The kidneys and formation of urine
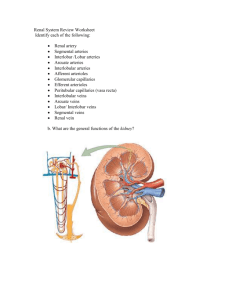
advertisement

Introduction -The important functions of kidney is: 1) To discard the body waste that are either ingested or produced by metabolism. 2) To control the volume and composition of body fluids. The functional unit of the kidney is the nephron which is responsible for the formation of urine. The nephron Each nephron has two major portions 1) Glomerulus (cluster of capillaries) [it is formed by a pair of afferent and efferent arterioles surrounded by [Bowman′s capsule]. 2) Renal tubules - which originates as a bulb called Bowman′s capsule. The renal tubule is made up of: i) Proximal (near) convoluted tubules ii) loop of Henle (ascending and descending limb) iii) Distal (far) convoluted tubule iv) Collecting duct formation of urine The formation of urine involves three major processes: 1) glomerular filtration, which takes place in the renal corpuscles. 2) Tubular reabsorption which take place in the renal tubules. 3) Tubular secretion which also take place in the renal tubules. 1)Filtration process: -The pressure of the blood within the glomerulus forces water and dissolved solutes through the semipermeable capillary membrane and into the Bowman′s space. - Approximately 120 ml/min of the renal plasma is filtered through the glomeruli forming ultrafiltrate which is further processed as it travels through the nephron. -The ultrafiltrate has the same composition as blood plasma but it is normally free of proteins and also cellular-free. -Some of the filtered products include water, glucose, electrolytes, amino acids, urea, uric acid, creatinine, and ammonia. -[The rate of filtration (the glomerular filtration rate) is an important indicator of renal function] How? 2) Tubular reabsorption: - As the ultrafiltrate (glomerular filtrate) passes through the proximal tubules, a large portion of the water, sodium chloride, bicarbonate, potassium, calcium, amino acids, glucose and other substances needed by the body are reabsorbed and pass back into the bloodstream. Like the proximal tubule, the descending limb of the loop of Henle is very permeable to water, but the resorption of solutes does not occur in this part of the loop. The ascending limb, however, is nearly impermeable to water, but there is active reabsorption of sodium chloride. In this section of the tubule and in the remaining tubule, hydrogen ion and ammonia are secreted. 3) Tubular secretion: It involves sending molecules from the blood capillaries into the tubular filtrate for excretion. (out of the body) - The tubular secretion process: ● removes unneeded foreign waste substances that are not filtered by the glomerulus including various medications and toxins. ● promotes secretion of hydrogen ions and other ions to help regulate acid – base and electrolytes balance. -Various ions are also secreted including hydrogen ions, ammonium ions, sodium ions, potassium ions, bicarbonate ions, uric acid and some weak acids and bases. - Hydrogen ions is secreted in the proximal and distal tubules. - Tubular secretion is caused mainly by active transport. Thus; by the selective reabsorption and secretion action of the renal tubules, the glomerular filterate modification leads eventually to excretion of urine that has a composition different from that of the glomerular filterate . -The glomerular filtrate enters the proximal tubules in an isotonic state. -In the proximal tubules, the reabsorption process begins. Water and salt ( Nacl) is reabsorbed. -At the descending limp of Henle, the water reabsorption continues osmosis (75% of water reabsorption occurs here ) and the water becomes more and more concentrated as it descends. -At the hairpin of Henles loop the fluid reaches the maximum concentration (becomes hypertonic) and the epithelium becomes water impermable, so water reabsorption Ceases. - the fluid continues ascending entering the ascending limb , which is impermeable to water ,and becomes progressively less concentrated due to Nacl reabsorption and will become isotonic then hypotonic at the end of the thick ascending limp of Henles loop . -In the distal tubules, active reabsorption of Nacl continues to a less extent . - both the distal convoluted tubule and the collecting tubules are sensitive to stimulation by the ADH (anti diuretic hormone). Thus their major function is to reabsorb water only to the extent required by the body. Role of kidneys in the regulation of acid – base balance: Body fluids are maintained within a narrow range that is slightly alkaline. -The normal PH of arterial blood is between 7.35 and 7.45 - If the blood PH rises above 7.45 , a person said to have alkalosis. - If the blood PH decreases below 7.35 , a person said to have acidosis. -Acids are continually produced during metabolism, so kidneys help maintain a normal PH by either excreting or retaining acids and bases. ● If the blood is acidic, hydrogen ions are excreted ( out of the body) and bicarbonate ions are reabsorbed. ● If the blood is basic, hydrogen ions are not excreted (reabsorbed) and bicarbonate ions are not reabsorbed. ( excreted) ● The ammonia that is secreted combines with the hydrogen ions to form ammaonium ions in the tubular lumen and this helps to regulate the hydrogen ions conc. of the urine. ● Hydrogen ions are produced as waste from the metabolism and are generally secreted. -Bicarbonate can also be secreted but is more often reabsorbed (usually up to 100%) to help maintain the proper blood PH. [The urine is usually acidic, so it follows that an excess of hydrogen ions is usually excreted. - Ammonia provides another means of buffering and removing the hydrogen ions in urine: H+ +NH3 NH4+ - Ammonia is produced in tubule cells by the deamination of amino acids. Three basic renal processes The substance is freely filtered but is also partly reabsorbed from the tubules back into the blood. For each substance in the plasma, a particular combination of filtration, reabsorption, and secretion occurs. The rate at which the substance is excreted in the urine depends on the relative rates of these three basic renal processes. Filtration, Reabsorption, and Secretion of Different Substances In general, tubular, reabsorption is quantitatively more important than tubular secretion in the formation of urine, but secretion plays an important role in determining the amounts of potassium and hydrogen ions and a few other substances that are excreted in the urine. Most substances that must be cleared from the blood, especially the end products of metabolism such as urea, creatinine, uric acid, and urates, are poorly reabsorbed and are, therefore, excreted in large amounts in the urine. Certain foreign substances and drugs are also poorly reabsorbed but, in addition, are secreted from the blood into the tubules, so that their excretion rates are high. Filtration, Reabsorption, and Secretion of Different Substances Nutritional substances, such as amino acids and glucose, are completely reabsorbed from the tubules and do not appear in the urine even though large amounts are filtered by the glomerular capillaries. Each of the processes - glomerular filtration, tubular reabsorption, and tubular secretion - is regulated according to the needs of the body. Glomerular filtration rate (GFR): The glomerular filtration rate (GFR) is the amount of renal filtrate formed by the kidneys in 1minute, and averages 100 to 125 mL per minute. ● GFR: will lead to the inefficient elimination and accumulation of the body waste products and toxins. ● GFR: can lead to insufficient time for proper reabsorption. Estimation of the GFR is used to assess the kidney function. Example of kidney function test: creatinine clearance test. What is creatinine? The main storage compound of high energy phosphate needed for muscle metabolism. Creatine H2O Creatinine (Waste product) Creatinine: anhydride of creatine! Jaffe´ reaction for measuring creatinine Creatinine + alkaline picrate solution Bright orange/red colored complex absorbs light at 485nm Normal creatinine clearance test Blood creatinine: Men: 0.6-1.2 milligrams per deciliter (mg/dL) or 71-106 micromoles per liter (mcmol/L) Women: 0.4-1.0 mg/dL or 36-90 mcmol/L Creatinine clearance: Men (younger than 40 years): 107-139 milliliters per minute (mL/min) or 1.8-2.3 milliliters per second (mL/sec) Women (younger than 40 years): 87-107 mL/min or 1.5-1.8 mL/sec Creatinine clearance values normally go down as you get older (normal values go down by 6.5 mL/min for every 10 years past the age of 20). Tubular reabsorption Tubular secretion