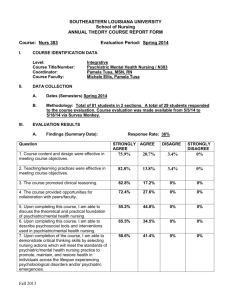
ISLAMIC UNIVERSITY OF GAZA FACULTY OF NURSING MASTER
advertisement

ISLAMIC UNIVERSITY OF GAZA
FACULTY OF NURSING
MASTER OF COMMUNITY MENTAL HEALTH NURSING
STANDARD OUTLINE FOR COURSE SYLLABUS
Course title: Contemporary mental health nursing
Course Instructor: Dr. Ashraf El-Jedi, RN, BSN, MSN,
DrPH.
Term: First semester 2009/2010
Course description
• This course allows students to study current issues
impacting upon the development and application of
mental health nursing principles. It focuses on two
central themes: 1) evidence-based nursing practice
and 2) global mental health. It provides students with
the most current, culturally competent, authoritative,
and comprehensive resource available.
Learning objectives
At the end of this course the participant will be able to:
• Identify different global issues in mental health nursing.
• Be Familiar with trends in provision of care in mental health
settings.
• Recognize the most recent Issues relating to policy, planning,
and clinical nursing practice.
• Consider ethical issues when practicing mental health nursing.
• Be Familiar with Human rights regarding mental
health/illness.
• Identify the most current, culturally competent, authoritative,
and comprehensive international and local resource available.
• Demonstrate understanding to the most up-to-date, evidencebased, culturally competent, practice.
Course content schedule:
Teaching Methods:
•
•
•
•
•
Lectures
Discussion
Demonstration
Audiovisual aids
Work group
Evaluation
•
•
•
•
Mid term exam
Assignment and project
Final exam
Total
30%
20%
50%
100%
Course Policies:1- Students are expected to prepare for lectures
by reading the assigned material and reviewing
relevant literature.
2- Attendance of lecture is a requirement. (See
the university policies regarding absence)
3- Students are expected to attend the exams.
Any missed exam will result in a grade of zero
(0) for that exam.
References
• Gail Wiscarz Stuart (2009). Principles and
Practice of Psychiatric Nursing. 9th Edition
• Stickley T & Basset T (2008). Learning about
mental health practice. Jone Wiley & Sons
Inc. England
Principles of Psychiatric
Nursing Care
• You are about to begin a voyage to places
you have never been before: the world of
psychiatric and mental health nursing,
students learned about pieces of peopleand infected toe, a congested lung, a
troubling twitch, or maybe even a broken
heart-but pieces nonetheless.
• Today, students learn about the wholeness
of people: a physically ill child struggling
to find safety in an abusive family, an
adolescent coping with eating problems
and self-esteem, a young adult grieving
over the diagnosis of HIV/AIDS, or an
elder, living alone, feeling confused and
going to a nursing home.
• This is the exciting world of today's
psychiatric nurse. It integrates the
biological, psychological, sociocultural,
environmental, legal, and ethical realities
of life and weaves them together in a
rich tapestry called Psychiatric-mental
health nursing practice.
Role Emergence
• The role of psychiatric nursing began to emerge in the
early 1950s.
• An article by Bennett and Eaton in the American
Journal of Psychiatry in 1951 identified the following
problems affecting psychiatric nurses:
• Scarcity of qualified psychiatric nurses.
• Underused of their abilities
• The fact that "very little real psychiatric nursing is
carried out in otherwise good psychiatric hospitals
and units".
Evolving Functions
In 1958 the following function of psychiatric nurses were
described (Hays, 1975):
• Dealing with patients' problems of attitude, mood, and
interpretation of reality.
• Exploring disturbing and conflicting thoughts and
feelings.
• Using the patient's positive feelings toward the therapist
to bring about psycho physiological homeostasis.
• Counseling patients in emergencies, including panic and
fear
• Strengthening the well part of patients.
The 1970s gave rise to the further development
of the specialty. Psychiatric nurses became the
pacesetters in specialty nursing practice. They
were the first to do the following:
• Develop standards and statements on scope of
practice.
• Establish generalist and specialist certification.
The 1980s were years of exciting scientific growth
in the area of psychobiology. New focus was
placed on the following:
•
•
•
•
•
Brain-imaging techniques
Neurotransmitters and neuronal receptors
Psychobiology of emotions
Understanding the brain
Molecular genetics related to psychobiology.
Psychiatric nurses thus entered the
1990s faced with the challenge of
integrating the expanding bases of
neuroscience into the caring and
holistic biopsychosocial practice of
psychiatric nursing.
• By 2000 psychiatric nurses agreed that
the knowledge base of the specialty is
based on the integration of the biological,
spiritual, social, and environmental
realms of the human experience
(Raingruber, 2003; Silverstein, 2006).
Contemporary Practice
• Psychiatric-mental health nursing is an
interpersonal process that promotes and
maintains patient behavior that contributes
to integrated functioning. The patient may
be an individual, family, group,
organization, or community.
• The American Nurses Association's PsychiatricMental Health Nursing Scope and Standards of
Practice (2007) defines psychiatric-mental health
nursing as "a specialized area of nursing practice
committed to promoting mental health through the
assessment, diagnoses, and treatment of human
responses to mental health problems and psychiatric
disorders…. {It} employs a purposeful use of self as
its art and a wide range of nursing psychosocial and
neurobiological theories and research evidence as its
science."
• The Center for Mental Health Services
officially recognizes psychiatric nursing as one
of the five core mental health disciplines.
• The other four disciplines are marriage and
family therapy, psychiatry, psychology, and
social work.
Nurse-Patient Partnership:
• The contemporary practice of psychiatric-mental
health nursing occurs within a social and
environmental context. Thus the "nurse-patient
relationship" has evolved into a "nurse-patient
partnership" that expands the dimensions of the
professional psychiatric nursing role. These elements
include clinical competence, consumer-family
advocacy, mutual responsibility, interprofessional
collaboration, social accountability, and legalethical parameters. (Figure).
Figurer: Elements of the Psychiatric-mental health
nursing role
.
Competent Caring:
• The three domains of contemporary
psychiatric-mental health nursing practice are
direct care, communication, and
management. Within these overlapping
domains of practice, the teaching,
coordinating, delegating, and collaborating
functions of the nursing role are expressed
(Figure ).
Figurer: Psychiatric-mental health nursing practice.
Psychiatric-mental health nurses are able to do
the following:
• Make culturally sensitive biopsychosocial health
assessments.
• Design and implement treatment plans for
patients and families with complex health
problems and co morbid conditions.
• Engage in care management activities, such as
organizing, assessing, negotiating, coordinating,
and integrating services and benefits for
individual and families.
• Provide a " health care map" for individuals, families,
and groups to guide them to community resources for
mental health, including the most appropriate
providers, agencies, technologies, and social systems.
• Promote and maintain mental health and manage the
effects of mental illness through reaching and
counseling.
• Provide care for physically ill people with
psychological problems and psychiatrically ill people
with physical problems.
• Manage and coordinate systems of care integration
the needs of patients, families, staff , and regulators
Domains of Psychiatric-Mental
Health Nursing Practice
Levels of performance
• Four major factors _ laws, qualifications, practice
setting, and personal initiative _ play a part in
determining the roles engaged in by each nurse.
Laws
• Nurse practice acts also address aspects of advanced
practice, including prescriptive authority (Staten et al,
2006). Nurses must be familiar with the nursing
practice act of their state and define and limit their
practice accordingly.
Qualifications
• Psychiatric_ mental health registered nurse
(RN- PMH).
• Psychiatric _ mental health advanced practice
Registered nurse (APRN – PMH): An
advanced practice nurse may be either a
clinical nurse specialist (CNS) or a nurse
practitioner (NP).
Practice setting
• Settings for psychiatric- mental health nurses include
psychiatric facilities, community mental health centers,
psychiatric units in general hospital, residential facilities, and
private practice. Many psychiatric hospitals have become
integrated clinical systems that provide inpatient care, partial
hospitalization or day treatment, residential care, home care,
and outpatient or ambulatory care.
• Community – based treatment setting have expanded to
include primary care clinics, schools, prisons, industrial
settings, managed care facilities, health maintenance
organizations, hospices visiting nurse associations, home
health agencies, emergency departments nursing homes, and
shelters.
• Psychiatric- mental health nurses are quickly
moving into the domain of primary care and
working with other nurses and physic- cians to
diagnose and treat psychiatric problems in
patients with comorbid medical conditions.
• Treatment in a nonpsychiatric environment
may be more efficient and more acceptable to
patients and their families.
Personal initiative
• This is a very important factor
Psychiatric nursing agenda
• Psychiatric- mental health nursing continues to
grow and evolve.
• More than 80,000 registered nurses are
working in mental health organizations in the
United States: half are employed in psychiatric
hospitals and the other half are community
based.
• There are more than 20,000 advanced practice
psychiatric- mental health nurses with graduate
degrees.
• To best meet the challenges of the next decade,
psychiatric nurses need to focus their energies
on three areas: outcome evaluation, leadership
skills, and political action.
Outcome evaluation
• Psychiatric-mental health nurses must identify,
describe, measure, and explain the process and
outcomes of the care they provide to patients,
families, and communities.
• "What difference does psychiatric nurse caring
make?
Leadership skills
• Psychiatric-mental health nurses need knowledge and
strategies that enable them to exercise leadership and
management in their work. Such leadership has a direct
impact on the care patients receive. It also strengthens
and expands the contribution of psychiatric nursing to
the larger health care system Psychiatric-mental health
nurses need knowledge and strategies that enable them
to exercise leadership and management in their work.
Such leadership has a direct impact on the care patients
receive. It also strengthens and expands the
contribution of psychiatric nursing to the larger health
care system
Political Action
• Increasing psychiatric nurses' political
awareness and skills is necessary to bring
about needed changes in the mental
health care delivery system.