditions were present on admission and have resolved, are still to be ruled out, or were in fact ruled out. The example below demonstrates consistent documentation of terms: Admission note: “Sepsis secondary to Pneumonia.” Progress note: “Sepsis, improving.” Discharge summary: “Sepsis and pneumonia, resolved” It is acceptable to document uncertain diagnoses as final conditions in the summary, provided the diagnostic workup and therapeutic approach correspond most closely with the suspected diagnosis. Examples include: Pneumonia probably due to pseudomonas Atypical chest pain probably due to GERD