Module 4: Nursing Homes
advertisement

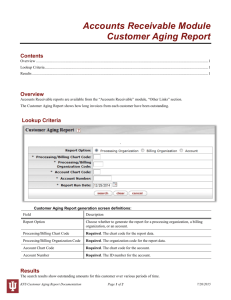
Module 8: Trends in Older Adult Services Aging Services of Minnesota Older Adult Services Orientation Manual © Aging Services of Minnesota 2014 1 Acknowledgements This resource was made possible by funding from the Ronald Patterson Governance Fund of the Aging Services of Minnesota Foundation Developed by Health Dimensions Group, Minneapolis, MN TERMS OF USE Aging Services of Minnesota (Aging Services) is the sole and exclusive owner of and retains all rights to this Orientation Manual (“Manual”) and all associated registrations. Aging Services makes this Manual available free of charge only to its members on the Members Only section of the Aging Services website, which is password protected. Member representatives are authorized to use any or all of this Manual only in the performance of duties and responsibilities on behalf of the member organization. The contents of the Manual may be customized to meet the needs of the member organization, and copies of any portion of the Manual may be distributed within the member organization. In every other respect, members and member representatives may not: (i) alter the Manual; (ii) add to the Manual; (iii) update the content of the Manual; (iv) distribute reproductions of the Manual to any person or organization not a member of Aging Services; (v) borrow portions of the Manual for use in other works; (vi) make derivative works; or (vii) be identified as an author of the Manual. © Aging Services of Minnesota 2014 2 Older Adult Services © Aging Services of Minnesota 2014 3 Trends Internal and external forces shaping the future of older adult services: Person-Centered Care Movement Technology to Support Aging in Place Shift in Funding to HCBS Affordable Care Act: Health Care Reform Alliances Between Hospitals and PAC © Aging Services of Minnesota 2014 4 Trend #1: The Person-Centered Care Movement Culture Values Goals Family Situation C Needs hoice Preferences P M urpose eaning Culture change = national movement for the transformation of older adult services, based on person-centered values © Aging Services of Minnesota 2014 5 Trend #1: The Person-Centered Care Movement The Green House® Project Small house neighborhood model for more intimate living environment Promotes privacy, dignity, independence, and mobility for improved quality of life More than 260 Green House Homes in 32 states © Aging Services of Minnesota 2014 6 Trend #1: The Person-Centered Care Movement Palliative Care Model Comfort care for those with chronic or terminal illness Relief from pain and suffering Palliative Care © Aging Services of Minnesota 2014 Physical, emotional, social, and spiritual dimensions of health 7 Trend #1: The Person-Centered Care Movement myPotential© Rehabilitation Program A person-centered rehab model developed by The Village at Rockville, a nursing home provider in Rockville, MD Person-centered features of the program include the myStay© personal care plan, concierge services, private rooms, and a therapy care team © Aging Services of Minnesota 2014 8 Trend #2: Technology to Support Aging in Place Both an Opportunity and a Threat Consumers indicate a strong desire to remain independent and in the home as long as possible. The use of technology to support independence in home and community-based settings is a growing enterprise. Technology presents aging services providers with the opportunity to innovate, expand service lines, and broaden market share. Technology may also pose a threat to aging services providers that do not innovate. Competitor technology offerings may serve as an innovative alternative to traditional services offerings. © Aging Services of Minnesota 2014 9 Trend #2: Technology to Support Aging in Place Healthsense launches eNeighbor® Many senior living providers are using technology to extend services outside their walls Healthsense eNeighbor® uses sensors in the home to learn the behavior of residents and automatically issue alerts when unexpected changes occur Sensor monitoring systems like eNeighbor have the potential to help prolong the time that individuals with Alzheimer's or other types of dementia are able to live at home or with family members. eNeighbor ® Monitoring System © Aging Services of Minnesota 2014 10 Trend #2: Technology to Support Aging in Place LG and Thrive Senior Living Partnership between LG, an electronics and telecom company, and Thrive Senior Living, an owner and operator of senior housing communities Provide Smart Senior Living Solutions – a suite of technologies that integrate an assisted living resident’s health information into one platform Smart walkers and wheelchairs currently under development by LG © Aging Services of Minnesota 2014 11 Trend #2: Technology to Support Aging in Place Aetna and Addus Home Care Smart Phones Health plan provider Aetna and home care provider Addus partner to conducting a pilot study–impact of providing smart phones to home care aides © Aging Services of Minnesota 2014 12 Trend #3: Funding Shift to HCBS There is a continued shift of Medicaid Long-Term Care (LTC) funding from institutional to home- and communitybased. Medicaid is the primary source of LTC funding. Kaiser Family Foundation indicates Medicaid is in a historic time of transformation. Factors shaping Medicaid today: Affordable Care Act Delivery and Payment System Reform BILLION Medicaid Economic Conditions © Aging Services of Minnesota 2014 $123 Amount of funding Medicaid program provided for LTC in the United States during 2012 Cost Containment & Program Improvements 13 Trend #3: Funding Shift to HCBS Medicaid LTC Spending in United States United States Medicaid LTC Expenditures Care Center 2012 55.0% HCBS 45.0% 15% increase in HCBS spending 2000 70.0% 30.0% *Care center includes institutional care settings 14 Trend #3: Funding Shift to HCBS Medicaid LTC Spending in Minnesota Minnesota Medicaid LTC Expenditures Care Center 2012 HCBS 67.7% 32.3% 20% increase in HCBS spending 2000 87.7% 12.3% *Care center includes institutional care settings 15 Trend #3: Funding Shift to HCBS Impact on Occupancy The impact of this trend is evident by continued declines in care center occupancy across the country Care Center Occupancy 95% Providers can expect Medicaid funding for care centers to continue to decrease and a continued emphasis on HCBS 90% 85% 80% 2004 2005 © Aging Services of Minnesota 2014 2006 US 2007 2008 2009 2010 Minnesota 16 2011 2012 Trend #4: Affordable Care Act: Health Care Reform The Triple Aim Improve Patient Experience TRIPLE AIM Improve Population Health © Aging Services of Minnesota 2014 Lower Costs 17 Trend #4: Affordable Care Act: Health Care Reform Value-Based Payment Value-based payment is an emerging payment model, driven by health care reform, in which the payment to health care providers is determined by the quality of outcomes Value-based payment has a measurable impact on the triple aim Lower cost Improved quality © Aging Services of Minnesota 2014 18 Trend #4: Affordable Care Act: Health Care Reform Value-Based Payment in Post Acute Care President Obama’s FY 2015 budget includes value-based purchasing for skilled nursing facilities and home health agencies beginning 2018 It proposes at least 2% of payments to be tied to the quality and efficiency of care Quality metrics will include: • Avoidable re-hospitalizations • Percentage of Medicare discharged home 19 Trend #4: Affordable Care Act: Health Care Reform Bearing Financial Risk through Bundled Payment Bundled payment is a health care reform driven payment model in which providers are responsible for a patient’s healthcare costs over an episode of care Post Acute Care Episode Bundling (BPCI Model 3) Specialty Care Physicians Outpatient Hospital and Ambulatory Care Inpatient Hospital Acute Care Inpatient Rehab and Long-Term Acute Hospital Skilled Nursing Facility Acute Care Episode with PAC Bundling (BPCI Model 2) © Aging Services of Minnesota 2014 20 Home Health and Hospice Trend #4: Affordable Care Act: Health Care Reform Reduce PAC Spending via Bundled Payment Billions At least 50% of Total PAC Provider Payments will be Bundled by 2021 Reduce PAC Spending by 2.85% $35 $30 $25 $20 $15 $10 $5 $0 2013 2015 2017 2019 2021 BPCI begins for all PAC providers BPCI pilot began 21 Trend #4: Affordable Care Act: Health Care Reform Narrowing Preferred Provider Networks Acute Care Preferred Provider Network Hospital/Network Providers Providers driving PAC referrals PAC Preferred Providers “Value” Providers 22 PAC Non-Preferred Providers Low-Quality, High-Cost Providers Trend #5: Alliances Between Hospitals and PAC Partnership Developments Alliances are developing between hospitals and post-acute providers “Policymakers and health care providers increasingly recognize that coordination between acute care hospitals and post-acute providers is essential to achieve quality health outcomes and ultimately better manage episodes of care.” Rich Umbdenstock President & CEO, American Hospital Association “Long-term care facilities were among the best partners for hospitals to lower their preventable readmission rates, a new survey shows.” “Partnering with long-term care and skilled nursing facilities was a chief strategy among 64% of senior hospital leaders working to limit preventable hospital readmissions.” Senior Housing News Survey from HealthLeaders Media Intelligence Unit © Aging Services of Minnesota 2014 23 Trend #5: Alliances Between Hospitals and PAC Examples Amedisys Home Health and Monongahela Valley Hospital Allina Health and Minnesota Care Centers Partner to reduce hospital readmissions Enter a joint venture to increase clinical integration Kindred HealthCare and Cleveland Clinic Participate in bundled (value-based) payment demonstration © Aging Services of Minnesota 2014 24 Trend #5: Alliances Between Hospitals and PAC Amedisys Home Health and Monongahela Valley Hospital Amedisys Home Health has partnered with hospitals through its Care Transitions program, designed to reduce unnecessary hospital readmissions through patient and caregiver health coaching and care coordination, which starts in the hospital and continues throughout completion of the patient's home health plan of care. Partnering with home healthcare 73% 60% of senior hospital leaders have adopted this strategy to lower preventable readmissions of hospitals have already selected home health care partners Source: “Readmission Reduction Strategies for Hospitals & Health Systems” and two surveys conducted by the Health Leaders Intelligence Unit © Aging Services of Minnesota 2014 25 Trend #5: Alliances Between Hospitals and PAC Allina Health and Minnesota Care Centers In February 2013, Allina announced it would enter into joint ventures with 5 care centers in the Minneapolis-St. Paul area to create transitional care units of the future Focus is specifically on short-stay, post-hospital care Transitional care units range from 40 to 60 beds and involve construction of new facilities as well as adaptation of existing hospital spaces The intention of these care center alliances is to create a clinically advanced care setting Participating care centers will benefit from increased clinical integration, skill development, and preferred provider status © Aging Services of Minnesota 2014 26 Trend #5: Alliances Between Hospitals and PAC Kindred HealthCare and Cleveland Clinic “Kindred seeks to shake up the post-acute care continuum” - Modern Health Care Kindred HealthCare and Cleveland Clinic have been awarded participation in the Bundled Payment for Care Improvement initiative (BPCI) Participation in this initiative is just one of several means in which Kindred is “shaking up the post acute care continuum” • It already has partnered with Cleveland Clinic to serve the system’s post-acute care patients in Cleveland Kindred is the nation’s largest provider of post-acute care Current: Future: 12 established integrated-care markets © Aging Services of Minnesota 2014 expanding to 25 markets 27 Notes © Aging Services of Minnesota 2014 28