Routes of Bacterial Infection
advertisement
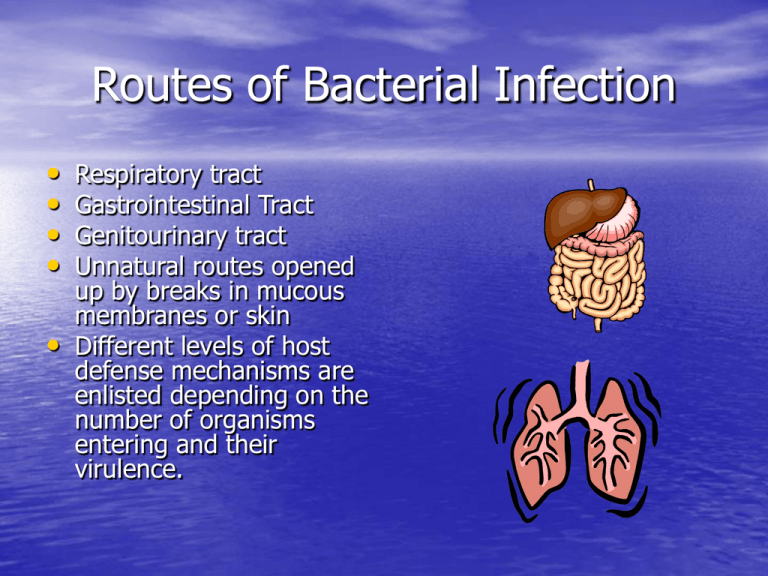
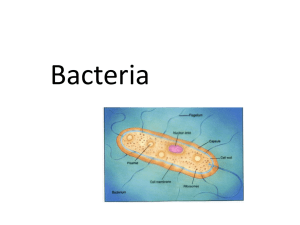
Routes of Bacterial Infection • • • • Respiratory tract Gastrointestinal Tract Genitourinary tract Unnatural routes opened up by breaks in mucous membranes or skin • Different levels of host defense mechanisms are enlisted depending on the number of organisms entering and their virulence. Immune Response to Bacteria • Extracellular Bacteria – Humoral immune response – Humoral antibodies produced by plasma cells in regional lymph nodes and submucosa of respiratory and gastrointestinal tracts – The antibodies remove the bacteria and inactivate bacterial toxins to protect the host cell from invading organisms. • Antibody neutralizes • • • • bacterial toxins Complement activation Antibody and complement split product C3b bind to bacteria, serving as opsonins to increase phagocytosis. C3a and C5a induce local mast cell degranulation Other complement split products are chemotactic for neutrophils and macrophages. Immune Response to Bacteria • Intracellular Bacteria – Cell-mediated immune response (Delayedtype hypersensitivity) – Activate Natural Killer (NK) cells provide early defense against bacteria. • In delayed type hypersensitivity, cytokines secreted by CD4+ T cells, such as IFN gamma, activate macrophages to kill ingested pathogens more effectively. Bacterial Evasion of Host Defense Mechanism • Four Steps in Bacterial Infection – Attachment to host cells – Proliferation – Invasion of host tissue – Toxin-induced damage to host cell Many bacteria have developed ways to overcome some of these host defense mechanisms Contribution of the Immune Response to Bacterial Pathogenesis • Disease can also be caused by the immune response to the pathogen. • Pathogen-stimulated overproduction of cytokines can lead to symptoms of bacterial septic shock, food poisoning, and toxic shock syndrome. Contribution of the Immune Response to Bacterial Pathogenesis • Bacteria that can survive intracellularly within • infected cells can result in chronic antigenic activation of CD4+ T-cells, leading to tissue destruction by a cell-mediated response with characteristics of a delayed type hypersensitivity reaction Cytokines secreted by CD4+ cells can accumulate, leading to the formation of granulomas. The concentrations of lysosomal enzymes in the granulomas can cause tissue necrosis. Diphtheria (Corynebacterium diphtheriae) • Gram positive, rod-like • • • • organism Bacterial disease caused by a secreted exotoxin. Spread via airborne respiratory droplets Exotoxin destroys underlying tissue, forming a tough, fibrous membrane compose of fibrin, white blood cells and dead respiratory cells Also responsible for systemic manifestations. Symptoms of Diphtheria • Damage to different organs such as the heart, liver, kidneys and nervous system. • Choking layer of bacteria and dead cells in the respiratory system, accompanied by an unworldly stench • Difficulty swallowing and breathing • Pus and blood discharge through nostrils following death from asphyxiation More info on diphtheria…… • The exotoxin is encoded by the tox gene carried by • • • • phage B (beta) Some strains can exist in the state of lysogeny. Exotoxin has two disulfide linked chains, a binding chain and a toxin chain. The binding chain interacts with ganglioside receptors on susceptible cells, facilitating internalization of the exotoxin. Inhibitory effect of toxin chain on protein synthesis leads to toxicity. Removal of the binding chain prevents exotoxin from entering the cell. How We Treat This Bad Boy…. • Toxoid prepared by treating diphtheria toxin with • • • formaldehyde. Reaction with formaldehyde cross-links the toxin, resulting in loss of toxicity and enhancement in its antigenicity. Usually administered with tetanus toxoid and inactivated Bordetelal pertussis in a combined vaccine that is given to children 6-8 weeks of age. Immunization with toxoid induces production of antibodies which bind to the toxin and neutralize its activity. The reaction that results from the vaccine Photo Ops of Diphtheria (Smile!) Tuberculosis (Mycobacterium tuberculosis) • Bacilli shaped organism • Pulmonary infection by inhalation • • • • of small droplets of respiratory secretions containing a few bacilli Inhaled bacilli are ingested by alveolar macrophages and multiply intracellulary by inhibiting formation of phagolysomes. Macrophages lyse and large numbers of bacilli are released. Cell mediated response by CD4+ T cells may be responsible for much of the tissue damage of the disease. Most common infection of tuberculosis is pulmonary tuberculosis. Symptoms of Tuberculosis • Symptoms of TB depend on where • in the body the TB bacteria are growing. TB bacteria usually grow in the lungs. TB in the lungs may cause – a bad cough that lasts longer than 2 weeks – pain in the chest – coughing up blood or sputum (phlegm from deep inside the lungs) Other symptoms of TB disease are – weakness or fatigue – weight loss – no appetite – chills – fever – sweating at night Immune Response to Tuberculosis • Cytokines produced by CD4+ T cells activate • • • macrophages, which kill the bacilli or inhibits their growth. High levels of interleukin-2 (IL-2), produced by macrophages, stimulates Th 1-mediated responses. IL-2 may also contribute to resistance by inducing production of chemokines that attract macrophages to the site of infection. CD4+ T cell mediated response mounted by those exposed to M. tuberculosis controls the infection and protects against later infection. Treatment and Vaccines • Tuberculosis is treated with several drugs including isoniazid, rifampin, streptomycin, pyrazinamide, and ethambutol. • Drug therapy must continue for at least 9 months to get rid of the bacteria since the intracellular growth of M. tuberculosis makes it difficult for the drugs to reach the bacilli. • Vaccine : attenuated strain of M. bovis called BCG (Bacillus Calmette-Guerin) Most effective against extrapulmonary tuberculosis. Not used in the U.S. though. Sorry! Tuberculosis Links! Yay! • http://www.phppo.cdc.gov/PHTN/tbmodul es/modules1-5/m1/anim.htm • http://www.phppo.cdc.gov/PHTN/tbmodul es/modules1-5/m3/photos/3photo3.9.htm • http://www.phppo.cdc.gov/PHTN/tbmodul es/modules1-5/m3/photos/3photo3.8.htm • http://www.cdc.gov/ncidod/diseases/subm enus/sub_tuberculosis.htm Lyme Disease (Borrelia burgdoferi) • Helical shaped bacteria • Disease spread by bite • • from an infected deer tick Enters the bloodstream and spreads to different organs in the body Arthritic symptoms and neurologic symptoms can develop. Most people complain of headaches and some people develop meningitis or encephalitis. Immune Response • Antibodies to a protein associated with the flagella of B. burgdorferi is usually detected after infection and may contribute to pathogenesis. • Antigen-antibody complexes can activate complement system, resulting in direct lytic damage to the joints or vasculature. • Interleukin 1 (IL-1) said to be involved in pathogenesis of Lyme disease, since Borrelia has a cell wall containing lipopolysaccharide (LPS) and LPS is a well known inducer of IL-1 • Most humans develop antibodies to a flagellar antigen, while mice develop antibodies to two proteins on the outer surface of the bacterial envelope. How do we treat it? • Lyme disease can be • successfully treated with broad-spectrum antibiotics such as penicillin and tetracycline. A vaccine based on outersurface protein A suggests that it offers significant protection. The vaccine was approved for use in January 1999. Online Information on Lyme Disease • http://www.cdc.gov/ncidod/dvbid/lyme/in dex.htm – This is just some general info on Lyme Disease • http://phil.cdc.gov/Phil/detail.asp?id=2417 – This is a up close and personal picture of Borrelia burgdorferi