Assessment of Iron, Porphyrins and Others
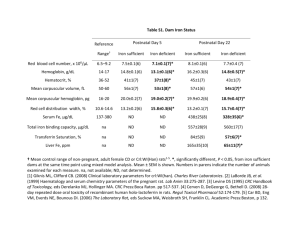
advertisement

MLAB 2401: Clinical Chemistry Keri Brophy-Martinez Chapter 5: Assessment of Iron, Porphyrins and Others Specimen Requirements: Iron Studies Serum without anticoagulant – Plasma with heparin ( check product insert) – – Oxalate, citrate or EDTA binds Fe ions, so they are unacceptable – Early morning sample preferred due to diurnal variation – No hemolysis Iron Study/Profiles Three Components ◦ Total Iron ( serum ) ◦ TIBC ◦ % Iron Saturation ( Fe Sat ) Total Iron % Fe Saturation x 100 TIBC The Iron Saturation is a measurement of how “full” transferrin is 3 Assessing Iron Levels and Forms Directly measured ◦ Iron ◦ Transferrin Beta globulin formed in the liver Measured by the amount of iron it can bind ◦ Ferritin Best diagnostic test for IDA Acute phase reactant Assessing Iron Levels and Forms • Indirect measure – TIBC (Total iron-binding capacity) • Measures the total amount of iron that apotransferrin can bind • Can be expressed as a percentage(percent saturation) • Ratio of serum iron to TIBC • Increased – Late pregnancy – IDA – Following hemorrhage – Following destruction of liver cells • Decreased – Decreased synthesis of transferrin – Increased loss of urine proteins Test Methodologies: Iron • Colorimetric Procedure – Separate Fe from transferrin with a strong acid – Iron is reduced from ferrous(Fe3+) to ferric(Fe2+) state – Addition of a chromogen creates a colored compound – Measurement of colored product by spectrophotometry Iron Reference Ranges – – Diurnal variation Men: 65-165 µg/dL – Decreased Levels • Decreased intake • Increased need • Increased loss – Increased Levels – Women: 45-160 µg/dL • • • • • • Increased absorption Hemolytic anemia Lead poisoning Pernicious anemia Megaloblastic anemia Hepatitis Test Methodologies:TIBC Pre-treatment and Colorimetric Method 1. Add Fe3+ to saturate binding sites on transferrin 2. MgCO3 is added to remove unbound Fe3+ 3. Mixture is centrifuged and the supernatant tested using the serum iron methodology Reference Ranges Transferrin ◦ 200-360 mg/dL Ferritin ◦ Male: 20-250 ng/mL ◦ Female: 10-120 ng/mL TIBC ◦ 250-425 µg/dL % saturation ◦ 15-55 Test Methodology: Hemoglobin Electrophoresis ◦ Discussed in separate unit Test Methodology: Porphyrins Screening tests ◦ Urinary PBG ◦ Urinary ALA ◦ Urinayr porphyrins Quantitative Assays ◦ URO ◦ PROTO ◦ COPRO Serve to classify porphyrias Lab Methods Watson-Schwartz for Urinary PBG( porphobilinogen) ◦ Screen for acute intermittent porphyria ◦ Specimen Qualitative: fresh morning urine Quantitative: 24 hour collection ◦ Reference Range <2 mg/daily Watson-Schwartz Principle ◦ PBG + Ehrlich’s reagent results in a red-orange chromogen ◦ Interferences Urobilinogen indole Lab Methods: HgbA1c Electrophoresis Enzymatic Assays HPLC ◦ Goal is to separate hemoglobin forms within a column. Then, glycated versus total hemoglobin can be measured spectrophotometrically ◦ Specimen requirements EDTA whole blood Can be non-fasting Reference range ◦ 4.0-6.0% Lab Methods: Myoglobin Procedures incorporate the binding of specific antibodies to myoglobin with a resulting chemical or physical change that can be measured and correlated to myoglobin concentration Specimen requirements ◦ Usually plasma ( check product insert) Specimen Requirements: Lead Whole blood ◦ Why? Circulating lead found in the RBC ◦ Venous sample preferred but capillary sample can be used ( must confirm positive on capillary) ◦ Royal blue top with EDTA anticoagulant ◦ Lead-free containers Urine Lab Method: Lead Test methodologies ◦ AAS ◦ Anodic stripping voltammetry Reference Ranges in blood ◦ Children< 10 µg/dL