Eyecare Review
advertisement

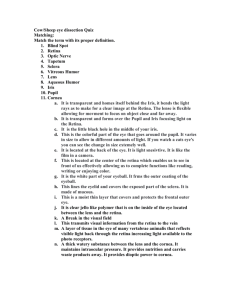
Eyecare Review— For Primary Care Practitioners Primary Care Practitioners See variety of eye problems Discuss treatment options Facilitate referrals Positioned to explain optometry's role as primary eye care providers Outline Anatomy Optics Turned Eyes Lazy Eye External Conditions Internal Conditions Diabetic Retinopathy ANATOMY Basic Anatomy Sclera Choroid Retina Cornea Fovea Pupil Lens Iris Ciliary Body Optic Nerve Lids Lashes—protection from foreign material Glands—lubricate anterior surface o Meibomian glands o Glands of Zeis o Glands of Moll Conjunctiva Thin, transparent, vascular layer lining o Backs of eyelids o Fornices o Anterior sclera Sclera Tough outer shell Composed of collagen bundles Protects from penetration Cornea Composed of regularly oriented collagen fibers 5 layers Anterior Chamber Space between cornea and iris Filled with aqueous humor produced by ciliary body Iris Iris gives eye color 2 muscles: o Dilator—opens o Sphincter—constricts Pupil Allows light to enter Enables view to back of eye and eye health evaluation Lens Located behind iris Focuses light on retina Allows for accommodation Normally transparent Where cataracts form Ciliary Body Primary functions o Pulls on lens for accommodation o Epithelium secretes aqueous fluid that fills anterior chamber Red Reflex Light reflection off retina Useful for assessing media clarity Affected by any opacity of cornea, lens, vitreous White reflex = leukocoria Refer immediately! Vitreous Humor Gel-like fluid that fills back cavity Serves as support structure for blood vessels while eye formed—before birth After birth, just ‘hangs out’ in there Where floaters are located Fundus Interior surface of eye Includes o Optic nerve o Retina o Vasculature Optic Nerve Head Collection of nerve fibers and blood vessels from retina Transfers info to brain’s visual cortex Slightly yellow-pink when healthy White ‘full moon’ appearance can mean trouble! Optic Nerve Head Cup is natural depression in center of nerve Cup size varies between people Very large cup, or change in appearance over time, can indicate glaucoma Physiologic Cup Optic Nerve Optic Disc Macula Dense collection of cone photoreceptors Fine detail and color vision Macular degeneration affects this area Retinal Vessels Include arteries and veins Only place in body where you can directly visualize blood vessels Excellent indicators of systemic diseases o o o o HTN Diabetes High cholesterol Carotid disease Peripheral Retina Can only be evaluated with dilated pupil Important to evaluate periodically to fully assess eye health OPTICS Optics Review Myopia Hyperopia Astigmatism Presbyopia Myopia Nearsightedness See well up close but blurry in distance Eye is too long Light focuses in front of retina Hyperopia Farsightedness See well in distance Eye is too short Focus point is behind retina Hyperopia Blurry image on retina Lens focuses to compensate Hyperopes often asymptomatic much their of lives Can cause headaches or eyestrain with extended reading These problems can get worse after age 40 Astigmatism Surface of cornea is irregular or misshapen Light focuses at various points causing distorted vision Often combined with nearsightedness and farsightedness Presbyopia Normal, age-related change Near vision becomes difficult Mid-40s lens becomes less elastic and loses ability to change focus Time for bifocals… MISALIGNED EYES Turned Eyes - Strabismus Eye misalignment o One or both turn in, out, up or down Caused by muscle imbalance 3 Kinds of Strabismus o Esotropia o Exotropia o Hypertropia 1. Esotropia Eye turns in towards nose 3 Types of Esotropia Infantile (congenital) o Develops in first 3 months of life o Surgery usually recommended— along with vision therapy and glasses Accommodative o Usually noted around age 2 o Child typically farsighted o Focusing to make images clear can cause eyes to turn inward o Treated with glasses but vision therapy may also be needed 3 Types of Esotropia Partially Accommodative o Combination of accommodative dysfunction and muscle imbalance o Glasses and vision therapy won’t completely correct eye turn o Surgery may be required for best binocularity If you see Esotropia Refer to pediatric optometrist or ophthalmologist Sooner the better for best chance of good vision 2. Exotropia Eye turns outward Congenital—present at birth Surgery usually needed to re-align Many exotropias are intermittent o May occur when patient is tired or not paying attention o Concentration can force eyes to re-align o Vision therapy and/or glasses can help 2. Exotropia When intermittent o Brain sometimes receives info from both eyes (binocular) o Less chance of amblyopia o However, important to be seen by eyecare provider when deviation noted 3. Hypertropia One eye vertically misaligned Usually from paresis of an extra-ocular muscle Typically much more subtle for patient to describe and provider to diagnose 2 Types Congenital o Most common type o Patients can compensate for years by tilting head o Can be discovered by looking at childhood photos 2 Types Acquired o Trauma— Extra-ocular muscle ‘trapped’ by orbital fracture o Vascular infarct— Systemic diseases that affect blood supply to nerves can cause temporary nerve palsy Diabetes and HTN most common Palsies tend to resolve over weeks or months o Neurological— In rare cases a tumor or aneurysm can cause symptoms LAZY EYE Lazy Eye - Amblyopia Decreased vision uncorrectable by glasses or contacts—not due to eye disease For some reason, brain doesn’t fully acknowledge images seen Lazy Eye - Amblyopia 3 Types of Amblyopia o Strabismic o Anisometropic o Stimulus deprivation 1. Strabismic Amblyopia One eye deviates from other and sends conflicting info to brain Brain doesn’t like to see double— so “turns off ” info from deviated eye Results in under developed visual cortex for that eye Can usually be reversed or decreased if treated during first 9 years Need to visit eyecare provider ASAP to determine cause Treatment If caught early, treatment can teach brain how to see better o Vision therapy/patching o Glasses o Surgical re-alignment Early vision screenings are critical! 2. Anisometropic Amblyopia Anisometropia—significant difference in Rx between eyes Commonly one eye more farsighted Farsighted eye works hard to see clearly—and sometimes gives up Brain relies on info from other eye 2. Anisometropic Amblyopia If not caught, one eye won’t learn to see as well as other Vision therapy and glasses are both beneficial Sooner the better 3. Deprivational Amblyopia Any opacity in visual pathway can be devastating to developing visual system o Congenital cataracts o Corneal opacities o Ptosis (droopy eyelid) o Other media opacities EXTERNAL CONDITIONS Common External Ocular Conditions Blepharitis Hordeolum—stye Preseptal cellulitis Orbital cellulitis Pterygium Corneal ulcer Conjunctivitis o o o o o o Viral “pink eye” Adenovirus Bacterial Allergic Hyperacute Chlamydial Blepharitis Inflammation of eyelids (anterior or posterior) Symptoms o o o o o Itching Burning Crusting Dry eye sensation Foreign body sensation Blepharitis Signs o Crusts on lid margins o Thickened, reddened eyelids o Plugged or inspisated meibomian glands along eyelid Treatment o Warm compresses, 10 minutes 1-2 x/day o Lid scrubs with diluted baby shampoo o Artificial tears o Erythromycin ointment at night Hordeolum (stye) Abscessed meibomian gland Raised, tender nodule Often gets larger over days to a week Hordeolum Signs o Raised nodule protruding out from or under lid o Red, swollen lid o Capped glands at site of infection Treatment o Warm compresses, BID-TID for 10 mins o Topical meds don’t penetrate abscess o Oral antibiotics if no response to traditional treatment Preseptal Cellulitis Bacterial infection of eyelid anterior to orbital septum Can arise from o concurrent sinus infection o penetrating lid trauma o dental infection o hordeolum o insect bite Preseptal Cellulitis Signs o Painful, swollen lid extending past orbital rim o May be unable to open eye o No decreased vision, restricted ocular motility or proptosis o White conjunctiva Treatment o Amoxicillin (augmentin) 500 mg PO TID o Treat infection quickly to minimize risk of orbital cellulitis Orbital Cellulitis Serious infection of soft tissues behind orbital septum Can be life-threatening Causes o Sinus infection o Extension of preseptal cellulitis o Dental infection o Penetrating lid injury o After ocular surgery Orbital Cellulitis Signs o Tender, warm periorbital lid edema o Proptosis o Painful ophthalmoplegia o Decreased vision o Severe malaise, fever and pain Treatment o Medical emergency o Hospitalization with IV antibiotics o Consider orbit/head CT to look for abscess o Consult pediatrician or infectious disease specialist Preseptal vs. Orbital Cellulitis Preseptal o Painful, swollen lid extending beyond orbital rim o Normal vision o Full EOMs o White conjunctiva o No proptosis o No fever Orbital o Painful, swollen lid that stops at orbital rim o Decreased vision o Restricted ocular motilities o Proptosis o Fever/malaise Pterygium Triangular-shaped growth of conjunctival tissue onto cornea Causes o UV exposure o Dryness o Irritants Smoke Dust Pterygium Signs o o o o Dry eye Irritation Redness Blurred vision Management and Treatment o UV tint on glasses o Avoid irritating environments o Artificial tears o Topical vasoconstrictor or mild steroid o Surgery Corneal Ulcer Infection of cornea o Bacterial o Fungal o Acanthamoeba Causes o SCL wearer o Trauma o Compromised cornea from preexisting condition Corneal Ulcer Signs o o o o o Pain Photophobia Blurred vision Discharge Hypopyon Treatment: o Start immediately Fortified antibiotics Fluoroquinolones o Culture may not be necessary if ulcer is small o Must be monitored daily! Conjunctivitis (red eye) Various Causes 1. Viral/Adenovirus 2. Bacterial 3. Allergic 4. Chlamydial 5. Herpetic 6. Toxic Conjunctivitis Signs o o o o o Irritation Burning/stinging Watering Photophobia Pain or foreign body sensation o Itching Discharge o o o o Watery Mucoid Mucopurulent Purulent 1. Viral Conjunctivitis (pink eye) Most viral infections are fairly mild and self-limiting Signs & Symptoms o Watering o Redness o Photophobia o Discomfort/foreign body sensation o Palpable preauricular node 1. Viral Conjunctivitis Patients often have recent history of URI Treat symptoms o Cool compresses o Artificial tears o Topical vasoconstrictors or mild antiinflammatory Frequent handwashing Usually runs course in 1-3 weeks 2. Adenoviral Conjunctivitis Highly contagious Most common types o Pharyngoconjunctival fever (PCF)— can be caused by adenovirus types 3, 4 & 7 o Epidemic keratoconjunctivitis (EKC)— caused most commonly by adenovirus types 8 & 19 2. Adenoviral Conjunctivitis Signs o Watering o Conjunctival follicles o Subconjunctival hemorrhages o Chemosis o Pseudomembranes o Lymphadenopathy o Keratitis 3. Bacterial Conjunctivitis Common, especially in children Usually self-limiting Signs/symptoms o Acute redness o Burning/grittiness o Mucopurulent discharge o Lids stuck shut in morning 3. Bacterial Conjunctivitis Common organisms: S. aureus, S. epidermidis, S. pneumonia, H. influenza (esp. peds) Usually self-limiting But important to use broad-spectrum antibiotic until discharge cleared (5-7 days) Antibiotics o Tobramycin o Polytrim—polymyxin + trimethoprim o Fluoroquinolones like Ocuflox or Ciloxan 5. Hyperacute Conjunctivitis Cause o Sexually transmitted o Neisseria gonorrhoeae Signs o Swollen, tender lids o Copious purulent discharge o Significant conjunctival redness and swelling o Lymphadenopathy 5. Hyperacute Conjunctivitis Treatment o Lavage o Take scrapings for culture and sensitivity testing o Patients usually hospitalized and started on IM Ceftriaxone o Topical antibiotics not effective 6. Chlamydial Conjunctivitis Cause o Sexually transmitted ocular infection Signs o Patients typically have mild but persistent follicular conjunctivitis non respondent to topical antibiotics o Any conjunctivitis lasting longer than 3 weeks despite therapy should be suspect 6. Chlamydial Conjunctivitis Patients can have concomitant genital infection (could be asymptomatic) o Refer for work-up if necessary Treatment o Oral—Azithromycin 1g, doxycycline 100mg bid x 7 days, erythromycin 500mg qid x 7 days. Also need to tx partners! o Topical—erythromycin, tetracycline, or sulfacetamide ung bid-tid x 2-3 weeks 4. Allergic Conjunctivitis Can be seasonal or acute Signs/symptoms o o o o o o Itching is hallmark Conjunctival redness Chemosis Lid edema Thin, watery discharge No palpable preauricular nodes 4. Allergic Conjunctivitis Treatment o Eliminate offending agent o If mild Cool compresses Artificial tears/vasoconstrictors o If moderate or severe Topical antihistamine/mast-cell stabilizer (ie. Patanol) Topical NSAID Topical steroid Oral antihistamine INTERNAL CONDITIONS Internal Ocular Conditions Glaucoma Cataracts Macular Degeneration Retinal detachment Glaucoma Progressive loss of Nerve fiber layer at ONH (increased cupping) Can lead to peripheral visual field loss Sometimes caused by elevated intraocular pressure Glaucoma Pathophysiology of progression not well understood Increased IOP o Damages nerves as they leave eye, causing cell death o Reduces blood supply to ONH, indirectly destroying cells by starving them of oxygen and nutrients Abnormal levels of neurotransmitter (glutamate) cause cells to die off Glaucoma Monitoring o o o o IOP ONH appearance Visual field testing Newer methods include HRT (Heidelberg Retinal Tomograph II) GDx Nerve Fiber Analyzer Genetic testing Glaucoma IOP reduction is mainstay of treatment Decrease aqueous production o B-blockers o Alpha-agonists o Carbonic anhydrase inhibitors Increase uveoscleral outflow o prostaglandin analogs Cataract Clouding of natural lens Patients experience o Blurred/dim vision o Glare, especially at night o Halos around lights o Doubling or ghost images of objects Etiology Everyone develops them if they live long enough! Types of cataracts o Age-related—senile o Trauma—blunt or perforating injury o Systemic conditions—diabetes o Medications—steroids Main Types Age-related o Nuclear sclerotic o Cortical spokes o Posterior subcapsular o Mature cataract Treatment Surgery When loss of vision interferes with daily activities o Driving o Reading o Hobbies Outpatient Surgery 5-10 minutes with skilled surgeon o Incision through cornea or sclera under upper lid o Circular tear in anterior capsule o Lens broken up with ultra sound instrument o Fragments suctioned out o Lens implant inserted Secondary Cataract Cloudiness forms on posterior capsule after cataract surgery 30-50% of patients YAG laser used to create opening Vision quickly restored Macular Degeneration #1 cause of blindness in Americans over age 65 Pathophysiology Causes not well understood Theorized link to o UV light exposure o subsequent release of free radicals o oxidation within retinal tissues Another theory—areas of decreased vascular perfusion in retina, lead to cell death Two Types Dry (atrophic) o 90% of those diagnosed Wet (exudative) o 10% of those diagnosed o But accounts for 90% of blindness caused by disease Symptoms None Blurred vision Metamorphopsia— straight lines appear wavy or distorted Scotomas—missing areas in vision Dry Form Slow, progressive loss of central vision Breakdown of underlying retinal tissues, resulting in mottling or clumping of normal pigment Drusen begin to accumulate Geographic atrophy can also occur Wet Form Can quickly degrade central vision Break in underlying tissues allows new blood vessels or fluid to come through New blood vessels are weak so frequently break and bleed Treatment for Dry Form Regular eye exams Careful discussion regarding family history Education UV protection Antioxidants o AREDS o PreserVision Stop smoking Treatment for Wet Form Refer to retinal specialist Photocoagulation Photo-dynamic therapy (PDT) Submacular surgery Macular translocation Anti-angiogenic drug therapy Retinal Detachment Several types o Rhegmatogenous— caused by break in retina o Exudative—caused by fluid accumulation beneath retina o Tractional—proliferative fibrovascular vitreal strands Signs & Symptoms Flashing lights in peripheral vision New floaters—black spots or ‘cobwebs’ Peripheral scotoma—dark shadow or “curtain” blocking vision Emergency Patients with these symptoms must see eyecare provider immediately Additional risk factors o Highly nearsighted o Diabetic o Recent trauma/injury Treatment Laser photocoagulation or cryotherapy Pneumatic retinopexy— gas bubble to tamponade retina back into place Scleral buckle Silicone oil DIABETIC RETINOPATHY Diabetic Retinopathy Diabetes affects retinal microvasculature One of leading causes of blindness among ages 20-64 Progression Over time, elevated and fluctuating blood sugar damages vessel walls Vessels leak fluid, lipids or blood into retina New vessels grow to bring more oxygen to retina Symptoms Fluctuating vision Blurred vision Distortion Sudden loss of vision Treatment Control blood sugar Refer to retinal specialist when vision threatened PRP (pan-retinal photocoagulation) Focal laser Vitrectomy Retinal detachment repair Working Together Together we can catch vision threatening conditions earlier Glad to answer questions Always happy to take your calls Questions?