2 - SN-DD
advertisement

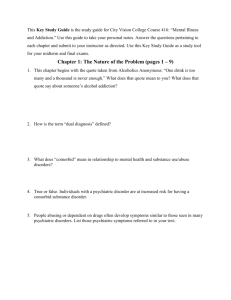
Integrated Treatment for Dual Disorders Kim Mueser, Ph.D. Dartmouth Medical School NH-Dartmouth Psychiatric Research Center Kim.t.mueser@dartmouth.edu Overview • • • • • • • Epidemiology Why focus on dual disorders? Models of etiology Assessment Treatment principles Research Avoiding the blame/demoralization trap Any Substance Use Disorder Prevalence % of Substance Use Disorder 60 50 40 30 20 10 0 Gen.Pop Schiz BPD MD OCD Phobia PD Rates of Lifetime Substance Use Disorder (SUD) among Recently Admitted Psychiatric Inpatients (N=325) (Mueser et al., 2000) % of Clients with SUD 100 75 50 25 0 Schizophrenia Schizoaffective Disorder Bipolar Disorder Major Depression Factors Influencing Prevalence of Substance Use Disorders (SUD): Client Characteristics Higher Rates • Males • Younger • Lower education • Single or never married • Good premorbid functioning • History of childhood conduct disorder • Antisocial personality disorder • Higher affective symptoms • Family history SUD Factors Influencing Prevalence of Substance Use Disorders: Sampling Location Higher Rates • Emergency rooms • Acute psychiatric hospitals • Jails • Homeless • Urban setting (drugs) • Rural setting (alcohol) Major Subgroups of Comorbid Clients • Severely mentally ill - psychotic Frequently abuse moderate amounts of substances Small amounts of substance use trigger negative consequences • Anxiety and/or depression Substance use can cause or worsen symptoms Frequently abuse moderate to high amounts of substances • Personality Disorders Antisocial & borderline most common Frequently abuse high amounts of substances Clinical Epidemiology 1. Rates higher for people in treatment 2. Approximately 50% lifetime, 25% 35% current substance abuse 3. Rates are higher in acute care, institutional, shelter, and emergency settings 4. Substance abuse is often missed in mental health settings Why Focus on Dual Disorders? 1. Substance abuse is the most common cooccurring disorder in persons with severe mental disorders 2. Significant negative outcomes related to substance abuse: 1) Clinical relapse & rehospitalization 2) Demoralization 3) Family stress 4) Violent behavior 1) Incarceration 2) Homelessness 3) Suicide 4) Medical illness 5) Infections diseases 6) Early mortality 3. Outcomes improve when substance abuse remits 4. Poor treatment is expensive for families and society Reasons for High Comorbidity Rates of Severe Mental Illness and Substance Abuse • Berkson’s Fallacy • Self-medication* • Super-sensitivity to effects of substances* • Socialization motives • Precipitation of psychosis from substance use • Common factors Poverty/deprivation Neurocognitive impairment Conduct disorder/antisocial personality disorder Self-Medication: More symptomatic clients don’t abuse more substances Substance selection unrelated to type of symptoms experienced Types of substances abused unrelated to psychiatric diagnosis Self-medication may contribute to some comorbidity but doesn’t explain all More evidence supporting self-medication in anxiety disorders (PTSD) Super-sensitivity Model: Biological sensitivity increases vulnerability to effects of substances Smaller amounts of substances result in problems “Normal” substance use is problematic for clients with severe mental illness but not in general population Sensitivity to substances, rather than high amounts of use, makes many clients with mental illness different from general population Stress-Vulnerability Model Medication Substance Abuse Biological Vulnerability Severity of SMI Stress Coping Status of Moderate Drinkers with Schizophrenia 4 - 7 Years Later (N=45) 100% 80% 60% 55.6 40% 20.0 20% 24.4 0% Abstinent Moderate Drinker Source: Drake & Wallach (1993) Alcohol Use Disorder Support for Super-sensitivity Model: Dual disorder clients less likely to develop physical dependence on substances Standard measures of substance abuse are less sensitive in clients with severe mental illness Clients are more sensitive to effects of small amounts of substances Few clients are able to sustain “moderate” use without impairment Super-sensitivity accounts for some increased comorbidity Overview of Assessment of Substance Abuse in Clients with Severe Mental Illness Detection Classification Functional Assessment Functional Analysis Treatment Planning • Psychological Dependence - Use of more substance than intended, unsuccessful attempts to cut down, giving up important activities to use substances, or spending lots of time obtaining substances. • Physical Dependence - Development of tolerance to effects of substance, withdrawal symptoms following cessation of substance use, use of substance to decrease withdrawal symptoms. Functional Assessment • Goals: To understand client’s functioning across different domains and to gather information about substance use behavior • Domains of Functioning 1. Psychiatric disorder 2. Physical health 3. Psychosocial adjustment (family & social relationships, leisure, work, education, finances, legal problems, spirituality) • Dimensions of Substance Abuse 1. 6-Month Time-Line Follow-Back Calendar 2. Substances abused & route of administration 3. Patterns of use 4. Situations in which abuse occurs 5. Reported motives for use • Social • Coping • Recreational • Structure/sense of purpose 6. Consequences of use Evaluating Social Factors Associated with Substance Abuse • Does person have non-substance abusing peers? • Can person resist offers to use substances? • Is the person lonely? • Can the person initiate and maintain conversations? • Is person able to get others to respond positively to him/her? • Can the person express feelings? Resolve conflicts? Common Symptoms Associated with Self-Medication • • • • • • Depression, suicidal thoughts Anxiety, nervousness, tension Hallucinations Delusions of reference & paranoia Sleep disturbance Mania/hypomania Recreational Skills and Substance Abuse • • • • What does the person do for fun? Hobbies? Sports? What is person’s involvement with others in recreational activities? • Does the person not participate in activities which he/she previously did? Functional Analysis • Goal: To identify factors which influence or control substance use behavior • Characteristics of Useful Functional Analyses 1. Focus on behaviors, NOT stable traits 2. Constructive, NOT eliminative 3. Contextual, NOT mechanistic 4. Examines maintaining factors, NOT etiological factors 5. Leads to hypotheses that can be tested by treatment & modified, NOT theories that remain unchanged regardless of outcome 6. Change usually doesn’t happen magically on its own •Constructing a Payoff Matrix 1. List advantages & disadvantages of using substances, & advantages & disadvantages of not using substances in Payoff Matrix 2. Use all available information from functional assessment 3. Consider advantages & disadvantages from the client’s perspective 4. View different reasons listed as hypotheses about maintaining factors, not established facts; reasons may change as new information emerges 5. If client is using, the pros of using & cons of not using should outweigh the pros of not using and cons of using Pay-Off Matrix Using Substances Advantages Disadvantages Not Using Substances Common Advantages and Disadvantages of Using Substances and Not Using Substances Using Substances Not Using Substances Advantages Feels good Acceptance & friendship when using with peers Decreased social anxi ety Feel "normal" when using with others Escape from b elief one is a "failure" or has not lived up to expectations Relief from d epression or anxiety Reduction or distraction from h allucinations Help getting to sleep Improved attention & concentration Decreased medica tion side effects Something to look forward to Reduction in craving or withdrawal symptoms Better relationships with significant others Stable & independent housing Improved control & stability of psychiatric illness Financial stability & control over one's money Stay out of jail/prison Minimize d exposure to infectious diseases & better management of medical illnesses Reduced exposure to trauma Improved ability to pursue goals & meet major role obligations (worker, student, spouse, parent) Better social relationships, including intimate relationships, with people who really care No physical dependence Disadvantages Conflict with significant others Housing instability & homelessness Relapses & rehospitaliza tions Financial problems Legal problems Infectious diseases & other me dical illnesses Increased exposure to trauma Inability to pursue goals & meet major role obligations (worker, student, spouse, parent) Physical dependence leading to need for greater amo unts Sociopathic or crimi nal socia l network Lac k of an intimate relationship Increased hallucinations or paranoia Lac k of positive feelings Awkwardness or peer p ressure from friends who use substances Social i solation because no friends who don't use Social an xiety Feel "abnormal" because of stigma from mental illness Confrontation with belief that one is a failure Persistent depression or anxiety Distress due to hallucinations Poor attention & concentration Troubling medication side effects Nothing to do or look forward to Cravings or withdrawal symptoms Examples of Interventions Based on the Payoff Matrix Using Subs tances Not Using Substance s Advan tages Naltr exone Disulfir am Contingen t reinforcement Comm unit y reinforcement Motivationa l i ntervie wing Dec isi ona l balance me thod Educa tion abou t dua l dis orders Persua sion g roups Disadvan tage s Disulfir am Financ ial paye eship Cond iti ona l discha rge from psychiatric hosp it al Probation or parole cond ition Skil ls training for social competence Identifying new social out le ts Teaching skill s for coping wit h d ist ressful symptoms Pharmacological treatment of distressful symp toms Deve loping alt ernative recreationa l activities Creating new & meaning pursuit s (e.g., work , schoo l, parenting) Teaching strategies for coping wit h cravings Treatment Planning • Goals: To determine which interventions are most likely to be effective and how to measure outcome • Steps 1. Engage the client and significant others 2. Assess motivation to change 3. Select target behaviors, thoughts, emotions to change 4. Identify interventions to address targets: select at least 1 strategy to enhance motivation & 1 strategy to address needs currently met by substance use 5. Choose measures to assess effects of intervention Treatment Barriers • Historical division of service and training • Sequential and parallel treatments • Organizational and categorical funding barriers in the public sector • Eligibility limits, benefit limits, and payment limits in the private sector Integrated Treatment • Mental health and substance abuse treatment Delivered concurrently By the same team or group of clinicians Within the same program The burden of integration is on the clinicians Other Features of Dual Disorder Programs • Assertive outreach • Stage-wise treatment: engagement, persuasion, active treatment, and relapse prevention • Long-term commitment • Comprehensive treatment • Reduction of negative consequences What are the Stages of Treatment? 1. Engagement, persuasion, active treatment, and relapse prevention 2. Not linear 3. Stage determines goals 4. Goals determine interventions 5. Multiple options at each stage What Do We Do During Engagement? • Goal: To establish a working alliance with the client • Clinical Strategies 1. Outreach 2. Practical assistance 3. Crisis intervention 4. Social network support 5. Legal constraints What Do We Do During Persuasion? • Goal: To motivate the client to address substance abuse as a problem • Clinical Strategies 1. Psychiatric stabilization 2. “Persuasion” groups 3. Family psychoeducation 4. Rehabilitation 5. Structured activity 6. Education 7. Motivational interviewing What Do We Do During Active Treatment? • Goal: To reduce client’s use/abuse of substance • Clinical Strategies 1. Self-monitoring 2. Social skills training 3. Social network interventions 4. Self-help groups 5. Substitute activities 6. Close monitoring 7. Cognitive-behavioral techniques to address: High risk situations Craving Motives for substance use Socialization Persistent symptoms Pleasure enhancement What Do We Do During Relapse Prevention? • Goals: To maintain awareness of vulnerability and expand recovery to other areas • Clinical Strategies 1. Self-help groups 2. Cognitive-behavioral and supportive interventions to enhance functioning in: Work, relationships, leisure activities, health, and quality of life Relapse Prevention Strategies • Construction a relapse prevention plan: – Risky situations – Early warning signs – Immediate response – Social supports – Abstinence violation effect Recovery Mountain • Combat demoralization related to relapses • Reframe relapses as part of road to recovery • Don’t loose sight of gains made between relapses • Learning experience, modify relapse prevention plan Stages of Substance Abuse Treatment 1. Pre-engagement: No contact with a counselor. 2. Engagement: Irregular contact with a counselor. 3. Early Persuasion: Regular contact with a counselor, but no reduction in substance abuse. 4. Late Persuasion: Regular contact with a counselor and reduction in substance use (< 1 month). 5. Early Active Treatment: Reduction in substance use (> 1 month). 6. Late Active Treatment: No abuse for 1-6 months. 7. Relapse Prevention: No abuse 6-12 months. 8. Remission: No abuse for over one year. Research on Integrated Treatment (IT) • 26+ RCT or quasi-experimental studies of IT (reviewed by Drake et al., 2004) • 3/4 studies of brief motivational interviewing interventions showed positive effects • 6/7 studies found group intervention better than 12step or standard care Research on IT (Cont.) • Family intervention: no RCTs examining family treatment alone • Comprehensive IT: 2 RCT & 1 quasiexp. study favor comp. IT over treatment as usual • Intensity: more intensive IT produces slightly better outcomes (e.g., Drake et al., 1998) Drake et al. (1998) • • • • 203 clients (77% schizophrenia) ACT vs. standard case management (SCM) (both IT) 3 year follow-up ACT better than SCM in alcohol severity & stage of treatment • No differences in hospitalization, symptoms, quality of life NH Dual Diagnosis Study Proportion of Days in Stable Community Housing 1.0 0.9 0.8 0.7 Beginning 6 months 12 months All DD Patients (N = 203) 18 months 24 months 30 months 36 months Patients in Recovery (N = 54) 1. Proportion of days in stable community housing (regular apartment or house, not in hospital, jail, homeless setting or doubling with friends or family) increased for all dual diagnosis clients. 2. They increased more rapidly for persons in recovery (no substance abuse for at least 6 months). NH Dual Diagnosis Study Percentage of Persons Hospitalized 70.0 60.0 50.0 40.0 30.0 20.0 10.0 0.0 Beginning 6 months 12 months All DD Patients (N = 203) 18 months 24 months 30 months 36 months Patients in Recovery (N = 54) 1. Percentage of persons hospitalized during each six months declined significantly for all clients. 2. It declined much more for those in recovery. Fidelity to IT Model Improves Outcome Limitations of Research • • • • Lack of standardization of treatments No or limited fidelity assessment No replication of program effects Unclear or variable comparison conditions Avoiding the Blame/Demoralization Trap Don’t blame the client for substance abuse or relapses because: Substance abuse is a disorder for which clients are no more responsible than their primary psychiatric symptoms Clients with most severe substance abuse need professional help the most; many others improve spontaneously Remember that the clients are doing the best they can To avoid demoralization: Remember: integrated treatment works in the long run There is usually no obvious “best solution” Adopt a collaborative-empirical approach to treatment View relapses as an inevitable part of the recovery process Develop a case formulation based on a functional analysis to guide treatment