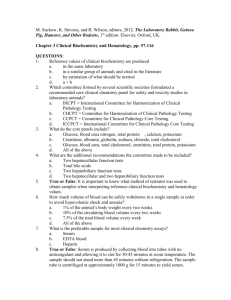
introduction to lab medicine 1
advertisement

INTRODUCTION TO LABORATORY MEDICINE DEFINITION Laboratory medicine a specialty in which pathologists provide testing of patient samples (usually blood or urine) in several different areas. Determination of the level of enzymes in blood in case of heart attack or Level of glucose (sugar) in the blood of a patient with diabetes. The presence of bacteria and other microorganisms. Blood cells studies for various types of anemias COURSE OBJECTIVES application of basic science to those clinical disciplines practiced by the medical laboratory scientist. the scope of Laboratory Medicine, and of its potential applications. How to analyze various samples under certain circumstances. COURSE CONTENTS Clinical Biochemistry Cardiac profiles Liver and renal panels Bone metabolism Lipid chemistry Special chemistry Cardiovascular markers Tumour markers Nutritional markers Calculi Immunology and Immunodiagnostics Drug monitoring Urine and serum proteins Autoimmune disease testing Endocrinology tests Fertility testing Point-of-Care Testing Cardiac markers Glucose monitoring program Blood gases and metabolites Routine chemistry panels Routine urinalysis and pregnancy screening Coagulation Complete Blood Counts Urine toxicology screening Laboratory Hematology Routine and special hematology Hemoglobinopathy studies Special stains Hematopathology Bone marrow consultations and interpretive report Flow cytometry CD 34 (stem cell) enumeration CD4/CD8 monitoring Leukemia/lymphoma immunophenotyping PNH Special coagulation Coagulation profiles, screening and factors and inhibitors Platelet studies Thrombophilia testing Microbiology Bacterial culture and sensitivities Blood cultures Molecular typing of organisms Viral detection methodologies HIV viral load -public health lab accredited site for viral load Chlamydia detection Infection control Reference centre for medical microbiology and infectious diseases Detection and typing of epidemiologically significant organisms Serology Clostridium difficile toxin testing Wide range of viral and non-viral serologies Molecular Diagnostic Testing Wide range of molecular testing for viral and bacterial agents Mycology Fungus detection Cells/tissues/organ donor testing Blood Bank/Donor Center Concepts of immunohematology and histocompatibility Blood transfusion services and quality assurance Blood donation and storage of blood Blood grouping Compatibility testing RECOMMENDED BOOKS Textbook: District laboratory practice in tropical countries by Monica Cheesbrough. Clinical chemistry by William J Marshall. Reference books: Medical Laboratory technology by Ramnik Sood. REASONS FOR ORDERING TESTS Aid in diagnosis Confirm diagnosis Evaluate prognosis Monitor therapy Screen for a disease SECTIONS OF THE LABORATORY CLINICAL PATHOLOGY 1. Clinical Chemistry BUN Cholesterol FBS 2. Clinical Microscopy Analysis of body fluids Urin analysis Fecal anaysis Semen analysis 3. Microbiology Cultures (sputum, blood, urine) 4. Hematology Biggest section Includes CBC,coagulation, PT, PTT BLOOD BANK Very critical section Serology/Immunology Bec. May have errors Blood typing Cross match AB Identification Goes hand in hand with serology and immunology Tests done for MALARIA SYPHILIS HIV Cardiac and thyroid fxntest II. ANATOMY PATHOLOGY Histopathology Submission of tissues for tests LABORATORY SERVICES Laboratory investigations of the patient. Laboratory aspects of detection and prevention of diseases. Request System of analysis System for interpretation of results and timely advice relevant to the urgency of the clinical problem FUNCTIONS OF A HOSPITAL LABORATORY To meet the request for laboratory investigations by maintaining adequate diagnostic facilities. To arrange for laboratory investigations from referral laboratories if not available in the premises. To provide professional advice on the management of the patient. To monitor individual patients. To provide laboratory facilities for research projects under taken by clinicians. To collaborate in development, study and control of new methods of treatment. To understand applied research on pathology related problems. To arrange for the training of the medical and paramedical staff. NATURE OF REQUEST STAT Performed immediately and by itself. Run control and standard 20-50% More expensive TAT is shortened Request is needed Today Confusing Performed as soon as possible, given priority Based on “running time” Routine Done with the batch Wait for TAT stated by laboratory VALUES REFERENCE VALUES Better term than “normal value” Pulled value, usually 95%of population Vary in diff. hospitals but not that far SIGNIFICANT VALUES Clinical decision should be made if higher or lower than reference value Usually when 2x to 3x CRITICAL VALUES Needs immediate attention “panic values” Should call physician Patient is at risk REFERENCE VALUES Not fixed for all Should consider: Age Sex Pregnancy Diurnal Variation Race Blood type ROUTINE EXAMINATIONS ROUTINE ADMISSION TESTS CBC, Urinalysis, Fecalysis ROUTINE CHEMISTRIES BUN, Creatinine, Glucose, Uric Acid, Cholesterol Sometimes triglycerides BASIC LAB EQUIPMENTS The Light Microscope. Colorimeters and photometers Water bath Laboratory centrifuge Balance Cold incubators refrigerators pH meters Mixers Ovens De-ionizers Safety cabinets. Glassware and plasticware SAMPLING Pathologist should try to answer the question which is imposed by the clinician. Correct specimen for requested test with necessary information so that right test is carried out And result is delivered to the requesting clinician with the minimum of delay. Patient identification must be correct. SPECIMEN TYPES Venous blood serum or plasma. Arterial blood. Capillary blood Urine Feces Cerebrospinal fluid Sputum and sliva Tissue and cells Aspirates (pleural fluid, ascites, joint fluid, intestinal (duodenal) fluid, pancreatic pseudocysts. Calculi BLOOD SPECIMENS Serum Plasma Urine specimen Preservative may be added to prevent bacterial growth or acid may be added to stabilize metabolites. Other specimen types Dangerous specimen Labelled as “dangerous specimen” yellow sticker. Similar label should be attached on the request form. HBV and HIV SAMPLING ERRORS Blood sampling techniques Prolonged stasis during venepuncture Insufficient specimen Errors in timing Incorrect specimen container In appropriate sampling site Incorrect sample storage. LIPID CHEMISTRY AND CARDIOVASCULAR PROFILE Main lipids in the blood are the triglycerides and cholesterol.(phospholipids, FFA) These are insoluble in the water. Transport in the blood is via lipoproteins.(protein) 4 major classes of lipoproteins. Chylomicrons Very low density lipoproteins (VLDL) Low density lipoproteins (LDL) High density lipoproteins (HDL) LIPOPROTEINS COMPOSITIONS COMPOSITION OF LIPOPROTEINS Class Diamete r (nm) % triacylglyc % % erol % protein phospholipi cholesterol & d cholesterol ester HDL 5–15 33 30 29 4 LDL 18–28 25 50 21 8 IDL 25–50 18 29 22 31 VLDL 30–80 10 22 18 50 8 7 84 Chylomicr 100-1000 <2 ons LIPOPROTEINS Chylomicrons carry triglycerides ( dietary fat) from the intestines to the liver, to skeletal muscle, and to adipose tissue. Very-low-density lipoproteins (VLDL) carry (newly synthesised or endogenous) triglycerides from the liver to adipose tissue and metabolized to LDL through IDL. Intermediate-density lipoproteins (IDL) are intermediate between VLDL and LDL. They are not usually detectable in the blood. Low-density lipoproteins (LDL) carry cholesterol from the liver to cells of the body. LDLs are sometimes referred to as the "bad cholesterol" lipoprotein. High-density lipoproteins (HDL) collect cholesterol from the body's tissues, and take it back to the liver. HDLs are sometimes referred to as the "good cholesterol" lipoprotein. LIPOPROTEIN METABOLISM 60% of plasma cholesterol is present in LDL, 25% in HDL and small quantity in VLDL. Lipoprotein metabolism is controlled by their protein component apolipoproteins. Apo A-1 in HDL and Apo B-100 in LDL are very important ones. Lipoprotein (a) in also present in human plasma. It is synthesized in the liver. Smaller but denser than LDL. Cholesterol esters are major lipids and it is an independent risk factor for IHD. LDL and VLDL are associated with premature atherosclerosis. HDL high levels are negative risk factors for IHD. HYPERLIPIDEMIA Coronary heart disease Acute pancreatitis Failure to thrive and weakness Cataract Endothelial dysfunction Lpid accumulation. Migration of inflammatory cells into the arterial wall. Atherosclerosis and plaque formation Plaque stability SCAD (asymptomatic) Chest pain at rest (angina, non ST elevation MI, STEMI) PATHOPHYSIOLOGY Atherosclerotic plaque, rupture and thrombus formation. Obstruction of coronary circulation. Necrosis of the heart tissue. Irreversible cardiac injury if occlusion is complete for 15-20 mins. Starts from endocardium and spreads towards epicardium. If full thickness of myocardium is involved then it is transmural infarct. PRECIPITATING FACTORS Physical exertion After surgical operation Early in the morning (adrenergic activity, fibrinogen level, platelet adhesiveness is increased). In the winter months Emotional stress DIAGNOSIS OF MI Detection of rise and fall of cardiac biomarker troponinT/I with one of the following: Symptoms of ischemia ECG changes Q wave ECG CHANGES CARDIAC PROFILE TEST ENZYMES Creatinine Kinase –MB(CK-MB) Lactate Dehydrogenase(LDH 1 and 2) Aspartate Aminotransferase(AST)/Serum Glutamate Oxaloacetate Transaminase(SGOT) Alanine Aminotransferase(ALT)/ Serum Pyruvate Transaminase(SGPT) LIPID PROFILE CHOLESTEROL TRIGLYCERIDE HDL LDL PROTEINS Myoglobin Troponins CARDIAC PROFILE Cardiac Enzymes Cardiac Profile assesses the function of the heart’s muscle and the increased level of enzymes following a myocardial infarction. The cardiac enzymes include the following: Aspartate aminotransferase (AST) Lactate dehydrogenase (LD) Creatine Kinase (CK) ASPARTATE AMINOTRANSFERASE (AST) (SGOT) found in all tissue, especially the heart, liver, and skeletal muscles it catalyzes the transfer of the amino group of aspartic acid to alphaketoglutaric acid to form oxaloacetic acid and glutamic acid Reaction catalyzed: Amino group Alpha-keto group Oxaloacetate & In aspartic acid In alpha-ketoglutaric acid glutamate Considerations in AST assays -Serum is the best specimen -Hemolyzed samples must be avoided -Alcohol lowers AST values -Muscle trauma like intramuscular injections, exercise, or surgical operation can significantly increase AST levels CLINICAL SIGNIFICANCE Myocardial infarction In myocardial infarction, AST levels are usually 4-10 times the upper limit of normal These develop within 4-6 hours after the onset of pain Peak on the 24th – 36th hour Usually normalize on the 4th or 5th day Muscular dystrophy Hepatocellular disorders Skeletal muscle disorders Acute pancreatitis INCREASED LEVELS OF AST Drug hepatoxicity Pulmonary infarction Pericarditis Acute hepatitis Skeletal muscle disorders DECREASED LEVELS OF AST Pregnant women Falsely elevated results Bilirubin Aceto-acetatae N-acetyl compounds P-aminophenol Sulfathiozole Isoniazid Methyldopa L-dopa Ascorbic acid LACTATE DEHYDROGENASE (LDH) Catalyzes the reversible oxidation of lactate to pyruvate Used to indicate AMI Is a cytoplasmic enzyme found in most cells of the body, including the heart Not specific for the diagnosis of cardiac disease DISTRIBUTION OF LD ISOENZYMES LD1 and LD2 (HHHH, HHHM) Fast moving fractions and are heat-stable Found mostly in the myocardium and erythrocytes Also found in the renal cortex LD3 (HHMM) Found in a number of tissues, predominantly in the white blood cells and brain LD4 and LD5 (HMMM, MMMM) Slow moving and are heat labile Found mostly in the liver and skeletal muscle CONSIDERATIONS IN LD ASSAYS Red cells contain 150 times more LDH than serum, therefore hemolysis must be avoided LDH has its poorest stability at 0°C Clinical Significance In myocardial infarction, LD increases 3-12 hours after the onset of pain Peaks at 48-60 hours and remain elevated for 1014 days In MI, LD1 is higher than LD2, thus called “flipped” LD pattern FLIPPED LDH An inversion of the ratio of LD isoenzymes LD1 and LD2; LD1 is a tetramer of 4 H–heart subunits, and is the predominant cardiac LD isoenzyme; Normally the LD1 peak is less than that of the LD2, a ratio that is inverted–flipped in 80% of MIs within the first 48 hrs DiffDx. LD flips also occur in renal infarcts, hemolysis, hypothyroidism, and gastric CA INCREASED LEVELS OF LD Megaloblastic anemia Pulmonary infarction Granulocyte leukemia Hodgekin’s disease Hemolytic anemia Infectious mononucleosis Progressive muscular dystrophy (PMD) CREATINE KINASE (CK) Is a cytosolic enzyme involved in the transfer of energy in muscle metabolism Catalyzes the reversible phosphorylation of creatine by ATP -Is a dimer comprised of two subunits, resulting in three CK isoenzymes The B, or brain form The M, or muscle form Three isoenzymes isolated after electrophoresis: CK-BB (CK1) isoenzyme Is of brain origin aand only found in the blood if the bloodbrain barrier has been breached CK-MM (CK3) isoenzyme Accounts for most of the CK activity in skeletal muscle CK-MB (CK2) isoenzyme Has the most specificity for cardiac muscle It accounts for only 3-20% of total CK activity in the heart Is a valuable tool for the diagnosis of AMI because of its relatively high specificity for cardiac injury Established as the benchmark and gold standard for other cardiac markers Considerations in CK assays CK is light sensitive and anticoagulants like oxalates and fluorides inhibit its action CK in serum is very unstable and rapidly loss during storage Stored specimens are not used since it contains cellular products and intermediate like adenylate kinase, ATP and G-6-Phosphate which affect the assay Exercise and intramuscular injections causes CK elevations Clinical Significance -In myocardial infarction, CK will rise 4-6 hours after the onset of pain -Peaks at 18-30 hours and returns to normal on the third day -CK is the most specific indicator for myocardial infarction (MI) Raised levels of CK Progressive muscular dystrophy Polymyositis Acute psychosis Alcoholic myopathy Delirium tremens Hypothyroidism Malignant hyperthermia Acute cerebrovascular disease Trichinosis and dermatomyositis Normal Value: a. Male – 25-90 IU/mL b. Female – 10-70 IU/mL CHOLESTEROL Normal values: range varies according to age Total Cholesterol: 150-250mg% Cholesterol esters: 60-75% of the total cholesterol CHOLESTEROL IS ADVISED IF YOU have been diagnosed with coronary heart disease, stroke or mini-stroke (TIA) or peripheral arterial disease (PAD) are over 40 have a family history of early cardiovascular disease have a close family member with cholesterol-related condition are overweight have high blood pressure, diabetes or a health condition that can increase cholesterol levels, such as an underactive thyroid FACTORS LEADING TO RAISED CHOLESTEROL an unhealthy diet: some foods already contain cholesterol (known as dietary cholesterol) but it is the amount of saturated fat in your diet which is more important smoking: a chemical found in cigarettes called acrolein stops HDL from transporting LDL to the liver, leading to narrowing of the arteries (atherosclerosis) having diabetes or high blood pressure(hypertension) having a family history of stroke or heart disease There is also an inherited condition known as familial hypercholesterolaemia (FH). This can cause high cholesterol even in someone who eats healthy diet. TRIGLYCERIDES Ester derived from glycerol and three fatty acids. Main lipids in the blood and important energy substrate. Insoluble in water. Hypertriglyceridemia Not an important risk facotr for coronary artery disease. It can cause pancreatitis when severe. Both hypertriglyceridemia and hypercholesterolemia are associated with various types of cutaneous fat deposition and xanthomatas. Hypertension Very common clinical problem. Usually essential type meaning that have no identifiable cause. Investigations for treatable causes like endocrine is necessary. HYPERLIPIDEMIAS LIVER Anatomy of liver LIVER HISTOLOGY I. TESTS BASED ON EXCRETORY FUNCTIONS LABORATORY RESULTS II. TESTS DUE TO DETOXIFICATION TESTS B/O SYNTHETIC FUNCTION Liver is the main source of synthesis of Plasma proteins Albumin Globulin Blood clotting factors Prothrombin Factors V, VII, and X SERUM ALBUMIN 3.5- 5.5 gm/dl SERUM GLOBULIN 2 -3.5 gm/dl TOTAL PROTEINS 6-8 gm/dl Albumin/ Globulin ratio 1.2:1 – 2.5: 1 Prothrombin time TESTS B/O METABOLIC FUNCTIONS SERUM TRANSAMINASES SERUM ALKALINE PHOSPHATASES REFERENCE RANGE ALT ( upto 42 U/L) AST (0-37 U/L) ALP (65-306 U/L) raised in obstructive jaundice. OTHER ENZYMES GGT (11-60 u/l) 5- NUCLEOTIDASE (2-17u/L) LDH (180-360 u/l) pathogenesis Different cells have different enzymes inside them, depending on the function of the cell. Liver cells happen to have lots of AST, ALT, and GGTP inside them. When cells die or are damaged, the enzymes leak out causing the blood level of these enzymes to rise; that is why the levels of these enzymes in the blood are considered good indicators of liver cell damage. ALT is more specific for liver disease than AST because AST is found in more types of cell (e.g. heart, intestine, muscle). The AST, for instance, will rise after a heart attack or bruised kidney. GGTP and AP are said to be more specific for evaluating biliary disease since they are made in bile duct cells. In liver disease caused by excess alcohol ingestion, the AST tends to exceed the ALT, while the reverse is true to for viral hepatitis. However, this particular generalization is often wrong. There are several things to remember: GGT (OR GGTP) Gamma Glutamyl Transpeptidase. This enzyme level is elevated in case of liver disorders. In contrast to the alkaline phosphatase, the GGT tends not to be elevated in diseases of bone, placenta, or intestine PROTHROMBIN TIME good correlation between abnormalities in prothrombin time and the degree of liver dysfunction. Expressed in seconds and compared to a normal control patient's blood SPECIALIZED TESTS serum iron, the percent of iron saturated in blood, the storage protein ferritin for hemochromatosis. accumulation of copper in the liver in wilson disease. RENAL PANEL Creatinine Calcium Sodium Chloride Carbon dioxide Albumin Blood urea nitrogen (BUN) Protein Phosphorus Glucose Potassium Glucose Potassium Phosphorous Sodium Albumin BUN Creatinine BUN/Creatinine Ratio Calcium Chloride Carbon Dioxide (CO2), Total BONE METABOLISM Bone is constantly remodelling Bone resorption= bone formation Why remodelling is necessary? To withstand changing environment To cope with workload To repair damage caused by recurrent microtraumas BONE METABOLISM Osteoclasts and Osteoblasts Osteocytes\ Encased osteoblasts which are connected to each other by long cellular processes forming a network connected by gap junctions.