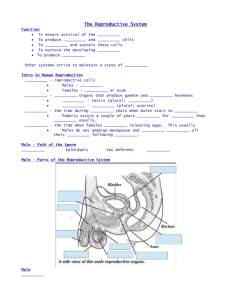
Chapter 18
The reproductive system
Physiologic Concepts
Spermatogenesis
Spermatogenesis (the formation of sperm)
begins during puberty and continues
throughout the lifetime of a male.
Undifferentiated germ cells lining the
seminiferous tubules undergo a programmed
number of mitotic cell divisions, resulting in
the production of the primary spermatocytes
(immature sperm), which ultimately develop
into the spermatozoa (mature sperm).
Spermatogenesis requires approximately 2
months. From each primary
spermatocyte, four viable sperm (each
with 23 chromosomes) are produced.
Spermatogenesis occurs in the
seminiferous tubule under the control of
two pituitary hormones folliclestimulating hormone (FSH) and
luteinizing hormone (LH) and the sex
hormones, primarily testosterone.
Follicle-Stimulating Hormone
FSH is a protein hormone released from the
anterior pituitary in response to a stimulating
hormone from the hypothalamus: gonadotropin-releasing hormone (GnRH) . The final
effect of FSH is to cause proliferation and
differentiation of the immature sperm.
Luteinizing Hormone
LH is the second protein hormone released from
the anterior pituitary in response to
stimulation by GnRH. LH stimulates the
synthesis of the steroid hormone testosterone
Stimuli Controlling GnRH Release
• GnRH is released in small pulses throughout the
day, resulting in relatively constant daily levels.
Increases or decreases in GnRH release may occur
seasonally and with different physical and
psychological conditions such as anxiety or
depression.
• Changes in the secretion of GnRH may affect sperm
formation by affecting LH and FSH and may alter
libido.
Male secondary sexual characteristics
Male secondary sexual characteristics are under the
control of the male androgens, especially
testosterone. The male secondary sexual
characteristics include the following:
• Increased protein anabolism and muscle mass.
• Increased bone growth and strength.
• Male pattern of hair on the face, axillary, and
pubic regions. Hair growth is thick on most areas
of the body.
• Increased metabolic rate, probably as a result of
increased protein anabolism (buildup) and
muscle mass formation. Increased metabolic rate
raises the caloric needs of males, beginning at
puberty, compared to females.
• Proliferation and activation of sebaceous
glands in the skin, which produce an oily
substance called sebum. Increased amounts of
sebum can cause acne, especially during
teenage years.
• A deepening voice, as a result of hypertrophy
of the larynx.
• Male pattern baldness, typically beginning
with a bald spot on the top of the head. A
genetic tendency influences male pattern
baldness.
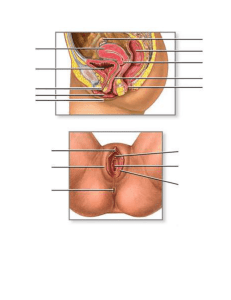
The Menstrual Cycle
The menstrual cycle is the cyclic maturation and
release of an ovum. It involves the growth of a
follicle, ovulation of the ovum, and characteristic
changes in the endometrial lining of the uterus.
Ovulation
On approximately day 12 of the menstrual cycle,
there is a dramatic rise (6- to 10-fold) in the
release of LH from the anterior pituitary. This rise
is called a preovulatory LH surge. FSH increases to
a lesser degree. Rising LH levels initiate a
profound, final growth of the follicle, and then
rupture, releasing the ovum into the abdominal
cavity.
Female Secondary Sexual Characteristics
The female secondary and associated sexual
characteristics are under the control of estrogen
and to a lesser extent progesterone .The female
secondary sexual characteristics include:
• Fully developed breasts.
• The female pattern distribution of pubic hair. The
growth of pubic and axillary hair in women is not
estrogen dependent, but occurs as a result of
adrenal gland androgen release.
Puberty
Puberty is the beginning of sexual maturation.
Puberty typically occurs at a younger age in girls
than boys. It begins in girls between 8 and 14
years of age, and in boys between 10 and 16
years of age. The menstrual cycle is the
culmination of puberty in girls. In boys, puberty
culminates in the ability to ejaculate mature
sperm.
Menopause
Menopause is defined only in retrospect, as a lack
of menstrual cycles for the previous 12 months. It
occurs in a woman when her ovaries no longer
respond to LH and FSH with estrogen and
progesterone production, and no longer release
an ovum
Pathophysiologic Concepts
Infertility
Infertility is the inability or reduced ability to produce
offspring. Infertility in a couple may result from
female factors (40 to 50%), male factors (30 to
40%), or a combination (20%). Infertility in a couple
may occur from the start of the relationship
(primary infertility) or after the couple has already
produced one or more offspring (secondary
infertility).
Female Factors
N.,B.Optimal fertility in women lasts to about 30
years of age and then begins to fall sharply with
increasing frequency as a woman ages.
- Problems with follicular growth, anovulation
(failure to ovulate), or ovulatory irregularities.
- Blockage of the fallopian tubes following pelvic
infection
- Presence of uterine abnormalities that prevent
implantation may be involved.
- Immune responses may destroy the implanted
embryo if the woman is either hyperimmune to
the embryo or fails to develop tolerance to it.
• Miscarriages later in gestation may occur if
the placenta is poorly placed or poorly
perfused with blood, or if the cervix cannot
support the weight of a growing fetus.
• Treatment of female infertility is specific to
the cause.
- Drugs to induce ovulation or superovulation
(more than one ovum) may be administered.
- Harvesting of eggs from the woman for in
vitro fertilization (outside of the body) may be
attempted. Eggs fertilized outside the body
may be implanted into the fallopian tube or
uterus.
Male Factors
May include :
-Defects in spermatogenesis that result in deformed
sperm or sperm too few in number to allow for
successful penetration of the ovum.
-Sperm motility (movement) may be impaired as well.
-Infection and scarring of the testicles, epididymis,
vas deferens, or urethra.
-Systemic infections, such as mumps, may cause
swelling of the testicles and destruction of the
seminiferous tubules.
-Obstruction of the blood vessels supplying the
testes can cause hypoxia and a failure of the
sperm to develop or survive.
- Autoantibodies produced against sperm may
reduce sperm number and quality.
- Exposure of the testicles to high temperature
may reduce spermatogenesis.
• Treatment of male factor infertility is specific to
the cause. For example, for a man with a low
sperm count, sperm may be obtained via
masturbation and then introduced artificially into
his female partner after techniques to increase
the concentration of the highest-quality sperm
have been performed. This process is called
artificial insemination.
Gynecomastia
Gynecomastia is the enlargement of breast tissue in
males. It can result from excess production of
estrogen in the male or the liver's inability to break
down normal male estrogen secretions.
Gynecomastia is frequently seen during early
puberty in some males and may be a normal
development or may be related to excess body
weight or a hormonal imbalance
Dysmenorrhea
Is painful menstruation that occurs without evidence
of pelvic infection or disease.
It is usually caused by excessive release of a specific
prostaglandin, from the uterine endometrial cells
which is a potent stimulator of myometrial smooth
muscle contraction and uterine blood vessel
constriction causing significant pain.
For most women, non-steroidal anti-inflammatory
drugs (NSAIDs) that inhibit prostaglandin
production, such as ibuprofen, can effectively
reduce cramping.
Prostaglandin inhibitors should be used at the first
sign of pain or at the first sign of menstrual flow.
Because forceful menstrual cramping may
contribute to the development of endometriosis
(painful growth of uterine tissue outside of the
uterus).
Complaints of dysmenorrhea should always be taken
seriously, and attempts should be made to reduce
its incidence.
Amenorrhea
Amenorrhea is the absence of a menstrual cycle.
-It is considered primary if a woman has never had a
menstrual cycle
-or secondary if she has had menstrual cycles in the past, but
no longer.
-Amenorrhea exists naturally before puberty (primary
amenorrhea) and after menopause (secondary amenorrhea).
-It also occurs during pregnancy, for a few to several weeks
after delivery of an infant, and may occur during lactation.
-Emotional disturbances and physical stress may also cause
amenorrhea.
-Endocrine disorders, especially involving the ovaries,
pituitary, thyroid, or adrenal glands, can cause amenorrhea,
both primary and secondary.
Conditions of Disease or Injury
Cryptorchidism
Is the failure of one or both testicles to descend
into the scrotum of a male infant.
It is present at birth and is especially common in
premature infants. For most infants born with
this condition, the testes will descend on their
own within the first year of birth.
If descent does not occur, the testes will remain at
a higher temperature than optimal for
spermatogenesis. This may affect sperm quantity
and quality, leading to infertility later in life.
Male sexual function and secondary sexual
characteristics are normal.
Clinical Manifestations
One or both testes will not be palpable in the scrotum at birth.
Diagnostic Tools
-Physical examination is used to diagnose the condition.
-Ultrasound or other imaging techniques may be used.
Complications
• Infertility
• Increased risk of testicular cancer even after surgical repair.
Treatment
• Most cases of cryptorchidism will reverse spontaneously
within 1 year. If spontaneous descent does not occur,
treatment with hCG may stimulate descent.
• If hormonal therapy is ineffective, surgery is required by 2
years of age.
Varicocele
It is an abnormal dilation of a vein in the spermatic cord.
A sudden occurrence of a varicocele in an older man may indicate an
advanced renal tumor.
Clinical Manifestations
• May be asymptomatic or associated with a slight feeling of
discomfort and testicular heaviness.
• Tortuous, dilated veins may be palpable.
Diagnostic Tools
• Physical examination is used to diagnose the condition. Ultrasound
may be used.
Complications
• Poor blood flow to the testes may cause infertility.
Treatment
• A support garment for the testicles is worn to relieve discomfort.
• To maintain fertility, surgical ligation of the vein may be
performed.
Hydrocele
Is the collection of a plasma filtrate in the scrotum,
outside the testes. This filtrate can reduce blood flow
to the testes.
It may be a congenital or traumatioc. A testicular tumor
maybe the cause. May be Idiopathic .
Clinical Manifestations
A hydrocele may be asymptomatic or associated with
palpable or visible swelling and discomfort.
Diagnostic Tools
Physical examination,ultrasound and visual inspection
using a light focused on the testicle may be able to
identify fluid.
Treatment
Identification of the cause and drainage of the fluid.
Benign prostatic hyperplasia (BPH)
Is the non-cancerous enlargement of the prostate
gland. BPH is seen in more than 50% of men older
than 60 years of age.
BPH may cause compression of the urethra as it
passes through the prostate, making urination
difficult, reducing force of the flow of the urine
stream, or causing dribbling of urine to occur.
The cause of BPH is unclear but may be related to an
imbalance between estrogen and testosterone in
the prostate.
Clinical Manifestations
• Increased frequency of urination, with delay in
initiating urination and a reduction in the force
of the urine stream.
• As the condition progresses, the bladder may
not empty completely, causing dribbling or urine
overflow. The time required to void increases.
Diagnostic Tools
• Diagnosis involves a good history and physical
examination coupled with the use of imaging
techniques. Biopsy of the prostate may be
required to rule out neoplasia.
Complications
With advanced BPH, urinary tract obstruction may
occur as urine is unable to pass through the
prostate. Urinary obstruction can lead to urinary
tract infections and, if unrelieved, renal failure.
Treatment
• Mild case is followed in a wait and see manner.
• drugs acting by blocking the action of androgens
on the prostate.
• drugs relaxing the muscles of the bladder and
prostate to improve urine flow. Both types of
medications may be used concurrently.
• transurethral incision of the prostate (TUIP). Lasers
may be used.
• microwave therapy.
• If obstruction to urine flow is severe, transurethral
prostatectomy (TURP) may be required to remove
the enlarged prostate. Complications may include
erectile dysfunction and incontinence.
• A permanent catheter might be placed in patients
unwilling to undergo or unable to tolerate surgery.
• Annual digital rectal examinations and screening for
prostate-specific antigen (PSA) are encouraged to
identify a malignancy that may arise from
hyperplastic cells.
Inflammatory Disorders of the Male Reproductive
Tract
Inflammation anywhere between the testes and the
urethral opening due to a sexually transmitted
disease or a urinary tract infection.
Clinical Manifestations
• Urethritis may present with pain and burning on
urination. A discharge from the penis may be
present.
• Epididymitis may present with acute scrotal or
inguinal pain. Flank pain may be present. The
scrotum may be inflamed and tender on the
affected side.
• Orchitis usually presents acutely with a very high
fever (104آ°F) and swelling and redness of the
testicle and scrotum. The individual appears very ill,
and malaise is obvious.
• Prostatitis from an ascending urinary tract infection
usually presents with painful and frequent
urination. Interrupted or slow urine stream and
nocturia (urination at night) may be present. Fever
and malaise are common. Low back or perineal pain
is common, especially when standing. Digital
examination reveals a very tender and enlarged
prostate.
Diagnostic Tools
-Blood and urine cultures for the identification
of an infectious organism may be required.
Complications
Epididymitis and orchitis may cause infertility,
related to poor testicular blood flow.
Treatment
• Antibiotic therapy.
• Orchitis is treated with bed rest, analgesics for
pain, and elevation of the testicles to increase
venous drainage. Cold compresses may reduce
initial inflammation. If a testicular abscess
occurs, surgical removal of the testicle may be
necessary.
Pelvic Inflammatory Disease (PID)
Is the infectious inflammation of any of the organs of the
upper genital tract in women, including the uterus,
fallopian tubes (salpingitis), or ovaries (oophoritis).
The infectious agent is usually bacterial and is often
acquired during sexual intercourse. A variety of microbial
agents may be implicated, including N. gonorrhoeae, C.
trachomatis, and Escherichia coli.
In severe cases, the entire peritoneal cavity may be
affected.
Clinical Manifestations
• Although occasionally a woman will be asymptomatic,
she usually presents with a high fever and severe bilateral
abdominal pain.
• Bleeding between periods may occur.
• Abdominal pain worsens with intercourse and physical
activity.
Diagnostic Tools
• Palpating or moving the cervix during an internal
pelvic examination is very painful.
• Purulent discharge at the external os may be
apparent on inspection.
• Culture of the cervical discharge may indicate the
infecting microorganism.
• White blood cell count and cell sedimentation rate
are usually elevated.
• Visualization of the inflamed pelvis by laparoscopy,
the insertion of a fiberoptic probe, can be used to
confirm the diagnosis of PID.
Complications
• PID may lead to scarring and adhesions of the
uterus or fallopian tubes, predisposing a
woman to infertility.
• Pelvic adhesions and scarring increase the risk
of a subsequent ectopic pregnancy. In an
ectopic pregnancy, the embryo implants and
grows at a site other than the uterus, usually
the fallopian tube. Rupture of the fallopian
tube may occur, leading to internal
hemorrhage and maternal death.
• Approximately 5% to 10% of women with PID
die, usually from septic shock.
Treatment
• Antibiotic therapy.
• Avoidance of sexual intercourse until the inflammation
has subsided.
• Education on the use of barrier methods of
contraception (condom, diaphragm with foam or jelly)
to prevent future occurrences of sexually transmitted
disease is important.
• Birth control pills may reduce PID by increasing the
production of cervical mucus, but do not replace the
need for a condom.
• The sexual partner(s) of an affected woman should be
evaluated for infection and, if necessary, treated with
antibiotics.
• Appendicitis must be ruled out as the cause of
abdominal pain.
Endometriosis
Endometriosis is the presence of uterine endometrial cells
outside the uterus, anywhere in the pelvic or abdominal
region. The endometrial cells respond to estrogen and
progesterone with proliferation, secretion, and bleeding
during the menstrual cycle. This can cause inflammation and
severe pain. The inflammation may lead to scarring of pelvic
or abdominal organs and infertility.
Clinical Manifestations
• Menstrual cramping and pain, ranging from mild to severe,
before and/or during menstruation is the most common
symptom of endometriosis.
• Changes in bowel movements, either diarrhea or
constipation, may occur around the time of menstruation.
• Pain with intercourse (dyspareunia) or during defecation (if
rectal tissue is involved). The pain is usually worse during
menstruation, but in severe cases pain may be constant.
Diagnostic Tools
Visualization of the peritoneal cavity using
laparoscopic techniques .
Complications
-Infertility is a common (30% to 40%)
complication of endometriosis. Endometriosis
may cause infertility by causing scarring and
obstruction of the fallopian tubes or by
initiating a maintained state of inflammation.
Hormonal disturbances may occur.
Emotional distress, family and marital problems,
especially if infertility is a concern.
Cancer of the Male Reproductive Tract
May develop in the penis, testes, or prostate.
Penile Cancer
Primary cancer of the penis is rare in the United States.
It usually occurs in non-circumcised men, possibly
related to accumulation of thick secretions (smegma)
under the foreskin Secondary penile cancer may occur
from metastasis of bladder, rectal, or prostate cancer.
Testicular Cancer
Testicular cancer is rare, mostly occurring in young men
between the ages of 15 and 35. The cause of testicular
cancer is unknown, but occurs more frequently in men
with a history of cryptorchidism. Trauma and prenatal
exposure to the synthetic estrogen diethylstilbestrol
(DES) may increase risk.
Prostate Cancer
Prostate cancer is the number one cancer among American
males and the second leading cause of death due to cancer in
that population (the first is lung cancer). Prostate cancer is
usually diagnosed in men older than 65 years of age.
Clinical Manifestations
• Penile cancer is characterized by an ulcerative lesion on the
shaft of the penis that may or may not be painful.
• Testicular cancer is characterized by the development of a
mass in the testis, which may become painful as it grows.
Testicular heaviness or aching may occur. Gynecomastia may
develop.
• Prostate cancer may be asymptomatic or associated with
increased frequency and urgency of urination, and a decrease
in the force of the urine stream. Blood may be passed in the
ejaculate, and in advanced disease, back pain may be present.
Diagnostic Tools
• Biopsy of cells of the penis can diagnose and stage penile
cancer.
• Transillumination of the testes, ultrasound, and MRI may
identify a testicular mass and support clinical findings of a
testicular cancer.
• A digital rectal examination may reveal a fixed, firm mass in
the prostate, suggestive of a tumor. The mass is often
painless with irregular borders and results in asymmetry of
the prostate gland. Ultrasound may be used to pinpoint the
location of a prostate tumor. A biopsy of prostate cells taken
via a transurethral resection can confirm the diagnosis of
prostate cancer.
• Prostate-specific antigen (PSA), can be used to identify the
presence of even early-stage prostate cancer.
• Measurement of PSA levels coupled with findings from a
digital exam offer the most sensitive screening results.
Complications
• Untreated, progressive penile cancer has an
extremely high mortality rate (about 90%).
• Testicular cancer may metastasize to the lungs,
lymph nodes, or central nervous system.
• Survival with prostate cancer depends on the
stage at diagnosis. Most men diagnosed with
stage D cancer die within 3 to 5 years.
• Erectile dysfunction and incontinence may
develop as a result of any of the male
reproductive cancers or may develop following
treatment of the cancers.
Cancer of the Female Reproductive Tract
May develop in the vagina, uterus, or ovaries.
• Vaginal Cancer Vaginal cancer usually occurring in women
older than 60 years of age. The vaginal squamous cells are
most often involved. Frequently, the cancer is a secondary
metastasis.
• Uterine Cancer includes:
- Cervical cancer is often a result of a sexually transmitted
disease of the cervix caused by certain strains of the human
papillomavirus (HPV). Cervical cancer is most common in
women who have had multiple sexual partners. The
premalignant changes, called dysplasia, can be identified and
staged during cytologic studies of a cervical smear (the
Papanicolaou smear, or Pap smear).
-Uterine endometrial cancer is the most common female
reproductive cancer and is usually an adenocarcinoma (from
the epithelial cells). Endometrial cancer is related to lifetime
exposure to estrogen and typically presents in
postmenopausal women.
• Ovarian Cancer
Although relatively rare, ovarian cancer causes death more
often than any other female reproductive cancer.
Clinical Manifestations
• Vaginal cancer may be asymptomatic or associated with
bleeding, discharge, or pain.
• Cervical cancer may be asymptomatic or associated with
bleeding after intercourse or spotting between menstrual
periods. A vaginal discharge with odor may be present.
• Endometrial cancer may be asymptomatic or associated
with abnormal bleeding.
• Ovarian cancer is usually asymptomatic until the disease is
advanced. Late symptoms include abdominal swelling and
pain. Gastrointestinal obstruction may cause vomiting,
constipation, or small-volume diarrhea.
Diagnostic Tools
• The Pap smear can identify cervical and
endometrial cancer.
• Direct cytologic sampling of the vagina and
endometrium can diagnose vaginal and
endometrial cancer.
• Ovarian cancer can be identified by use of MRI or
vaginal ultrasound. The ovaries may be palpable.
Surgery is required to stage the disease and identify
metastases. Increased level of an ovarian tumor cell
antigen, CA125, in a symptomatic woman or a
woman with a family history of ovarian or breast
cancer can be an early indication of disease.
Complications
• Death may occur with any of the reproductive cancers.
Survival rates are highest (75 to 95%) with endometrial
cancer and lowest (25 to 30%) with ovarian cancer. Early
detection can improve survival rate significantly, especially
for cervical cancer, which has a survival rate near 100% if
identified while still in situ (before it has spread).
Treatment
• Surgery, with or without chemotherapy. Laser surgery or
cryosurgery (freezing) may be used for vaginal or cervical
cancers. Improved chemotherapy has increased survival rate
for all reproductive cancers, including ovarian cancer.
• Prophylactic bilateral salpingo-oophorectomy, the removal
of both ovaries and fallopian tubes, may be performed on
women at high risk of ovarian cancer who choose this
option.
Breast Cancer
• Breast cancer may be discovered while in situ
(localized), or it may be discovered as a
malignant (spreading) neoplasm. Breast
cancer is usually an adenocarcinoma found in
the milk ducts.
Risk Factors for Breast Cancer
• - A history of the disease in one or more firstdegree relatives (sisters or mother).
• - Lifetime estrogen exposure. Women who
experience early menarche and late
menopause are at increased risk.
• - Lack of or delayed childbearing
• estrogen replacement therapy.
• - A high-fat diet and, in some studies, alcohol
consumption .
• - Hormone replacement therapy (HRT) in
postmenopausal women .
• N.B.,Protection against breast cancer is
possible by consumption of a diet rich in fruits
and vegetables, regular exercise, and weight
control.
Clinical Manifestations
• A painless lump or mass in the breast. Most cancers
occur in the upper outer quadrant of the breast
(50%) or in the center of the breast (20%). The lump
is usually unilateral and fixed (non-mobile), with
irregular borders.
• Retraction of the nipple, nipple discharge, or
puckering of the breast tissue may signal an
underlying tumor.
• Lymph node swelling, either axillary or clavicular,
may indicate metastasis.
Diagnostic Tools
• Breast self-examination (BSE) performed on a regular
(monthly) basis. BSE should be performed by all
women older than 20 years.
• Mammography, the increased use of mammography
has contributed to the fall in death rate due to breast
cancer. Annual or biannual mammography is
recommended for all women older than 40 years of age
and for younger women with a family history of the
disease or other risk factors.
• Biopsy of a suspected lump will confirm the diagnosis.
Determination of tumor size, tumor characteristics, and
examination of surrounding lymph nodes allow for
staging and histologic classification of the tumor.
Staging is from I to IV and is important in determining
treatment and in estimating prognosis
Complications
Widespread metastases may occur. Sites of metastasis
include the brain, lungs, bone, liver, and ovaries.
Treatment
• Surgery, including mastectomy or lumpectomy.
Nodal involvement indicates metastasis of the
tumor and requires more aggressive post-surgical
interventions.
• Adding radiotherapy or chemotherapy in
conjunction with surgery improves survival and
reduces the likelihood of recurrence. These
therapies are based on the presence or absence of
metastasis.
Sexually Transmitted Infection (STI)
may develop in anyone having sexual contact with
multiple partners. Microorganisms capable of
causing an STI include the bacteria Neisseria
gonorrhoeae, responsible for causing gonorrhea,
and Treponema pallidum, responsible for causing
syphilis.
The herpes simplex virus, human papillomavirus
(HPV), hepatitis B virus, and human
immunodeficiency virus (HIV) are also sexually
transmitted. Trichomonas vaginalis is a protozoan
responsible for causing trichomoniasis.
An STI may be passed via semen or vaginal secretions
or by skin-to-skin contact.
Clinical Manifestations
• Gonorrhea may be asymptomatic or may present with
purulent discharge from the urethra or vagina and
burning on urination. Some individuals, including
infants born to infected mothers, may develop
conjunctivitis or pharyngitis.
• Primary syphilis is characterized by the presence of a
painless genital ulcer (chancre) that spontaneously
regresses. Secondary syphilis develops weeks to
months later and is characterized by a temporary skin
rash, typically located on the palms of the hands and
the soles of the feet. Tertiary syphilis may develop
decades after the initial infection and is characterized
by sensory loss, muscle weakness, and heart defects.
• Trichomoniasis may be asymptomatic or may present
with greenish discharge and itching. Pain with
intercourse is common. Men are seldom symptomatic.
Diagnostic Tools
• Smears of vaginal or urethral discharge observed
under the light microscope.
• Vaginal or urethral cultures.
Complications
• Untreated gonorrhea may cause female sterility or
pelvic inflammatory disease. Both men and women
may develop disseminated infection with arthritis,
endocarditis, or conjunctivitis leading to blindness. If
passed to a newborn during birth, blindness may
result.
• Untreated syphilis may cause heart failure and
neurologic deterioration. If passed to a fetus during
pregnancy, fetal death or neonatal infection may
occur.
Treatment
• Because of the prevalence of penicillinresistant gonorrhea, gonorrhea is currently
treated with a single intramuscular dose of
ceftriaxone.
• Syphilis is treated with intramuscular
penicillin.