5.1 mA
advertisement

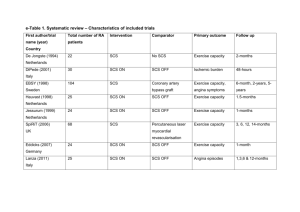
Neuromodulation; A new Frontier for Neuroradiologists Bassem A. Georgy, M.D., North County Radiology Assistant Clinical Professor, University of California, San Diego Financial Disclosure • Consultant; DePuy Spine, Arthrocare Inc., Dfine • Advisory Board; Osseon LLC, Spine Aligns • Multiple pending Patents Overview • • • • • History Gate Theory Indications Implantation techniques SCS and Neuroradiology What is Neurostimulation? • Delivery of electrical impulses to the spinal cord to block pain signals transmission • Induce Paresthesia • Patient feels a tingling sensation in the usual area of pain • Any kind of neuropathic pain refractory to other treatments and not candidate for further surgical procedures Types of Pain • Neuropathic Pain – Radiculopathy – Herpetic Neuropathy – Diabetic Neuropathy • Nociceptive Pain – Discogenic pain – Facet and SI pain • Mixed Pain – FBSS – Cancer pain What is a Spinal Cord Stimulator? • Electrical lead implanted in the epidural space • Lead is tunneled under the skin • Lead is connected to a charger that is implanted in a subcutaneous pocket • Patient control the charger from outside Types of SCS Procedures • SCS trial – Subcutaneous lead implantation and outside charger • Percutaneous implantation – Subcutaneous lead implantation, subcutaneous pocket for charger • Surgical implantation – Laminectomy for lead implantation Gate Control Theory -Proposed by Melzack & Wall in 1965 -A non-painful stimulus that acts likes gates can block the transmission of a painful stimulus. The Gate Control Theory • There is a gate in the spinal cord that controls the flow of noxious pain signals to the brain. • The theory suggests that the body can inhibit these pain signals or "close the gate" by activating certain nonnoxious nerve fibers in the dorsal horn of the spinal cord. • The neurostimulation system, implanted in the epidural space, stimulates these pain-inhibiting nerve fibers, masking the sensation of pain with a tingling sensation (paresthesia) • Stimulate the large diameter A fibers not small C fibers Mechanism of Action • • • • GABAergic effects Dorsal Column Stimulation Increased blood flow Neurotransmitters metabolites concentration in the CSF Indications • • • • • • • • Failed back surgery Syndrome RSD Arachnoiditis Peripheral Neuropathy Axial pain Post herpetic Neuralgia Peripheral Vascular diseases Angina Percutaneous Lead Placement • • • • • • Local anesthesia Insert 14G Touhy needle into the epidural space Confirm needle location with fluoroscopy and loss of resistance Introduce guidewire Insert lead Confirm lead location with fluoroscopy 13 13 Dual Lead Placement • Insert second needle one level below/contralateral to first • Place lead tips at same level or staggered 18 18 Intraoperative Screening • • • Connect lead and screener Test by trying different electrode combinations and polarities Goal of matching stimulation to pain pattern 22 22 CURRENT STEERING Lateral Steering Longitudinal Steering CASE STUDY • 45 year-old male with bilateral leg and lower back pain • (red indicates pain pattern) • Implanted with dual Octrode leads and an Eon rechargeable IPG T-8 • Stim-set 1 uses a bipole and 5.1 mA current to cover the right leg pain • (light blue indicates paresthesia) + 5.1 mA • Stim-set 1 remains running • Stim-set 2 uses a guarded cathode and 4.6 mA current to capture the left calf • Current needs to be steered cephalad to capture the left leg pain + 4.6 mA + + 5.1 mA • Stim-set 1 remains running • Stim-set 2 steers current up one electrode to capture the entire left leg at 6.0 mA • Patient does not like stimulation in the left calf 6.0 mA - - + 4.6 mA + 5.1 mA • Stim-set 1 remains running • Stim-set 2 focuses the 6.0 mA current by using a guarded cathode to pull stimulation out of the left calf 6.0 mA + + + 5.1 mA • Stim-sets 1 and 2 remain running • Stim-set 3 covers the lower back pain • Now, the current levels to each stimset need to be optimized with Active Balancing™ 7.1 mA + 6.0 mA + + + 5.1 mA Test Stimulation • • • Lead secured to skin Allows for test stimulation of several days Success is defined if more than 50% pain relief 30 30 Goals of the Trial Evaluation The goals of the trial evaluation period (several days) are to • evaluate the effect that SCS therapy has on – pain – opioid use – function and activity levels • determine the patient’s – electrical energy requirements – optimal parameter settings • The goal is at least a 50% reduction in pain without intolerable side effects Permanent Percutaneous Implantation 1. Successful trial 2. Percutaneous lead placement • • • Lead anchored to supraspinous ligament Retest the patient Extension externalized 32 32 Permanent Percutaneous Implantation • Employ local anesthetic for tunneling path • Create stab wound on flank • Tunneling to flank • Pass extension through stab wound 33 33 Permanent Percutaneous Implantation • • • Pocket site identified and created Extension connected with lead Pocket creation for connector and excess lead 34 34 Permanent Percutaneous Implantation • • • • • Neurostimulator/extension connection Implant neurostimulator in pocket X-rays for system visualization Incisions closed Settings optimized with external programmer 35 35 SCS in the IR: Things You Will Need Surgical Instruments • • • • • • • Scalpel Bovey Suction Scissors Grabbers Retractors Suture/Closures Sutures • Non absorbable Tichron (0. 2-0) Silk • Absorbable Dexon (3-0) Moncril (4-0) SCS in the IR: Things You Will Need Programmer Post Procedural • Antibiotics Ancef 1 gm 7-10 days • Post procedural pain Resume prior pain meds • # to call for problems • Appt. for f/u programming, wound recheck Complications –Infection –Lead dislodgment –Loss of functionality –Lead fracture –Surgical revision for reduction or loss of pain relief –Interference may be caused by MRIs and other radio frequency devices 41 41 SCS and Interventional Radiology • Can I do it ? • Training – Medtronic, ANS, Advanced Bionics • Reimbursement • Privileges • SCS clinical Service Peripheral SCS SCS Service • • • • • • • • Consultation Trial Remove lead Assess trial and check wound Permanent placement Check would Follow up Office, nurse (PA) , support staff