Meeting Basic Survival Needs of the World's Least Healthy People

Global Health Law
Meeting Basic Survival Needs of the World's
Least Healthy People: Toward a Framework
Convention on Global Health
Lawrence O. Gostin
Linda and Timothy O’Neill Professor of Global Health Law
Georgetown University Law Center
The Challenge of Protecting Global Health
Health problems have serious economic, political, and security ramifications for millions
Major health hazards cross State borders
Protection of global health requires cooperation & global governance
Future Expectations: If No Changes Take Place
Most affected States:
Least capable of effecting change
States with resources to protect global health:
Lack political will to act outside their borders
Act out of narrow self interest or humanitarian instinct
Ethical/Legal obligation is not acknowledged
Assistance driven by public sympathy in catastrophic events, not long term health problems.
Result:
Spiraling deterioration of health in poorest regions with global consequences for disease transmission, trade, international relations, and security.
Meeting Basic Survival Needs
A focus on these major determinants of health would enable the international community to have a dramatic effect on global health prospects.
Sanitation
& Sewage
Essential
Medicines &
Vaccines
Pest
Control
Clean Air
& Water
Well
Functioning
Health System
Less dramatic and glamorous than emergency response measures, this approach would have lasting effects on common health problems.
Tobacco
Reduction
Diet
& Nutrition
Role of International Law I
Shortcomings of Current Legal Solutions:
Diverse state & non-state actors influencing health outcomes.
Difficulty in setting normative standards and assuring followthrough – especially in health.
International law is ineffective at creating obligations or even incentives for better funding, services, or protection in health of poor populations.
Role of International Law II:
FCGH as a Starting Point
The arena of global health law is in need of an innovative mechanism to structure international obligations.
Framework Convention on Global Health (FCGH):
Commit States to economic and logistic targets
Remove barriers to engagement of private and charitable sectors
Set realistic goals for global health spending as % GNP
Specify optimal areas of investment for basic survival needs
Build sustainable health systems
Create incentives for scientific innovation
WHO or new institution created for this purpose would set standards, monitor progress, mediate disputes.
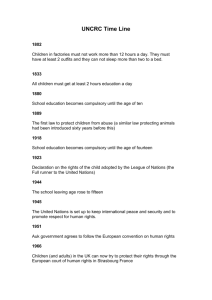
Detailed Lecture Outline
I.
Why should governments care about serious health threats outside their borders?
II.
Global equity and disproportionate burden of disease.
III. The international community’s choice to target a few high profile issues instead of deeper systemic problems in global health: what is the significance of basic survival needs?
IV. The value of international law and the proposal for a
Framework Convention on Global Health.
I. Global Health: A Matter of National Interest?
Human activities promote the spread of disease across national borders:
Environment
Pollution
Proximity to Animals
CYCLE OF
Congregation,
Consumption, and Movement
Overtaxed
Health
Systems
Members of the world community must rely on one another for health security:
State Instability
Bioterrorism
Poor Health
I. Global Health: A Matter of National Interest?
a. National Interests in the Health of the Populace
Primary obligations of a State:
– Defense
– Security
– Welfare includes Domestic Health affects
Health of Other Populations Beyond National Borders:
– DNA fingerprinting confirms pathogen migration
– More than 30 infectious diseases emerged in past 2-
3 decades. (Haemorrhagic fevers, Leginnaire’s disease, Hantavirus, West Nile virus, monkeypox, etc.)
– Vast growth in global trade of fruits, vegetables, meats, and eggs brings forth outbreaks of foodborne infections (Salmonella, E. coli, Norwalk).
More reasons to pay attention:
•Emerging and reemerging diseases increasingly affect developed nations, with resistance to front line drugs.
•Domestic costs of response can disrupt social life and infringe on individual rights.
I. Global Health: A Matter of National Interest?
b. National Economic Interests: Trade and Commerce
Disease
SARS in 2003
Effect on Trade and Commerce
Travel bans
FMD, BSE, and Avian influenza
Mass culling of flocks and herds, trade bans on beef, lamb, poultry.
Pandemic human influenza?
Projected loss of global GDP ≤ 6%)
HIV/AIDS Massive loss of life expectancy, with negative impact on entrepreneurs, skilled workforce, parents, and political leaders. Estimated GDP loss in hardest hit countries is almost 20% (World Bank).
Countries with extremely poor health become unreliable trading partners that struggle to:
•Develop and export products and natural resources
•Pay for essential vaccines and medicines
•Repay Debt
I. Global Health: A Matter of National Interest?
c. National Security
■ CIA: Infant mortality is a leading predictor of State failure.
■ U.S. Dept of State: AIDS is a national security threat.
Human
Rights
Abuses
Political
Instability
More likely to join in armed struggles
Sub-Saharan Africa:
•Overwhelming poverty and disease are paired with numerous political and military entanglements.
•The region’s marginal strategic importance has allowed the world to ignore the health and security crises.
States in
Poor
Health
Mass
Migrations
Civil
Unrest
More likely to harbor terrorisms
Eurasia:
•Burgeoning HIV/AIDS crises in India,
Russia, and China mirror that of sub-Saharan Africa.
•Additional emerging health problems (infant mortality, women’s health) exacerbate the HIV/AIDS crisis.
•Eurasia’s population, economic participation, and military prowess make it strategically important; regional instability will have dire ramifications for the world.
I. Global Health: A Matter of National Interest?
d. How States Perceive Global Health
-Although States may understand the threat of health hazards beyond their borders, actual engagement is limited-
•OECD countries: increased development assistance for global health from nearly $2 billion to $12 billion (1994-
2004).
•Gates Foundation will donate up to $3 billion per year for global health development.
BUT
•Global health development assistance is dwarfed by annual military spending ($1 trillion) and agricultural subsidies ($300 billion).
•Increase in assistance is a response to a few high-profile problems (HIV/AIDS, Pandemic flu,
Asian tsunami) – not a strategic long term commitment.
•Even with new investments most OECD states have not fulfilled their pledges (0.7% of GNP) and would need $100 billion to close the gap.
•National security assessments and international agreements only narrowly justify state action on global health.
Could states be correct that true global engagement does not serve their interests?..
II. Global Health Disparities: Are Profound Health Inequalities Fair?
•Poor populations’ burden of disease is not only higher than that of wealthier states, but also disproportionate.
•The degree to which the poor suffer unnecessarily is rarely considered.
•Disparities in life expectancy and likelihood of maternal death during labor are vast:
Average life exp in Africa is 30 years less than that in Americas or Europe.
A child from Zimbabwe or Swaziland is expected to live less than half as long as a child in Japan.
A child born in Angola is 73 times more likely to die than a child born in
Norway.
As life expectancy steadily climbs in developed states, less developed and transitional countries (Russia) are witnessing a drop in LE.
In one year, 14 million of the poorest people in the world died. If their life expectancy matched that of the world’s rich, that number would have dropped to 4 million .
II. Global Health Disparities: Are Profound Health Inequalities Fair?
a. Diseases of Poverty: Preventable Suffering
“Diseases of Poverty” – endemic in the world’s poorest regions but unknown among the world’s wealthy: filarial worms, elephantiasis, guinea worms, malaria, river blindness, schistosomiasis, and trachoma.
Guinea Worms: In 2003 the three most endemic countries, i.e., Sudan,
Ghana, and Nigeria reported 20,299 cases of the disease. (CDC)
Lelmi Malik, a 32-year-old mother of three, writhes in pain as Solomon
Olukade massages a guinea worm from her ankle in the village of
Dunkure, Nigeria. (March 22, 2001)
Credit: Mike Urban/Seattle Post-
Intelligencer
Filarial Worms: the secondleading cause of permanent and long-term disability in the world.
Filariasis causes disfiguring enlargement (elephantiasis) of the arms, legs, breasts, genitals.
Below: Antoinette St. Fab, left and her mother, Marie Denise
Bernard, in Léogane, Haiti.
Their Swollen legs are a symptom of lymphatic filariasis
Image Credit: NY Times
River Blindness/
Onchocerciasis: The disease is most intensely transmitted in remote African rural agricultural villages, located near rapidly flowing streams. Presently, it is estimated that 37 million people carry O. volvulus , with 90 million at risk in Africa. - African
Programme for Onchocerciasis
Control [APOC] (2005)
Image Credit: BBC International
II. Global Health Disparities: Are Profound Health Inequalities Fair?
b. Who is Responsible for Addressing Global Health Disparities?
Causal Pathways to Disadvantage Include:
•Poverty
•Poor Education
•Unhygienic Environments
•Pollution
•Social Disintegration
Systemic Disadvantages in health and other aspects of social, economic, and political life :
Almost everyone believes this is unfair, but there is no consensus on the ethical or legal obligation to help
Existing Inequalities
Beget Other Inequalities.
:
Fundamental Questions:
•WHY are inequalities unfair?
•WHO is responsible for change?
•What LEVEL of assistance is ethically justified?
II. Global Health Disparities: Are Profound Health
Are Disparities Ethically Wrong?
Argument:
Disparities are Ethically Wrong Because…
Problem:
Inequalities are self evidently wrong and unfair.
Needs elaboration.
Inequalities violate human rights.
Inequalities specifically violate the right to health.
“Rights discourse” is more rhetorical than truly explanatory.
“Right to Health” focuses on State obligations to their own populations.
Alternative: Theory of human functioning
Health is an asset essential for adequate functioning of individuals and communities.
Population health is a transcendent value because it enables a series of activities critical to public welfare.
II. Global Health Disparities: Are Profound Health Inequalities Fair?
b. Who is Responsible for Addressing Global Health Disparities?
Is There a Duty to Rectify Disparities?
•Existing claims (Nagel, Rawls, Walzer) are narrowly framed around the state:citizen relationship.
•Positing such a relationship between countries is a challenge.
•Arguments for a non-statist view of the global community that focuses on interdependence are rare outside activist circles.
What
Creates
Such Duty?
DUTY TO
RESPOND
Whose
Duty
Is It?
What is the
Scope of
Such Duty?
Lack of a principled ethical argument may show the need for international law.
III. Basic Survival Needs: Ameliorating Suffering and Early Death
Most international aid is ineffective and even counterproductive:
•The current level of support will surely wane.
•After the interest and/or resources have run out, the world’s poor will be in the same or worse position as before.
Solution:
Mobilization of public and private sectors to meet basic survival needs. (e.g. Marshall Plan)
Marshall Plan poster, circa 1949
III. Basic Survival Needs: Ameliorating Suffering and Early Death a. Reframing the Approach to Development Assistance
•Emphasis on high-visibility crises diverts resources from long-term projects that focus on everyday needs.
•A small number of wealthy donors are setting the global development agenda – with little understanding of local needs and capacities. (see right)
•Assistance is fragmented and uncoordinated: programs compete with each other and with local efforts.
•Many projects have narrow, short-term goals preferring quick, observable, and quantifiable results.
•Massive infusion of assistance can produce problematic over-reliance and dependency.
•Host countries also carry some responsibility for the failures of international assistance: preference for other needs over health, corrupt misappropriation of funds, incompetence, and bureaucracy.
III. Basic Survival Needs: Ameliorating Suffering and Early Death b. Basic Survival Needs as a Measure of Int’l Health Assistance
Immunizations
Assistance should be redirected to support
Basic Survival Needs.
Health
Education
Essential
Medicines
Primary
Health Care
Nutritional
Foods
Potable
Water
Sanitation
Pest
Abatement
Public
Health
Infrastruct.
Something as simple as a vaccine, generic drug, basic engineering, or sanitation can result in significant health improvements among the world’s poorest populations.
Nigerian woman receives a smallpox vaccination in 1969 during the World Health
Organization's effort to wipe out smallpox. By 1979 the virus had been eradicated.
III. Basic Survival Needs: Ameliorating Suffering and Early Death b. Health Systems: Basic Infrastructure & Capacity Building
Foreign run state-of-the-art facilities
Capacity-building assistance
Poor countries in need of adequate health care
Health System Needs:
Public health agencies
Primary health care services
Human resources – skilled workers
(HCW)
Public health education facilities (to minimize brain drain).
Foreign aid workers
Area of Concern:
Even when developing countries train HCWs, they are pushed to migrate by depressed working conditions at home and pulled by aggressive recruiting from OECD states.
IV. Global Governance for Health: Proposing a Framework Convention
Investing in Infrastructure…
• The amount of money is not more important than the strategy of investment and utilization of newly available resources.
• A structured approach would:
1. Set goals
2. Ensure coordination
3. Monitor results
Existing tools are inadequate – a NEW approach is needed.
IV. Global Governance for Health: Proposing a Framework Convention a. International Health Law: WHO’s Record
WHO’s Normative Powers:
• Can adopt binding conventions that are stronger than normal treaties.
• Has quasi-legislative powers to adopt binding regulations. (opt-out system).
WHO’s Thin Record (in 60 years):
• Modern international health law has only 1 significant regulation and 1 treaty
• The IHRs (revised in 2005 and addressing the same diseases as a
1851 conference) address the trans-migration of disease and not the health of poorest populations.
• FCTC (2003) regulates the only lawful product that is uniformly harmful and was only feasible because of industry villification.
IV. Global Governance for Health: Proposing a Framework Convention b. Influence of Trade and the Human Right to Health
• Other agencies have developed international law that affects health...
• WHO’s lack of participation can be blamed on their image as a narrowly scientific/technical agency, yet is still has the responsibility to contribute its expertise.
• WHO’s definition of a right to health is so broad as to be unattainable.
• Recasting the problem of poor health as a human rights violation is unhelpful:
1. Legal obligation falls on the state to protect its own population – other populations cannot take precedence.
2.
Since the right to health is “progressively realizable”, potential violations require subjective judgment.
3. Even if some obligation can be read, there is no systematic method of implementation and enforcement.
IV. Global Governance for Health: Proposing a Framework Convention c. Framework Convention: Details
The Framework Convention Format
Framework Convention on Global Health
Responds to
Incorporates a bottom-up strategy
Strives to build health system capacity
Sets priorities to meet basic survival needs
Engages stakeholders to contribute resources and expertise
Works to harmonizes activities among world actors
Evaluates and monitors progress towards set goals and priorities.
Structural inadequacies in international health law:
•Vague standards
•Ineffective monitoring
•Weak enforcement
•“Statist” approach
The Kyoto Protocol, UN Framework Convention on Climate Change, and Framework Convention on Tobacco Control illustrate the developing and essential role of the framework convention-protocol approach.
IV. Global Governance for Health: Proposing a Framework
Broad Principles of the Framework Convention
IV. Global Governance for Health: Proposing a Framework Convention c. Framework Convention: Details
Advantages of the Framework Convention
Incremental process and ability to evolve in the long term: helps avoid political bottlenecks.
Creation of international norms and institutions provides an ongoing and structured forum for States and stakeholders to interact.
A high profile forum can educate and influence actors to take decisive steps.
Existence of a “normative community” helps build international consensus.
Active engagement of stakeholders in negotiation, debate, information exchage, and capacity building.
Challenging barriers to FCGH remain:
Domination of economically and politically powerful countries.
Deep resistance to expend/transfer wealth.
Little confidence in international legal regimes
V. The Tipping Point
Many Reasons to Act:
•National interest
•Ethical obligation
•Legal obligation
Although no one reason may be definitive, the cumulative weight of such evidence leaves no room for the status quo.
The complex and enduring problems in global health require a response that is:
COLLECTIVE – COOPERATIVE – INNOVATIVE -- COMMITTED
Consequences of Inaction: State political and economic decisions to withhold a fair share of assistance, major outbreaks of preventable infectious disease, and a dangerous shift of affluent actors to another cause.