The Risk Manager's Role in Practitioner Credentialing
advertisement

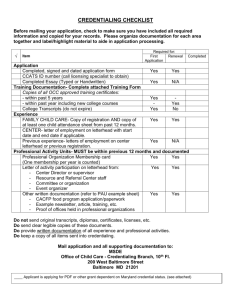
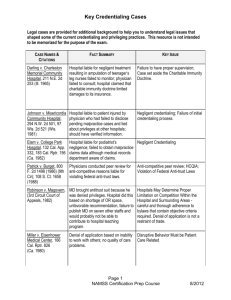
The Risk Manager’s Role in Practitioner Credentialing WHO ARE THESE PEOPLE? When you go to the hospital seeking medical care, how do you know that the doctors are properly trained, licensed, and qualified to take care of you? Why Credential? Patient Safety Risk Management - Negligent Credentialing Accreditation and Regulatory Requirements Definitions Credentialing – The process of collecting, assessing and validating the qualifications and credentials against established criteria. Privileging – The process health care organizations use to determine the specific procedures and treatments each health care practitioner may perform based on training and current competence. Judgment Criminal Education Patient Care Background Staff Competence Complaints Communication Skills NPDB Practice Based Learning Patient Complaints Medical Work History Professionalism Knowledge System Based Practice Training Claims History Technical Skills Health Negligent Credentialing Negligence is conduct that is culpable because it falls short of what a reasonable person would do to protect another individual from a foreseeable risk of harm Organizations can be found liable for negligent credentialing Negligent Credentialing Cases Darling v Charleston Memorial Community Hospital, 211 N.E. 2d 253 (Ill. 1965) Hospital liable for negligent treatment resulting in amputation of teenager’s leg. Nurses failed to monitor; physician failed to consult; hospital claimed charitable immunity doctrine-court ruled against hospital for failure to provide proper supervision. Errors in Credentialing Process Information Errors Process Errors Decision Errors Information Errors Information existed that could have been known but wasn’t, and the information would have impacted a credentialing decision Silos MSS Quality Risk Medical Records Information Errors Elam v College Park Hospital, 132 Cal. App. 332, 183 Cal. Rptr. 156 (Ca. 1982): Hospital liable for podiatrist’s negligence; failed to obtain malpractice claims data, even though medical records department was aware of claims-court ruled negligent credentialing. Significant Court Decisions Johnson v Misericordia Community Hospital, 294 N.W. 2d 501, 97 Wis. 2d 521 (Wis. 1981) Hospital liable to patient injured by physician who had failed to disclose pending malpractice cases and lied about privileges at other hospitals; should have verified information-court ruled negligent credentialing; failure of initial credentialing process Process Errors Failing to follow bylaws, regulations and/or policies Not consistently applying processes, requirements and criteria Adopting an unreasonable policy and/or criteria Lawrence R. Poliner, MD v. Texas Health Systems, James Knochel, MD Upon review, the advisory committee recommended a temporary restriction of Dr. Poliner's cardiac catheterization lab privileges for up to 15 days. Dr. Poliner agreed in writing after he was told he would receive a summary suspension of all his privileges if he didn't agree to the penalty. Dr. Poliner brought federal and state antitrust claims, along with tort and breach of contract claims, against the defendants. A lengthy legal battle ensued, the result of which has significant meaning for those administering peer review and the physicians under evaluation. Lawrence R. Poliner, MD v. Texas Health Systems, James Knochel, MD The jury determined the defendants weren't entitled to federal or state immunity. Jurors awarded Dr. Poliner more than $360 million in damages, $90 million of which were for alleged mental anguish and injury to career and reputation on Dr. Poliner's defamation claims and $110 million of which were for punitive damages. The district court reduced the defamation damages to $22.5 million to comply with the law. Prejudgment interest added up to more than $11 million, making the total award more than $33 million. Lawrence R. Poliner, MD v. Texas Health Systems, James Knochel, MD On July 23, 2008, the 5th Circuit Court of Appeals reversed the federal trial court's judgment and ruled for the hospital and Dr. Knochel based on federal immunity for their actions. Dallas attorney Lewis Lefko, JD, said the Poliner case sends a message to entities conducting peer review that they should make every effort to follow their bylaws and treat physicians fairly. "The Poliner case says that if you don't do it right, it may not look reasonable to a physician or to a jury," he said. Decision Errors The necessary information was known, but medical staff leaders failed to make a wise decision. Failure to address concerns identified in the credentialing & recredentialing process. One red flag may not be a problem or concern in itself but more than one suggests closer scrutiny. Kadlec Medical Center v. Lakeview Anesthesia Associates, 2005 WL 1155768, 2 (E.D. La. 2005) Dr. Berry was known to have diverted controlled drugs for personal use at an Alabama hospital and appeared to have been under their influence when on duty. He was fired and lost privileges. Hired in Washington State. Harmed a patient (a young women in a non-responsive vegetative state) as a result of drug abuse problem. Kadlec Medical Center v. Lakeview Anesthesia Associates, 2005 WL 1155768, 2 (E.D. La. 2005) Kadlec Medical Center v. Lakeview Anesthesia Associates, 2005 WL 1155768, 2 (E.D. La. 2005) Best Practices Provide correct information when responding to verification requests Don’t omit key information when providing verifications Address letter to Credentialing and/or MEC Sign as Agent of MEC Best Practices In addition to viewing a government issued photo identification, send the applicant’s picture with reference and training requests. Why? “Dr.” Gerald Barnes legally changed his name in the 1970’s to Gerald Barnes, the name of a licensed physician who was practicing in Stockton, California. He obtained copies of Dr. Barnes’ records and medical credentials and used the documents to obtain employment at numerous medical clinics and offices in Southern California. Best Practices Verify all clinical work history (when possible). Request information from past groups as well as hospitals Why? Michael Swango, M.D. In 1985, he was convicted of aggravated battery for the non-fatal poisoning of co-workers at an ambulance service. He spent 30 months in prison and lost his medical license. Despite his record, he was able to get jobs at hospitals in South Dakota, Virginia, New York and Zimbabwe. He is believed to have killed as many as 35 patients and is suspected in more than 60 deaths. “Blind Eye: The Story of A Doctor who Got Away with Murder” by James Stewart. Best Practices Include practitioner’s picture in notices to departments. Clinical areas should have access to privileges granted to each practitioner Pictures included with privileging information Best Practices Why? “Dr.” Ofari Mays October 2005, Orlando Florida – Mr. Mays was arrested and accused of impersonating a doctor. He spent days at Orlando Regional Medical Center dressed in scrubs and lab coat. He had access to the hospital, reviewed patient records and discussed treatments with nurses and other doctors. Best Practices Sharing of information between hospitals MS.06.01.05 EP 9 Before recommending privileges, the organized medical staff also evaluates the following: Relevant practitioner-specific data as compared to aggregate data, when available Morbidity and mortality data, when available NAMSS PASS NAMSS PASS™ is a secure, online database that provides quick, easy, and inexpensive access to the affiliation history of practitioners and is the first and only universal resource for tracking practitioner affiliation history. NAMSS PASS NAMSS PASS NAMSS PASS Best Practices Google applicants Sharing of information medical staff, quality and risk management within organization Self query NPDB Don’t deny privileges –table requests pending documentation. NPDB Continuous Query Program Additional reference Document current competence at reappointment. Risk Managers Advocate for education and training for medical staff professionals and medical staff leaders Encourage networking with other medical staff professionals Champion certifications for medical staff professionals Open communication with medical staff professionals Risk Managers Review credentialing policies and processes Review reference, affiliation, and training verification forms Review and collaborate on wording of sensitive topics and discussions in meeting minutes Review and collaborate on sensitive affiliation verification responses