BOrganic
advertisement
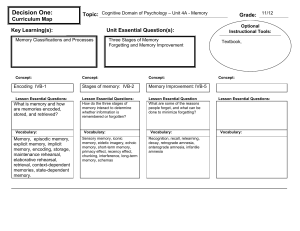
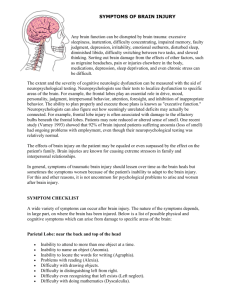
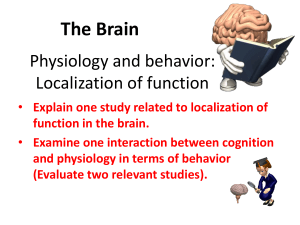
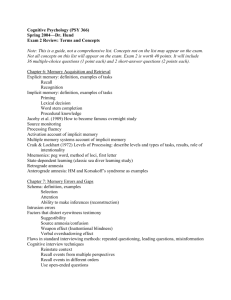
PSY 335 Memory and Amnesia Memory Disorders Influences on Memory Alcohol – Bits & Pieces Stress -- Kolb & Whishaw Seg 32 (CD 2) Diabetes – Kolb & Whishaw Ch 13 Seg 6 (CD 3) Kinds of Memory Disorders Organic – having a physical cause Functional – having a psychological cause Dys (as a prefix) means difficulty or limited ability to perform. A (as a prefix) means complete inability or lack of a function. Alcohol & Memory Alcoholic amnesia – alcohol prevents consolidation so nothing is remembered and no memory can be recovered. Alcoholic blackout – state-dependent memory, so recall is possible if one is back in the same state. Because many crimes are committed while drunk, memory failure is frequently blamed on alcohol. Sleep & Memory New sleep studies suggest a "memory lifecycle” with three stages - stabilization, consolidation, and re-consolidation. • • • Initial stabilization takes up to 6 hours. Sleep needed for consolidation, deep non-REM Alcohol disrupts consolidation Sleep deprivation produces effects similar to aging. • Procedural memory and recognition memory are most strongly affected. Sources of Organic Dysfunction Accident Disease • Car accidents and other injuries (e.g., N.A.) • War • Encephalitis (viral) – inflammation of the lining • • • of the brain, causing swelling. Stroke Alzheimer’s disease Korsakov’s syndrome (prolonged alcoholism) Alzheimer’s Disease A fatal degenerative disease caused by cell failure – neurofibrillary tangles and plaques that interfere with cell function. • All areas of the brain are eventually affected, but frontal lobes and memory go first. Confusions and memory problems do not resemble normal aging, amnesia or other memory problems. Classification of Disorders See Rivermead Behavioural Memory Test (RBMT) pg 263, Table 11.1 and Wechsler Memory Scale -- tests used to assess memory problems. Disorders classified by type of symptom: • Generalizing – confusion, fuzziness, mental • slowing. Localizing – few generalizing symptoms but impairment of specific functions. Clusters of symptoms are a syndrome. • Concern about symptoms is a symptom itself. Frontal Lobe Deficits Confabulation – production of a false memory. • Momentary confabulation – responses that • could be correct. Fantastic confabulation – responses clearly fictional. Source amnesia – fact is remembered but not the source. Memory of temporal order. Frontal Lobe Deficits (Cont.) Impaired recall – more “ugly stepsisters,” no categorization. Metamemory is impaired, including FOK (feeling of knowing) judgments and monitoring of search. False recognization: • Increased false alarms • Increased intrusions Frontal Lobe Deficits (Cont.) Faulty encoding and poor representation may be a cause of poorly focused search. • Information is needed to guide search. The left frontal lobe guides encoding. The right frontal lobe guides retrieval. Frontal Lobe Deficits (Cont.) Emotional deficits: Impaired awareness of memory loss: If confabulations are believed by others, there is no feedback on normalcy. • Cognitive apathy, lack of motivation • Flattened affect • Inaccurate assessment of performance • Lack of distress Alien Hand (Anarchic Hand) Syndrome – a Frontal Lobe Deficit Peter Sellars in “Dr. Strangelove: or How I learned to story worrying and love the bomb” Damage to the Parietal Association Cortex Confusion about directions, inability to use words describing spatial relations: • Under, up, down Inability to name body parts or point to parts of the body. Capgras syndrome (rt. Posterior parietal) inability to recognize close family members • • Sometimes animals or even furniture Invasion of the body snatchers Reading & Writing Disorders Alexia – inability to read Agraphia – inability to write Caused by damage to the left angular gyrus which integrates information from the sensory modalities. Pure Word Deafness A person can hear and speak, read and write normally but cannot understand speech. Occurs with bilateral destruction of the auditory cortex or disconnection from Wernicke’s area. Because Wernicke’s area is not damaged, speech produced is OK. Perceptual Deficits Aphasia – involves inability to name something. Agnosia – involves inability to recognize something. Visual agnosias – inability to combine individual visual impressions into complete patterns. Types of Visual Agnosias Object agnosia – inability to recognize common objects. Prosopagnosia – inability to recognize faces. Kolb & Wishaw Disc 3, segment 1 Color agnosias: • Achromatopsia (cortical color blindness) • Color anomia – inability to name colors. • Color agnosia – inability to recognize colors Other Agnosias Amusia – tone deafness, melody deafness, disorders of rhythm, measure, tempo. Astereoagnosia – inability to recognize the nature of an object by touch. Asomatoagnosia – knowledge of one’s own body. • Indifference to illness, asymbolia for pain Pure Anomia Loss of memory of words (anomic aphasia) • Cannot name pictures of common objects • Difficulty reading and writing Produced by damage to either Broca’s or Wernicke’s area (fluent anomia). Use circumlocutions to get around missing words. Broca’s Aphasia Broca’s area may contain memories of the movements needed to produce speech. Produces three deficits: • • • Anomia – word-finding difficulty Agrammatism – loss of grammatical construction Difficulty with articulation Slow, laborious, nonfluent speech without function words with with content words. Conduction Aphasia Disruption of verbal short term memory due to damage to the subcortical axons that connect Broca & Wernicke’s areas. Results in poor repetition – only meaningful words can be repeated (through other means). • Non-words cannot be repeated (blaynge). Amnesic Syndrome Short term memory is intact (unimpaired) Anterograde amnesia present affecting both recognition and recall tasks. Retrograde amnesia present, but extent varies. Semantic memory largely intact but can be affected by antero & retro amnesias. Procedural memory is intact. Causes of Amnesic Syndrome Damage to: Herpes simplex encephalitis Korsakoff’s syndrome (thiamine deficiency plus chronic alcoholism) Direct injury (H.M., N.A.) • Hippocampus • Temporal cortex (adjacent to hippocampus) • Diencephalon (especially mamillary bodies) Anterograde Amnesia No new declarative information can be added to long-term memory Events from the present are quickly forgotten Usually accompanied by retrograde amnesia. Performance on IQ tests is unimpaired because it relies on info learned in past. Retrograde Amnesia Declarative information from the past is forgotten. Information is forgotten in a temporal gradient (based on time): • • Ribot’s law – newer information forgotten first. Both semantic and episodic information show this gradient. Difficult to test due to differences in life experiences, impairment varies. Focal Retrograde Amnesia Loss of remote memory unaccompanied by anterograde amnesia. May occur when the temporal cortex is damaged but not the hippocampus. Cases reported without head injury and with loss of procedural memory are probably malingering (faking). Evidence for Implicit Memory Alzheimer’s patients show impaired priming. Huntington’s Chorea patients show normal priming but impaired procedural memory. Procedural memory and priming are spared by amnesia.