The Blood
advertisement

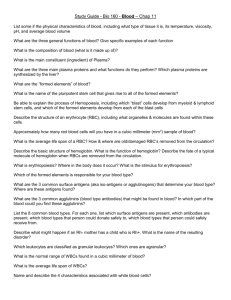
The Blood The Blood Definition Blood is a connective tissue, not a body fluid, made of fluid (plasma) and cellular elements (RBC, WBC, and platelets) Its volume is 5-6 L in males and 4-5 L in females It is slightly alkaline, with a pH of ~ 7.4 Its color varies from bright to dark red It has a salty metallic taste The Blood Functions The blood is vehicular organ that reaches all the other tissues Transports oxygen and nutrients Removes CO2 and other by-products of cell activity Pivotal in maintaining homeostasis, growth and tissue repair Participates in the defense against infection Participates in hemostasis Participates in body heat distribution and regulation Marieb and Hoehn Human Anatomy & Physiology seventh edition Pearson Benjamin Cummings The Blood Plasma Straw colored fluid made of water (~90%), other contents include: Proteins make the bulk of the solutes: Albumens (60%), manufactured in the liver are the most abundant Globulins (36%) are immune bodies Fibrinogen (4%) for blood clotting Nutrients: glucose, amino acids, lipids, cholesterol Electrolytes: Na+, K+, Ca++, Mg++, H+, Cl-, HCO3-, PO4--, SO4-Waste: urea, creatinine, uric acid, bilirubin Gases: O2 , CO2 , N2 Protein bound hormones Plasma without clotting factors is called “serum” Peripheral blood smear Marieb and Hoehn Human Anatomy & Physiology seventh edition Pearson Benjamin Cummings Electron micrograph of blood smear Pathophysiology McCance & Huether fifth edition Elsevier Mosby The Blood RBC An RBC is a 7.5 micron disc shaped body with a central depression The cell is without a nucleus or mitochondria AN RBC contains hemoglobin and filamentous proteins attached to the cell wall to impart flexibility on it Antigens are embedded in the cell membrane, they decide the blood group The RBC cytoplasm provides energy to maintain intracellular homostasis This energy is generated mostly through anaerobic glycolysis RBCs function is gas exchange: O2 to the tissues and CO2 to the lungs The Blood RBC Structure of Hemoglobin Each hemoglobin molecule is made up of four globin chains and four heme molecules Heme molecule is a porphyrin type pigment with a ferrous ion (Fe++) Globin is a 287 amino acid protein made of two α, and two non α chains Adult hemoglobin A is (αα/ββ), fetal hemoglobin F is ( αα/γγ) An enzyme, 2,3 diphosphoglycerate (2,3 DPG) binds to hemoglobin molecule, it lowers its affinity to O2 Binding of O2 to heme breaks some of the globin bonds exposing more heme molecules to bind with O2 Structure of hemoglobin Each heme molecule combines with one oxygen atom Marieb and Hoehn Human Anatomy & Physiology seventh edition Pearson Benjamin Cummings Structure of hemoglobin and the oxygen dissociation curve Davidson’s Principles and Practice of Medicine eighth edition, Churchill Livingstone The Blood RBC Development of RBCs Hypoxia → erythropoietin (kidney)→ red marrow of long bones→ erythroid stem cell→ erythroblasts cell division→ smaller cells loosing nucleus and gaining hemoglobin → reticulocyte→ mature RBC Reticulocytes contain remnants of cell organelles Their presence in excess in the peripheral blood (>2%) indicates excessive RBC destruction The normal number of RBCs is 4.3-5 million/mm3 in the female and 5.1-5.8 million/mm3 in the male The normal values for Hgb are 13-15 gm/dl for females and 14-16 gm/dl in males Amino acids, lipids, carbohdrates, iron, vitamin B12 and folic acid are essntial for hemoglobin synthesis The Blood RBC Hemoglobin has a remarkable ability to bind with oxygen forming oxyhemoglobin It can also release the oxygen to the tissues becoming deoxyhemoglobin Hemoglobin combines with CO2 forming carbaminohemoglobin The Blood RBC Destruction Life span ~ 120 days RBCs are phagocytosed by the reticulo-endothlial cells of the spleen Globulin is hydrolyzed to amino acids that are recycled Iron is removed from heme and reused to synthesize Hgb Heme remnant converted to bilirubin Bilirubin is conjugated with glucoronic acid, and secreted in bile In the intestine most is converted to stercobilin and excreted A small amount of stercobilin is absorbed by the kidney and secreted as urobilinogen The Blood RBC Disorders of RBCs Anemia is reduced RBC count Anemias can be caused by RBC loss or reduced production Hemorrhage, hemolysis, depressed bone marrow Reduced hemoglobin content of RBCs Iron, intrinsic factor, folic acid, or B12 deficiency Congenital hemoglobin defects Thalassemia, sickle cell anemia, spherocytosis The Blood RBC Disorders of RBCs Plolycythemia Bone marrow disorder causing an increased number of circulating RBCs and increased blood viscosity Aplastic anemia Results from bone marrow suppression or destruction (radiation, drugs, chemicals) All the blood elements are deficient Normal and sickle cell RBC In sickle cell disease hemoglobin S replaces the β chain In thalassemias, the α or β chains can be absent or defective Marieb and Hoehn Human Anatomy & Physiology seventh edition Pearson Benjamin Cummings The Blood White Blood Cells (WBC) Function Lymphocytes are the effectors of the immune function WBCs main function is to fight bacterial infections WBCs are the only nucleated blood formed elements They exercise their functions in the tissues not the blood stream Selectines induce the WBC to adhere to capillary endothelium WBC migrate to the tissue spaces by diapeditic movement between endothelial cell, diapedesis is initiated by chemical attraction to the infection site initiated by damaged cells “chemotaxis” WBC destroy the bacterial cell wall by oxidation and digestion by proteins “defensisns” The Blood White Blood Cells (WBC) Types The total number of WBCs is 4000 to 10,000/mm3 There two main types of WBCs: granulucytes and agranulocytes Granulocytes, are of three types Neutrophils (polymorphs) 50-70%, oxidize bacteria Eosinophils, 2-4% bilobed nuclei, attack parasites Basophils, 1% in peripheral blood, reside in the tissues, contain histamine, involved in hypersensitivity reaction The Blood White Blood Cells (WBC) Types Agranulocytes are of two types Lymphocytes, the smallest and second most abundant T cells (80%) mediate cellular immunity, express CD1,2,3,4,5,7 & 8 B cells mediate humoral immunity, express immunoglobulin light chains on the surface Monocytes, the largest, migrate to the tissues and become macrophages involved in cellular immunity, secrete IL1 , TNF, and CSF White blood cells, the granulcytes Davidson’s The Priciples and Practice of Medicine, eigthteenth edition Churchill Livingstone Monocytes and lymphocytes Davidson’s The Priciples and Practice of Medicine, eighteenth edition Churchill Livingstone The Blood WBC Development WBC production is Stimulated by two types of messengers Inerleukins: IL-3 stimulates basophils (also RBCs and platelets) IL-5 stimulates eosinophils IL-3, IL-4 and IL-7 stimulate B lymphocytes IL-2, IL-4 and IL-7 stimulate T lymphocytes Colony stimulating factors (CSF) G-CSF stimulate neutrophils (granulocytes) GM-CSF stimulate eosinophils and monocytes WBC life span is 1 to 9 days Development of blood cells Vander’s Physiology eighth edition, Mc Graw Hill The Blood WBC Leukemias A single unspecialised WBC precursor cell “clones” itself uncontrollably The resulting “leukemia” is therefore “monclonal” The more undifferentiated cells produce acute (blastic) leukemias The more differentiated (cytic) cells produce chronic types A leukemia is called according to the producing cell Leukemias impair the bone marrow, and other blood cells functions Death is inevitable unless treated, it results from bleeding or sepsis The Blood Blood Coagulation Coagulation is a natural mechanism that acts to diminish blood loss from hemorrhage Coagulation (thrombosis) especially in the microcirculation is also a manifestation of inflammation and sepsis Coagulation occurs in three Stages Platelet plug The cascade leading to fibrin (clot) formation Clot retraction and repair (PDGF) The Blood Blood Coagulation The Platelets Structure and Function Platelets are discoid shaped bodies of 2-4 μm Derived from megacaryocytes arising from lineage committed stem cells They are fragments of cells, they have no nuclei They contain three types of granules in the cytoplasm Alpha granules contain fibrinogen and von Willebrand factor (vWF) Delta (dense) granules store adenosine diphosphate and serotonin Lysosomes, contain acid hydrolases The Blood Blood Coagulation The Platelets Platelets are activated by thrombin, collagen, or ADP, they discharge their content which leads to the formation of thrombaxane A2 Platelets adhere to exposed collagen in the presence of von Willebrand factor (vWF) Their life span is 8-14 days, they are destroyed in the cells of the RE system The structure of a platelet Davidson’s The Priciples and Practice of Medicine, eighteenth edition Churchill Livingstone Initial vasoconstriction and platelet plug Vander’s Physiology eighth edition Mc Graw Hill v Intrinsic and extrinsic coagulation pathways Calcium ions are essential for the coagulation cascade Vander’s Physiology eighth edition Mc Graw Hill The role of the liver in blood coagulation Vander’s Physiology eighth edition Mc graw Hill EM of a blood clot: RBC’s and fibrin NIBSC?Science Photo Libraray – Taken from Vander Physiology eighth edition Mc Graw Hill Prostacyclin (PGI2 ) and nitric oxide inhibit platelet aggregation Vander’s Physiology eighth edition Mc graw Hill The Blood Anticoagulation Natural Anticoagulants Tissue factor pathway inhibitor (TFPI) Plasminogen - plasmin Heparin Antithrombin III Protein C Protein S Vitamin E quinone Natural anticoagulants also have anti inflammatory activity The Blood Anticoagulation Massive blood flow The (Intact) Endothelium Prevents platelet contact with collagen Displays heparin on its surface Secretes prostacyclin (PGAI2) and nitric oxide Activates protein C via attached thrombomodulin-thrombin complex Secretes tissue plasminogen activator The Blood Anticoagulation Heparin Is a natural anticoagulant found in the body Can be given by IV or subcutaneous routes for anticoagulation Can be easily neutralized (its action reversed) by protamine It has an antithrombin effect Inhibits platelet functions Its effect is measured by estimating the partial prothrombin time (PTT) The Blood Antigoagulation Aspirin (ASA) Inhibits cyclooygenase (COX) that catalyzes the formation of thrombaxane Mature platelets can not make new thrombaxane because their COX is blocked Endothelial cells can synthesize new COX, therefore they are not affected by ASA Thrombaxane is important for platelet aggregation Platelet function is assessed by the bleeding time New drugs that interfere with fibrinogen/platelet binding are now available The Blood Anticoagulation Vitamin K antagonists Warfarin, also known as coumadin Interfere with the liver synthesis of coagulation factors Effect measure by checking the protime (PT) now reported as international normalized ratio (INR) Vitamin E quinone is a potent anticoagulant Inactivation of Factors VIII & V by thrombin activated protein C Vander’s Physiology eighth edition Mc Graw Hill Fibrinolysis, a mechanism for clot resorption Vander’s Physiology eighth edition Mc Graw Hill The Blood Thrombolytics Plasminogen activates plasmin, a natural fibrinolytic agent Tissue Plasminogen Activator (t-PTA) activates plasminogen Plasmin dissolves an already formed clot (thrombolytic therapy) Streptokinase and Urokinase Thrombolytic action Streptokinase has side effects but less costly Urokinase has less side effects but more expensive New drugs that interfere with fibrinogen/platelet binding are now available The Blood Transfusion The following blood elements can be transfused to cover a deficiency in quantity or quality of one or more of the blood components Whole blood does not allow time for checking for the presence of infectious agents Packed RBC’c for low Hb Platelets for thrompcytopenia and bleeding Plasma (fresh frozen) to replace deficient intrinsic factors Cryoprecipitate for hemophilia The Blood Transfusion Stored blood is acidified with citrates to prevent coagulation It looses its platelets Has more potassium, and accumulates ammonia More hemolysed RBC as the storage is prolonged Hemoglobin tends to hold more to O2 because of the reduction in 2,3 diphophoglyceric acid (2.3 DPG) The life span of RBCs stored at 4o C is about 28 days The Blood Blood Types RBC’s have surface antigens RBC’s can be grouped according to the presence or absence of certain antigens There are many RBC antigens but only a A, B, AB and the Rh are of clinical significance Each one of the four types can be Rh positive or negative Donor blood is mixed with recipient serum to decide compatibility, donor cell clumping indicate incompatibility Major blood groups A certain group posseses its antigen on the RBC surface and antibodies against the others Marieb and Hoehn Human Anatomy & Physiology seventh edition Pearson Benjamin Cummings The Blood Transfusion Transfusion of incompatible RBCs results in their hemolysis in the donor This leads to blockage of the renal tubules, hypotension, fever, back pain, and may prove fatal This is treated by stopping the transfusion, hydration, and alkalinization of the urine Not every reaction to transfusion is due to infused RBC hemolysis, other less severe reactions can occur Identification of the RBC group Marieb and Hoehn Human Anatomy & Physiology seventh edition Pearson Benjamin Cummings The Blood Rh Factor There are no preformed Rh antibodies in Rh- individuals They develop after exposure to Rh+ factors (antigens) This explains the fact that an Rh+ fetus of an Rh- mother does not usually suffer But the Rh- mother can be sensitized to the Rh+ antigens during the first pregnancy, especially during delivery Subsequent fetuses can suffer from the mother’s Rh antibodies passed to it and its blood hemolyzes This can be prevented by giving the mother serum that blocks the Rh+ factors antigenicity The Blood Rh Factor Eighty five percent of the population have Rh antigens (Rh+) There are several Rh groups (factors, antigens) Three groups: Rh, C, D, and E, are of clinical importance An Rh- mother may develop antibodies against her Rh+ fetus The Rh- mother antibodies can pass to the Rh+ fetus resulting in hemolysis of its RBCs, a condition know as erythroblastosis fetalis This sequence usually occurs after the first pregnancy