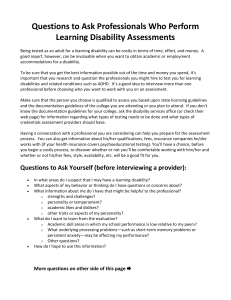
MALNUTRITION and DISABILITY
advertisement

MALNUTRITION and DISABILITY Dr Ingrid Bucens, Vientiane, May 2011. E 33% (mod) stunted emerging global priority More difficult to measure 23% screen positive for ‘significant disability’ 39% ‘not fulfilling developmental potential’ Layout of talk 1. MN – definitions, prevalence, consequences 2. Links between malnutrition and disability 3. Interventions for prevention and treatment of malnutrition related disability 4. Programmatic issues. Malnutrition – Classifications • Macronutrient (‘Protein-energy’) vs micronutrient • Degree - mild/moderate/severe – How far anthropometric measures deviate from normal • Rapidity of onset and duration – Acute (wasting +/– oedema) – Chronic (stunting) • Timing of onset / age group affected – In-utero – Childhood – Adult (life-long) Recognising Childhood Malnutrition TYPE ANTHROPOMETRIC MEASURE APPEARANCE UNDERWEIGHT WFA < -2SD Skinny WASTING WFH <- 2SD Very skinny WASTING + OEDEMA (WFH) OEDEMA Swollen, skin and hair abnormalities STUNTING (Chronic MN) HFA < -2SD Short (+/- skinny) MACRONUTRIENT (protein - energy) deficiency May not look abnormal May not look abnormal unless lined up against same age peers. Recognising Malnutrition in Mothers and Babies • MOTHERS – LOW BMI • < 18.5kg/m2 – MUAC • <20-25cm – SHORT • Height < 145cm • Chronic undernutrition. • BABIES – LBW (< 2.5kg) • ‘Mixed bag’ - Preterm + SGA – SGA (IUGR + others) Recognising MICRONUTRIENT deficiencies - IRON - - - Anaemia - Mucous membranes, nail changes - FOLIC ACID - Anaemia - IODINE - Endemic regions (mountains, non-iodinised salt) - Goitre ZINC - Skin rash + persistent diarrhoea (acrodermatitis enteropathica) VITAMIN A - Night blindness (not so easy to recognise in children) Prevalence • 33% stunting – Some regions ~ 50% • 10-19% mothers low BMI • 11% babies IUGR • 10% wasting – S Asia ~ 16% – Kwashiorkor less common – Severe wasting 3.5% • 45% children <5 yrs have anaemia ~ half due to iron deficiency HUGE NUMBERS OF MOTHERS, BABIES AND CHILDREN AFFECTED BY MALNUTRITION IN LOW AND MIDDLE INCOME COUNTRIES. CONSEQUENCES of Malnutrition • Individual (death, disease, disability) – DEATH – INFECTIONS • +/- death / disability – GROWTH FAILURE – ADULT HEALTH OUTCOMES • ‘Barker’ – DISABILITIES • Families / Generations – Growth – Reproductive health • Maternal complications and death • Small size at birth , disability outcomes – Educational / Economic • Societal – Economic • Burden of treatment • Loss of productivity – DALYS SIZE OF THE BURDEN Global deaths and disease burden measured in DALYS, in children < 5 yrs, attributed to nutritional status measures in 2004 21.4 21.2 Lancet (2008) Maternal and Child Undernutrition Series, 1st paper. THE LINKS TO DISABILITY 1. Common risk factors / root causes a. b. Psychosocial Biological 2. Disability is a cause of MN. 3. MN is a cause of disability. 4. Overlap of intervention strategies. Link 1:- Common multiple risks • The common milieu of MN and disability – WHO ‘The Critical Link’ • Common mechanisms (CARING) are important for healthy physical growth and psychological development. • Children in low resource contexts (POVERTY) are often exposed to multiple, cumulative risks which compromise caring – and therefore compromise both growth and development. The link between poverty and disability, +/- via Malnutrition. MALNUTRITION POVERTY Insufficient food -Low (maternal) education - Overcrowding -Poor sanitation -Poor health practices:breastfeeding, diet , reproductive health (FP), care-seeking, toxins (alcohol) -Infections / diseases -Maternal stress -(‘Poor parenting’) -Weak health services -etc DISABILITY Other -Trauma -Genetic -Metabolic -Asphyxia -etc Many of the ‘causes’ / risks are common MALNUTRITION DISABILITY MALNUTRITION POVERTY and associated risks – overcrowding, poor sanitation, low maternal education, poor health practices (breastfeeding), maternal stress and depression, stress, ill health, poor parenting skills (orphans), weak health services etc Poor reproductive health (extremes maternal age, no child spacing) Infections – TB, HIV, malaria (anaemia, cerebral infection) Poor health seeking behaviour (immunisations, care of illness) Breastfeeding inadequate Feeding practices inadequate Neonatal ills (jaundice, asphyxia, preterm) Recurrent diarrhoea Genetic, consanguinity, chromosomal, congenital microcephaly Environmental toxins (lead) TRAUMA LINK 2 Disability is a direct cause of MN. • Children with disability often develop MN – Babies suck poorly – breastfeeding failure – Less actively seek food (motor, sensory, cognitive) – Neglected by ‘carers’ – Rejected by society – Develop secondary illnesses which in turn cause MN (TB) LINK 3 Malnutrition is a cause of disability MN POVERTY DISABILITY Risks – milieu of poverty other ?How much disability from MN is directly due to MN and how much is due to the co-existing risks? • MN directly causes disability – Stunting – Wasting – Micronutrient deficiencies • Iodine • Vit A • Folic acid • Iron • MN indirectly causes disability – IUGR – Maternal Vitamin A deficiency and DISABILITY • May cause irreversible blindness. • Vit A related blindness is a VERY common cause of blindness in low resource countries. Iron deficiency and DISABILITY • Children who are not otherwise malnourished but who have iron deficiency and iron deficiency anaemia have impaired cognitive development and behaviour when compared to non-iron deficient children. • They score lower on cognitive, motor and behavioural tests. • Association is less consistent or less strong for iron deficiency without anaemia. Folic Acid and Disability • Spina bifida (neural tube defect, myelomeningocoele) +/- hydrocephalus • Vit B12 IODINE deficiency and disability • Iodine is needed for thyroid hormone, essential for brain development. • Irreversible severe intellectual disability (and stunting) in offspring of deficient mothers. • Lesser but significant cognitive impairment in children in iodine deficient areas. • Iodine deficiency is endemic in mountain populations without iodinised salt. Congenital hypothyroidism SEVERE ACUTE MALNUTRITION and DISABILITY • Children hospitalised with SAM (+/-oedema) consistently have developmental and behavioural abnormalities. – Cognitive scores lower – Motor lower – Behaviour markedly abnormal • No specific deficits. • With rehabilitation behaviour virtually returns to normal; other developmental deficits persist. • Children /adolescents who were earlier hospitalised for acute MN show persistent deficits in cognition, school function including behaviour – attention - social interaction. • How much of the deficit is due to associated stunting and the social milieu at home? Stunting and DISABILITY • Strong evidence for association between early childhood stunting and significant cognitive impairment (moderate to large effect). • Concurrent and longterm association, through to adulthood. – Young child height correlates to cognition at 40y! • Poorer development, lower IQ, poorer school performance even after controlling for confounders (social milieu). No specific deficit. • Younger children also have emotional and behavioural, attentional problems and relationships at school. • Individual and population level. IUGR and disability • Some studies found cognitive deficits in infancy for IUGR babies vs normally nourished newborns. • Review of IUGR studies, controlling for confounding (preterms, other neonatal problems eg asphyxia, causes of IUGR, home environment, quality of NBC) concluded that, provided no secondary asphyxia, there is little effect of IUGR on developmental outcome. Maternal malnutrition and DISABILITY • No direct link between maternal malnutrition and disability however – Maternal malnutrition is a cause of IUGR which may lead to stunting. – Maternal malnutrition increases the risk of maternal death (delivery complications) • ‘Motherless children don’t do well’ (malnutrition and disability). Orphan studies. LINK 4 Interventions for MN + disability. MN DISABILITY POVERTY MILIEU OF POVERTY At risk kids OTHER 1. Interventions for root causes will reduce MN and disability of all causes. 2. Interventions which prevent MN will prevent disability due to MN. 3. Interventions which treat MN reduce reversible disability due to MN. 4. Interventions for disability may also improve growth. 5. Combined interventions are most effective. Nutrition interventions • PREVENTIVE – Supplementation • Micronutrient • Macronutrient (food / milk) – Health education • • • • Breastfeeding Complementary Sanitation / hygiene Disease prevention – HIV, IPT, zinc, BCG • STIMULATION – Root cause strategies • Poverty alleviation • Food security • Family planning • ‘CURATIVE’ – Treatment of acute severe MN (in/outpatient) – Supplementation for catch up growth for IUGR and stunting – Micronutrients • Vit A, iron, folic acid • Iodine, zinc – Health education – STIMULATION Prevention strategies for Micronutrient deficiency/disability. Micronutrient deficiencies cause severe and often irreversible disability. Effective prevention strategies exist for at risk populations. • Vit A – Regular supplements to children. • Iron supplementation (fortification) – Prevents iron deficiency and anaemia. – Improves developmental outcomes. – Is recommended for young children except in malaria endemic areas. – Deworming • Folic acid supplementation pre-conception in all contexts prevents folate deficiency and related disability. • Iodine – Antenatal supplements (oil or inject) begun before T2 reduces stillbirths, prevents congenital hypothyroidism and improves childhood cognitive outcomes even for subclinical deficiency. – Childhood supplementation (oil) may improve cognition but results mixed. Supplementation at school recommended for girls. – Universal salt iodinisation is a very effective strategy. Treatment for micronutrient deficiencies/disability. • Except for iron for school aged children with IDA, these strategies are less effective. – Iron • May not fully reverse the developmental disability in infants /preschool children with IDA. • In school age deficits are reversible. – Iodine – lesser grades of disability may be improved if treatment started early. – Vitamin A – only early eye changes are reversible. – Folic acid disability is not reversible. Preventing IUGR and childhood MN • IUGR can be reduced with – Antenatal supplementation interventions • Childhood MN can be prevented – Antenatal interventions – Interventions in infancy / very early childhood – These interventions, in turn, reduce maternal malnutrition • Via prevention of childhood stunting Preventive interventions. • Food to pregnant / lactating women / infants • • • • Food is more effective than individual micronutrients. Improves birthweight. Improves infant growth and prevents stunting Improves developmental outcomes in infancy and the benefit may be sustained • Stimulation interventions pregnancy / postnatally • Improve developmental outcomes • May improve growth • Food + stimulation • May improve growth better than food alone • Has a greater effect on cognition than either intervention alone. These interventions have most effect if interventions begin in pregnancy or at birth and continue through 2-3 years. More effective in populations at risk of malnutrition including maternal MN and IUGR. Treatment interventions The developmental disability of MN is partly reversible. • FOOD – Reverses weight loss of wasting – Stunting is more difficult to reverse; may improve if food supplementation before 3 years. – Concurrent benefits on motor and cognitive development. May be sustained, especially if begun < 2 yrs, but evidence limited. – Effect on development is not as strong as with preventive interventions. • STIMULATION – Benefits development • FOOD + STIMULATION – May improve growth better than food alone. – Significantly improves cognitive development in wasting and stunting. • Do not reach level of normally nourished • Effect on development is sustained – Best results on growth and cognition if begin < 2yrs. SUPPLEMENTATION + STIMULATION for stunting Stunted children have long term deficits in cognition. Deficit improved by stimulation +supplementation, but not to normal. Walker SP, Chang SM, Gratham-McGregor SM. Effects of early childhood psychosocial stimulation and nutritional supplementation on cognition and education in growth-stunted Jamaican children: prospective cohort study. Lancet 2005; 366: 1804-07. ‘Developmental intervention’ for children with MN is more effective if begun < 2yrs. L3 …. Developmental interventions • Benefits – Lots of evidence of effectiveness in improving developmental outcomes, school readiness and educational outcomes. – Effective in developing world settings – May improve nutritional status • Interventions are most effective if – – – – – Target populations / groups most likely to benefit (MN) Input is intensive - targets both children and carers Begun antenatally and continued for at least 3 years Good quality Delivered together with nutritional intervention! The mutual reinforcement of nutritional and developmental interventions. • Developmental interventions hope to – Improve the way mothers CARE for their children • includes caring for feeding, hygiene, health seeking • become more responsive to children’s needs • Nutrition interventions make children stronger – child can benefit more from his environment – can elicit more care Key messages. • MN and disability are both highly prevalent and co-exist in poor populations. • Both may be the result of the risks that co-exist in poverty and each may cause or aggravate the other. • Early growth impacts cognitive development • Effects of MN and malnutrition induced disability (educational failure) are perpetuated through generations, for biological and environmental reasons. • The economic consequences of this are very significant and government, including non-health sectors, need to be aware of this. • Interventions for each affect the other. The most effective interventions for both MN and disability are those which include both a nutritional and developmental component. • Preventive interventions are more effective than treatment because some malnutrition induced disability is irreversible. • Interventions are most effective if begun during pregnancy or the first two years (most intensive periods of both growth and development) and if they target at-risk populations. Considerations for programming • Examine existing MNCH systems and services from a life cycle approach – Review what is being done that affects MN and / or disability – Are there any key intervention gaps? • Consider if your health system can improve efficiency or can feasibly increase interventions – Combine interventions that target similar ages and are to be delivered by same HW – Select priorities based on local epidemiology (Iodine, bed nets) – Beware high cost and complex interventions – Phase in changes and target risk groups • Multi-sectoral collaboration (education, root causes) EG. Preventing malnutrition + disability PRECONCEPTIONAL PRENATAL NEONATAL EARLY YEARS POVERTY REDUCTION / WATSAN/EDUCATION/ACCESS to HEALTH SERVICES Salt iodinisation; ?iron or folate fortification Health Education -Reproductive Supplement at risk mothers Supplement at risk mothers Supplementing Family Planning (adolescent pregnancy) ‘Stimulation’ Parent education Newborn screening Iron, zinc, vitA, deworm Iron/folate Iodine, Fefol At risk FU (LBW) ‘Stimulation’ ECD ANC, counsel, bed nets SBA, EMONC Parent education at risk NBC/PNC Growth/development monitoring and counseling Breastfeeding IMCI/referral/danger sign awareness / vaccination Most important messages of all. •Preventing malnutrition (in its various forms) is a priority for reducing the burden of disability in low resource contexts. A WELL BALANCED DIET AND A STIMULATING ENVIRONMENT ARE GOOD FOR CHILDREN!