Male repro
advertisement

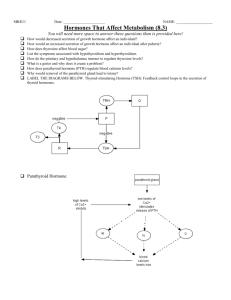
THE MALE REPRODUCTIVE SYSTEM Learning objectives • Outline the steps involved in spermatogenesis • Describe the endocrine regulation of testicular function: the role of the GnRH pulse generator, FSH, LH, testosterone, and inhibin. • Know the general structure of testosterone, and describe its biosynthesis, transport, metabolism, and actions. • List the major target organs and cell types for testosterone and other androgens. • Describe the processes involved in regulation of testosterone secretion Which of the following is a correct statement about the production of human sperm? a. Spermatogonia undergo meiosis b. Spermatogenesis occurs in the epididymis c. Normally, 10 to 20 million sperm are produced daily d. FSH is required e. Complete maturation of spermatozoa occurs in about 1 month OVERALL CONTROL OF ADULT MALE HORMONAL SECRETION Leydig cells • 20% of the adult testis is connective tissue interspersed with Leydig cells. • The function of the Leydig cells is synthesis and secretion of testosterone , the male sex steroid hormone. • Testosterone has both local (paracrine) effects and endocrine effects. Functions of Sertoli Cells • Provide nutrition for the development of germinal cell into spermatozoa and conversion of spermatids into sperms • Production of Androgen-Binding Protein thereby maintain high supply of androgen to the deveolping germ cells • Form Blood-Testes Barrier -prevents entry of toxin • Foetal Sertoli cell produce MIS • Produce Inhibin which inhibits FSH secretion • Synthesize estrogen from testosterone by aromatisation Functions of the Sertoli cells in the seminiferous tubules include a. Secretion of FSH into the tubular lumen b. Secretion of testosterone into the tubular lumen c. Maintenance of the blood-testis barrier d. Synthesis of estrogen after puberty e. Expression of surface LH receptors Spermatogenesis The process of sperm formation Hormonal Factors That Stimulate Spermatogenesis 1. Testosterone 2. Luteinizing hormone 3. Follicle-stimulating hormone 4. Estrogens 5. Growth hormone STRUCTURE OF SEMINIFEROUS TUBULE • The tight junctions between Sertoli cells divide the lumen into a) Basal compartment b) Luminal or adluminal compart. • The spermatogonia are located in the basal compartment • The spermatocytes develop in the luminal compartment within the cytoplasmic folds of the Sertoli cells The Seminiferous Tubules Spermatogenesis divided into three phases: (1) Mitotic divisions of spermatogonia generate the spermatocytes, which are destined to become mature sperm; (2) meiotic divisions of the spermatocytes, which decrease the chromosome number and produce haploid spermatids; (3) spermiogenesis, in which spermatids are transformed into mature sperm through the loss of cytoplasm and the development of flagella SPERMATOGENESIS- 1st STAGE • Spermatogonia in the basal comparment of Seminiferous tubules are called Type A SPERMATOGONIA. • These divide 4 times to form slightly more differentiated cells called Type B SPERMATOGONIA SPERMATOGENESIS- 2nd STAGE • MIGRATION: The Type B spermatogonia migrate centrally across the tight junctions of the Sertoli cells into the adluminal compartment • Having penetrated the barrier they become enfolded in the cytoplasmic processes of Sertoli cells. • Further development occurs in association with the Sertoli cells. SPERMATOGENESIS- 3rd STAGE • FORMATION OF PRIMARY SPERMATOCYTE- For a period averaging 24 hrs the Type B spermatogonium becomes progressively enlarged and modified to form the PRIMARY SPERMATOCYTE • At the end of 24 hrs in the primary spermatocyte the DNA has replicated and each of the 46 chromosomes has 2 chromatids bound together at the centromere SPERMATOGENESIS-4th STAGE • FIRST MEIOTIC DIVISION & FORMATION OF SECONDARY SPERMATOCYTE- The Primary spermatocyte undergoes the first meiotic division • Each pair of chromosome separate so that each secondary spermatocyte has 23 chromosomes • Each of the 23 chromosomes has 2 chromatids SPERMATOGENESIS- 5th STAGE • SECOND MEIOTIC DIVISION & FORMATION OF SPERMATIDS- within 2-3 days a second meiotic division occurs so that 2 spermatids are formed • Each spermatid contains 23 chromosomes having 1 chromatid each • Half of the spermatids have X chromosomes and the other half Y chromosomes • Thus the eventual sperm which fertilizes the ovum provides half the genetic material SPERMATOGENESIS- 6th STAGE • SPERMIOGENESIS: CONVERSION OF SPERMATIDS TO MATURE SPERMATOZOON • The spermatids have characteristics of epitheloid cells • Each spermatid elongates into a sperm composed of a head & a tail. • This change requires that the spermatid is in close association with the Sertoli cell SPERMIOGENESIS • From a single spermatogonium 512 sperms are formed. • The process takes 74 days on average • The two testes of the adult form 120 million sperms each day • STORAGE: A small quantity is stored in the epididymis, but most in the vas deferens & ampulla of the vas deferens Maturation of Sperm in the Epididymis • Maturation of Sperm in the Epididymis -capability of some motility • Storage of Sperm-up to 120 million sperm each day; They can remain stored, maintaining their fertility, for at least a month; After ejaculation, the sperm become fully motile, and they also become capable of fertilizing the ovum, a process called maturation. • Capacitation of the spermatozoa:-uterine and fallopian tube fluids wash away the various inhibitory factors, it lose much of their excess cholesterol, becomes much more permeable to calcium ions. FACTORS AFFECTING SPERMATOGENESIS • TEMPERATURE: Requires a temperature considerably lower than interior of body. The testes are maintained at a temperature of 32 c. They are kept cool by a heat exchange in a counter-current fasion between the spermatic arteries and veins. FACTORS AFFECTING SPERMATOGENESIS • REDUCED SPERMATOGENESIS AND SPERM COUNTEFFECT OF HIGH TEMPERATURE 1) CRYPTORCHIDISM-testes in the abdomen at high temp 2)Tight cloth Binders cause degenration of tubular walls & sterility results 3)Hot baths reduce count 4)Seasonal Variation: Sperm count greater in winter regardless of scrotal temperature FACTORS AFFECTING SPERMATOGENESIS • INFECTION: Mumps causes bilateral orchitis • STRICTURE OF THE GENITAL DUCT causes degeneration of tubular epithelium • GENETIC ABNORMALITIES: Klinefelter’s Syndrome Adults with bilateral cryptorchidism • Elevated temperatures • FSH secretion is elevated, probably as a result of decreased Sertoli cell production of inhibins. • Testosterone secretion by the Leydig cells of cryptorchid testes also tends to be low, and as a result, LH secretion of is elevated. Q. Functions of the Sertoli cells in the seminiferous tubules include a. Secretion of FSH into the tubular lumen b. Secretion of testosterone into the tubular lumen c. Maintenance of the blood-testis barrier d. Synthesis of estrogen after puberty e. Expression of surface LH receptors Testosterone Actions of Androgens on Target Tissues Mediated by Testosterone • Differentiation of epididymis, vas deferens, and seminal vesicles • Deepening of voice • Increased muscle mass • Pubertal growth spurt • Spermatogenesis • Negative feedback on anterior pituitary • Libido • Cessation of pubertal growth spurt (epiphyseal closure) Mediated by Dihydrotestosterone • Differentiation of penis, scrotum, and prostate • Male hair pattern • Male pattern baldness • Sebaceous gland activity • Growth of prostate Age-related changes in LH and testosterone secretion in the normal male 1. Fetal life Normal male development requires the presence of 3 hormones:testosterone,dihydrotestosterone, and the Müllerian inhibiting factor (MIH). 1. (hCG) + LH → Leydig cells → testosterone → Wolffian ducts 2. testosterone → dihydrotestosterone → urogenital sinus & genital organs 3. Sertoli cells → MIH → absence of female internal structures In order for male differentiation to occur during embryonic development, testosterone must be secreted from the testes. What stimulates the secretion of testosterone during embryonic development? A) Luteinizing hormone from the maternal pituitary gland B) Human chorionic gonadotropin C) Inhibin from the corpus luteum D) Gonadotropin-releasing hormone from the embryo’s hypothalamus • Wolffian ducts differentiate into the majority of male internal structures; namely, epididymis, vasa deferentia, and seminal vesicles. • Dihydrotestosterone induces the urogenital sinus and genital tubercle to differentiate into the external scrotum, penis, and prostate gland. 2. Childhood Within a few months after birth, LH and testosterone drop to low levels and remain low until puberty. The cause of this prolonged quiescence of reproductive hormone secretion during childhood is not known. Interestingly, LH secretion remains low in spite of low testosterone. 3. Puberty Near the onset of puberty, the amplitude of the LH pulses becomes greater, driving the mean level of LH higher. Early in puberty, this potentiation of the LH pulses is especially pronounced during sleep. This increased LH stimulates theLeydig cells to again secrete testosterone. 4. Adult During adulthood, LH secretion drives testosterone secretion. Thus, it is not surprising that the relative levels of the two hormones parallel one another. 5. Aging adult Testosterone and inhibin secretions decrease with age. Men in their seventies generally secrete only 60–70% as much testosterone as do men in their twenties. Nevertheless, there is no abrupt decrease in testosterone secretion in men that parallels the relatively abrupt decrease in estrogen secretion that women experience at menopause. The loss of feedback will cause an increase in LH and FSH secretion. In order for male differentiation to occur during embryonic development, testosterone must be secreted from the testes. What stimulates the secretion of testosterone during embryonic development? A) Luteinizing hormone from the maternal pituitary gland B) Human chorionic gonadotropin C) Inhibin from the corpus luteum D) Gonadotropin-releasing hormone from the embryo’s hypothalamus Erection • Erection is caused by dilation of the blood vessels (a parasympathetic response) in the erectile tissue of the penis (the corpora- and ischiocavernous sinuses). • This dilation increases the inflow of blood so much that the penile veins get compressed between the engorged cavernous spaces and the Buck’s and dartos fasciae. • As a result,for a brief period, inflow of blood to the penis exceeds outflow. • Mediators that remove the chronic state of vasoconstriction are probably vasoactive intestinal peptide (VIP) and/or nitric oxide (NO). Acetylcholine may also be involved. Emission • Emission is the movement of semen from the epididymis, vasa deferentia, seminal vesicles, and prostate to the ejaculatory ducts. • The movement is mediated by sympathetic (thoracolumbar) adrenergic transmitters. • Simultaneously with emission, there is also a sympathetic adrenergic-mediated contraction of the internal sphincter of the bladder, which prevents retrograde ejaculation of semen into the bladder. • Destruction of this sphincter by prostatectomy often results in retrograde ejaculation. Ejaculation • Ejaculation is caused by the rhythmic contraction of the bulbospongiosus and the ischiocavernous muscles. • Contraction of these striated muscles that are innervated by somatic motor nerves causes the semen to exit rapidly in the direction of least resistance, i.e., outwardly through the urethra. • Ejaculation ,is mediated by somatic motor efferents. Consequences of deficient testosterone production • During second to third month of gestation -ambiguity in the male genitalia and male pseudohermaphrodism. • third trimester --leads to problems in testicular descent (cryptorchidism) along with micropenis. • Puberty-- to poor secondary sexual development and overall eunuchoid features. • Postpubertal --decreased libido, erectile dysfunction, decrease in facial and body hair growth, low energy, and infertility Hormonal Changes in Specific Altered States Spermatogenesis is regulated by a negative feedback control system in which follicle-stimulating hormone (FSH) stimulates the steps in sperm cell formation. What is the negative feedback signal associated with sperm cell production that inhibits pituitary formation of FSH? A) Testosterone B) Inhibin C) Estrogen D) Luteinizing hormone Estrogen is required for normal reproductive function in the male. Where is the principal site of estrogen synthesis in the male? A) Leydig cells B) Osteoblasts C) Liver cells D) Prostate cells A man suffers from a disease that destroyed only the motor neurons of the spinal cord below the thoracic region. Which aspect of sexual function would not be possible? A) Arousal B) Erection C) Lubrication D) Ejaculation A “birth control” compound for men has been sought for several decades. Which of the following would provide effective sterility? A) Substance that mimics the actions of luteinizing hormone B) Substance that blocks the actions of inhibin C) Substance that blocks the actions of follicle stimulating hormone D) Substance that mimics the actions of gonadotropin releasing hormone A man is taking a number of medications, one of which appears to be interfering with the emission phase of the sexual act. Which of the following medications could cause this problem? A) A medication that prolongs the duration of action of nitric oxide B) A medication that blocks the smooth muscle receptors for nitric oxide C) A medication that increases the release of nitric oxide D) A testosterone-like androgen compound E) An inhibitor of beta-adrenergic nervous system receptors Following ejaculation, arterial blood flow into the corpora cavernosa decreases back to the normal resting level resulting in the flaccid state. What is the best explanation for this decrease in blood flow? A) Systemic arterial pressure decreases due to absence of sexual stimulation B) The level of sympathetic stimulation to the arterioles supplying the corpora cavernosa decreases C) Resistance of the arterioles supplying the corpora cavernosa increases D) Formation of nitric oxide in the endothelial cells of the arterioles supplying the corpora cavernosa is stimulated by the increase in parasympathetic nervous system activity E) Resistance of the venules draining the sinuses of the corpora cavernosa increases Men who take large doses of testosterone-like androgenic steroids for long periods are sterile in the reproductive sense of the word. What is the explanation for this finding? A) High levels of androgens bind to testosterone receptors in the Sertoli cells, resulting in overstimulation of inhibin formation B) Overstimulation of sperm cell production results in the formation of defective sperm cells C) High levels of androgen compounds inhibit the secretion of gonadotropin-releasing hormone by the hypothalamus, resulting in the inhibition of luteinizing hormone and folliclestimulating hormone release by the anterior pituitary D) High levels of androgen compounds produce hypertrophic dysfunction of the prostate gland Which of the following decreases the resistance in the arteries leading to the sinuses of the penis? A) Stimulation of the sympathetic nerves innervating the arteries B) Nitric oxide C) Inhibition of activity of the parasympathetic nerves leading to the arteries D) All of the above