Skeletal System
advertisement
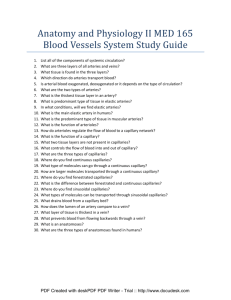
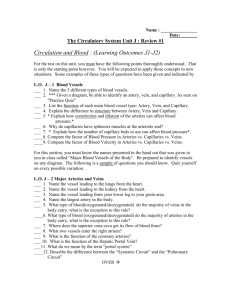
The Cardiovascular System: Blood Vessels Chapter 19 Introduction The blood vessels of the body form a closed delivery system that begins and ends at the heart Often compared to a plumbing system, it is a far more dynamic system of structures that pulse, constrict and relax and even proliferate to meet changing body needs Blood Vessel Structure & Function The major types of blood vessels are – Arteries • The large distributing vessels that bring blood to the body – Capillaries • The tiny vessels that distribute blood to the cells – Veins • The large collecting vessels that bring blood back to the heart Intermediate vessels connect – Arterioles bring blood to the capillaries – Venules drain blood from the capillaries Blood Vessel Structure & Function The pattern of distribution starts with arteries to arterioles to capillaries to venules to veins The blood vessels in the adult human body carry blood in a distribution network that is approximately 60,000 miles in length Only capillaries come into intimate contact with tissue cells and serve cellular needs Structure of Blood Vessel Walls Blood Vessel Walls The walls of blood vessels are composed of three distinct layers or tunics The tunics surround a central opening called a lumen Blood Vessel Walls The innermost tunic is the tunica intima This tunic contains the endothelium, the simple squamous endothelium that lines all vessels Its flat cells fit closely together, forming a slick surface that minimizes friction as blood moves through the vessel lumen Tunica adventitia Blood Vessel Walls In blood vessels larger than 1 mm in diameter, a subendothelial layer of loose connective tissue, subendothelial layer, (basement membrane) supports the endothelium Blood Vessel Walls The middle tunic, the tunica media, is mostly circularly arranged smooth muscle cells and sheets of elastin The activity of the smooth muscle is regulated by vasomotor nerve fibers of the sympathetic division of the autonomic nervous system Tunica media Blood Vessel Walls Depending on the needs of the body, the vasomotor fibers can cause vasoconstriction or vasodilation The activities of the tunica media are critical in regulating circulatory dynamics Generally, the tunica media is the bulkiest layer in arteries, which bear the chief responsibility for maintaining blood pressure and continuous blood circulation Blood Vessel Walls The outermost layer of a blood vessel is the tunica externa This tunic is composed largely of loosely woven collagen fibers that protect blood vessels and anchor it to surrounding structures Tunica externa Blood Vessel Walls The tunica externa is infiltrated with nerve fibers and lymphatic vessels and, in larger vessels, a system of tiny blood vessels These vessels, the vasa vasorum nourish the external tissues of the blood vessel wall Tunica externa Arteries Arteries are vessels that carry blood away from the heart All arteries carry oxygen rich blood with the exception of those in the pulmonary circuit Blood proceeds to the tissues through – Elastic arteries – Muscular arteries – Arterioles Elastic (Conducting) Arteries Elastic arteries are thick walled arteries near the heart - the aorta and its major branches These arteries are the largest in diameter and the most elastic A large lumen allows them to serve as low resistance pathways that conduct blood from the heart to medium-sized arteries and thus are called conducting arteries Elastic (Conducting) Arteries The elastic arteries contain more elastin than any other type of vessel While present in all three layers, the tunica media contains the most The abundant elastin enables these arteries to withstand and smooth out large pressure fluctuations by expanding when the heart forces blood into them and then recoiling to propel blood onward into the circulation when the heart relaxes Elastic (Conducting) Arteries Elastic arteries also contain substantial amounts of smooth muscle, but they are relatively inactive in vasoconstriction Because elastic arteries expand and recoil passively to accommodate changes in blood volume, the blood is kept under pressure Thus, blood flows continuously rather than starting and stopping with each heart beat Muscular (Distributing) Arteries The muscular distributing arteries deliver blood to specific body organs and account for most of the named arteries Proportionately, they have the thickest media of all vessels Their tunica media contains relatively more smooth muscle and less elastic tissue than that of elastic arteries They are more active in vasoconstriction and are less distensible Muscular (Distributing) Arteries As in all vessels, concentric sheets of elastin occur within the tunica media of muscular arteries although these sheets are not as thick or abundant as those of elastic arteries Muscular (Distributing) Arteries A feature unique to muscular arteries, especially thick sheets of elastin lie on each side of the tunica media An external elastic lamina lies between the tunica media and tunica externa Muscular (Distributing) Arteries The elastin in muscular arteries, like that in elastic arteries, helps dampen the pulsatile pressure produced by the heartbeat Arterioles Arterioles have a lumen diameter from 0.3 mm to 10 m, and are the smallest of the arteries Larger arterioles exhibit all three tunics, but their tunica media is chiefly smooth muscle with a few scattered muscle fibers The smaller arterioles that lead into capillary beds, are little more than a single layer of smooth muscle cells spiraling around the endothelial lining Arterioles The diameter of each arteriole is regulated in two ways: – Local factors in the tissues signal the smooth musculature to contract or relax, thus regulating the amount of blood sent downstream to each capillary bed – Sympathetic nervous system adjusts the diameter of arterioles throughout the body to regulate systemic blood pressure Capillaries The microscopic capillaries are the smallest blood vessels In some cases, one endothelial cell forms the entire circumference of the capillary wall The average length of a capillary is 1 mm and the average diameter is 8-10 m Capillaries Capillaries have a lumen just large enough for blood cells to slip through in single file Capillaries Capillaries are the body’s most important blood vessels because they renew and refresh the surrounding tissue fluid (interstitial fluid) with which all cells in the body are in contract Capillaries deliver to interstitial fluid the oxygen and nutrients that cells need while removing carbon dioxide and nitrogenous wastes that cells deposit in the fluid Capillaries Given their location and the thinness of their walls capillaries are ideally suited for their role of providing access to nearly every cell Along with the universal functions just described some capillaries also perform site-specific functions – – – – Lungs: gas exchanges Endocrine glands: pick up hormones Small intestine: nutrients Kidneys: removal of nitrogenous wastes Capillary Beds A capillary bed is a network of the body’s smallest vessels that run throughout almost all tissues, especially the loose connective tissue This flow is also called a microcirculation Capillary Beds In most body regions, a capillary bed consists of two types of vessel a vascular shunt (metaarteriole) and true capillaries Capillary Beds The terminal arteriole leads into a metarteriole which is directly continuous with the thoroughfare channel Capillary Beds The thoroughfare channel joins the postcapillary venule that drains the capillary bed Capillary Beds The true capillaries number 10 to 100 per capillary bed, depending on the organ served Branch from metarteriole to thoroughfare channel Capillary Beds A cuff of smooth muscle fibers, called a precapillary sphincter surrounds the root of each capillary at the metarteriole and acts as a valve to regulate the flow of blood into the capillary Capillary Beds When the precapillary sphincters are relaxed, blood flows through the true capillaries and takes part in exchanges with tissue cells Capillary Beds When the precapillary sphincters are contracted, blood flows through the shunts and bypasses the tissue cells Capillary Beds Most tissues have a rich supply, but there are a few exceptions – – – – Tendons and ligaments / poorly vascularized Cartilage / from adjacent connective tissue Epithelia / from adjacent connective tissue Cornea / nourished by aqueous humor Capillary Beds The relative amount of blood entering a capillary bed is regulated by vasomotor nerve fibers and local chemical conditions A capillary bed may be flooded with blood or almost completely bypassed, depending on conditions in the body or in that specific organ Example of shunting blood from digestive organs to skeletal muscles Capillary Permeability The structure of capillaries is well suited for their function in the exchange of nutrients and wastes between the blood and the tissues through the tissue fluid A capillary is a tube consisting of thin endothelial cells surrounded by a basal lamina The endothelial cells are held together by tight junctions and occasional desmosomes Capillary Permeability Tight junctions block the passage of small molecules, but such junctions do not surround the whole perimeter of the endothelial cells Instead, gaps of unjoined membrane called intercellular clefts occur through which small molecules exit and enter the capillary Capillary Permeability External to the endothelial cells, the delicate capillary is strengthened and stabilized by scattered pericytes Capillary Permeability The pericytes are spider shaped cells whose thin processes form a network that is widely spaced so as to not to interfere with capillary permeability Capillary Permeability Structurally there are three types of capillaries – Continuous – Fenestrated – Sinusoidal Continuous Capillaries Continuous capillaries are abundant in the CNS, skin and muscles and are the most common They are continuous in the sense that their endothelial cells provide an uninterrupted lining Continuous Capillaries Adjacent cells are joined laterally by tight junctions However, these are usually incomplete and leave gaps of unjoined membrane called intracellular clefts that are just large enough to allow limited passage of fluids Fenestrated Capillaries Fenestrated capillaries have fenestrations (pores) spanning the endothelial cells Fenestrated capillaries occur only where there are exceptionally high rates of exchange of small molecules between blood and the surrounding tissue Fenestrated Capillaries The fenestrations are usually covered by a thin diaphragm but this variety has much greater permeability to fluids and small solutes Fenestrated capillaries are found where active capillary absorption or filtrate formation occurs Fenestrated Capillaries Fenestrated capillaries are found in the small intestine to receive digested nutrients These capillaries are also found in the synovial membranes of joints to allow water molecules to exit the blood to form synovial fluid Intercellular clefts Routes of Capillary Permeability Molecules pass into and out of capillaries via four routes – Direct diffusion through endothelial cell membranes – Through the intercellular clefts – Through cytoplasmic vesicles or caveolae – Through fenestrations in fenestrated capillaries Routes of Capillary Permeability Most exchange of small molecules is thought to occur through intercellular clefts Caveolae apparently transport a few larger molecules, such as small proteins Carbon dioxide and oxygen seem to be the only important molecules that diffuse directly through endothelial cells because these uncharged molecules easily diffuse through lipid containing membranes of cells Low Permeability Capillaries The blood-brain barrier prevents all but the most vital molecules(even leukocytes) from leaving the blood and entering brain tissue The blood-brain barrier derives its structure from the capillaries of the brain Brain capillaries have complete tight junctions, so intercellular clefts are absent Low Permeability Capillaries Brain capillaries are continuous, not fenestrated and they also lack caveolae Vital capillaries that must cross brain capillaries are “ushered through” by highly selective transport mechanisms in the plasma membranes of the endothelial cells Sinusoidal Capillaries Some organs contain wide, leaky capillaries called sinusoids Each sinusoid follows a twisted path and has both expanded and narrowed regions Sinusoidal Capillaries Sinusoids are usually fenestrated and their endothelial cells have fewer cell junctions than do ordinary capillaries Sinusoidal Capillaries In some sinusoids the intercellular cleft is wide open Sinusoids occur wherever there is an extensive exchange of large materials, such as proteins or cells, between the blood and surrounding tissue Sinusoidal Capillaries Sinusoids are found in only in bone marrow and spleen, where many blood cells move through their walls The large diameter and twisted course of sinusoids ensure that blood slows when flowing through these vessels, allowing time for the many exchanges that occur across their walls Veins Veins are the blood vessels that conduct blood from the capillaries back to the heart Because blood pressure declines substantially while passing through the high-resistance arterioles and capillary beds, blood pressure in the venous part of the circulation is much lower than in the arterial part Veins Because they need not withstand as much pressure, the walls of veins are thinner than those of comparable arteries The venous vessels increase in diameter, and their walls gradually thicken as they progress from venules to the larger and larger veins leading to the heart Venules Venules, ranging from 8 to 100 m in diameter are formed when capillaries unite The smallest venules, the postcapillary venules, consist of endothelium on which lie pericytes Venules Venules join to form veins With their large lumens and thin walls, veins can accommodate a fairly large blood volume Up to 65%of the body’s total blood supply is found in the veins at any one time although the veins are normally only partially filled with blood Veins externa Veins have three distinct tunics, but their walls are always thinner and their lumens larger than those of corresponding arteries There is little smooth muscle even in the largest veins Veins The tunica externa is the heaviest wall layer and is often several times thicker than the tunica media In the venae cavae, the largest veins, which return blood directly to the heart the tunica externa is further thickened by longitudinal bands of smooth muscle Tunica externa Veins Veins have less elastin in their walls than do arteries, because veins do not dampen any pulsations (these have been smoothed out by the arteries) Because blood pressure within veins is low, they can be much thinner walled than arterioles without danger of bursting Veins Low-pressure conditions demand some special adaptations to help return blood to the heart at the same rate as it was pumped into circulation One structural feature that prevents the backflow of blood away from the heart is the presence of valves within veins Veins Venous valves are formed from folds of the tunica intima and they resemble the semilunar valves of the heart in structure and function Venous valves are most abundant in the veins of the limbs, where the upward flow of blood is opposed by gravity Veins A few valves occur in the veins of the head and neck, but none are located in veins of the thoracic and abdominal cavities A functional mechanism that aids the return of venous blood to the heart is the normal movement of our body and limbs Veins Another mechanism of venous return is called the skeletal muscular pump Here contracting muscles press against the thin-walled veins forcing valves proximal to the contraction to open and propelling the blood toward the heart Vascular Anastomoses Where vessels unite or interconnect, they form vascular anastomoses Most organ receive blood from more than one arterial branch and arteries supplying the same area often merge, forming arterial anastomoses Arterial anastomoses provide alternative pathways called collateral channels for blood to reach a given body region Vascular Anastomoses If one arterial branch is blocked arterial anastomoses provide the region with an adequate blood supply Arterial anastomoses are abundant in abdominal organs and around joints, where active movement may hinder blood flow through one channel Vascular Anastomoses Anastomoses are also prevalent in the abdominal organs, brain, and heart Because of the many anastomoses among the smaller branches of the coronary artery in the heart wall, a coronary artery can be 90% occluded by atherosclerosis (plaque) before a myocardial infarction (heart attack) occurs Vascular Anastomoses Arteries that do not anastomose, or which have a poorly developed collateral circulation (retina, kidneys, spleen) may be vulnerable if their blood flow is interrupted Veins anastomoses much more freely than arteries and because of abundant collateral circulation occlusion of a vein rarely blocks blood flow leading to tissue death Vasa Vasorum The wall of the blood vessels contain living cells and therefore require a blood supply of their own For this reason the larger arteries and veins have tiny arteries, capillaries and veins in their tunica externa These tiny vessels the vasa vasorum nourish the outer half of the wall of a large vessel with the inner half being nourished by the blood in the lumen End of Material Chapter 19