The Cerebellum
advertisement

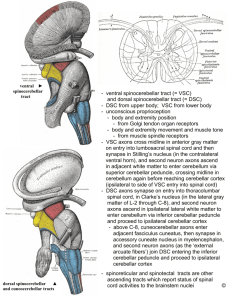
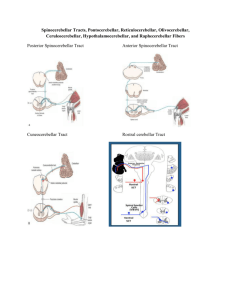
The Cerebellum Clinical Examination Objectives To be knowledgeable about the aspects of the neurological examination pertaining to the cerebellum To understand how to localize lesions within the cerebellum on the basis of clinical findings To develop a framework about the presentation of nervous system illness Cerebellar Examination Midline cerebellar function Cerebellar hemispheric function Clinical localization in the cerebellum For purpose of localization, cerebellum can be viewed as a saggitally-oriented structure containing 3 zones on each side: Midline Intermediate Lateral Midline zone Consists of the anterior and posterior parts of the vermis, fastigial nucleus and associated input and output projections concerned with posture, locomotion, position of head relative to trunk, control of EOM’s Cerebellar signs resulting from midline cerebellar disease disorders of stance/gait, truncal postural disturbances, rotated postures of the head, disturbances of eye movements Intermediate zone Consists of paravermal region of cerebellum and interposed nuclei (emboliform, globose) concerned with control of velocity, force and pattern of muscle activity Clinical disorders related to disease of this zone not clearly delineated Lateral zone cerebellar hemisphere and dentate nucleus on each side concerned with the planning of movement in connection with neurons in the Rolandic region of the cerebral cortex (fine, skilled) Lesions result in abnormalities of skilled voluntary movements: hypotonia, dysarthria, dysmetria, dysdiadochokinesia, excessive rebound, impaired check, kinetic and static tremors, pastpointing Midline Cerebellar Function Observation Posture, head position Gait Eye movements Rhomberg Test Tests of gait- tandem, toe + heel walking, walking backward Hop on each foot Cerebellar Hemispheric Function Finger-to-nose test Rapidly alternating movements Heel-to-shin test Cardinal Features of Cerebellar Dysfunction Hypotonia Ataxia Dysarthria Tremor Ocular Motor Dysfunction Classic signs of cerebellar damage Depending on extent, an individual may have one symptom or a combination In all cases, symptoms from unilateral damage appear on the side ipsilateral to the injury Ascending spinocerebellar pathways are uncrossed and descending corticoopontocerebellar fibers are crossed; thus motor deficits from cerebellar damage are ipsilateral to the lesion whereas motor deficits from damage to motor areas of the cerebral cortex are contralateral to the lesion postural instability delayed initiation and termination of motor actions inability to perform continuous, repetitive movements errors in smoothness and direction of a movement lack of coordingation or synergy of movement, especially complex movements lack of motor plasticity or learning Hypotonia usually accompanies acute hemispheric lesions Interestingly less often seen in chronic lesions Ispilateral to the side of a cerebellar lesion More noticeable in upper limbs and proximal muscles (beware of increased tone with a cerebellar lesion—may reflect compression of brainstem/corticospinal tracts)!! Probably due to fusimotor activity, secondary to cerebellar injury (especially the dentate), with a response to stretch in muscle spindle afferents Ataxia Defective timing of sequential contraction of agonist /antagonist muscles Results in a disturbance in smooth performance of voluntary acts (errors in rate, range, force, duration) Without cerebellar modulation, skilled movements originating in cerebral cortex are inaccurate, poorly controlled May affect limbs, trunk, gait (depends on part of cerebellum involved) usually persists despite visual cues (unlike ataxia due to posterior column disease affecting the spinal cord) Asynergia= lack of synergy of various muscles while performing complex movements ( movements are broken up into isolated, successive parts-- decomposition of movement) Dysmetria= abnormal excursions in movement Dysdiadochokinesia= impaired performance of rapidly alternating movement Past-pointing Excessive rebound when an opposed motion is suddenly released Cerebellar Dysarthria Abnormalities in articulation and prosody (together or independent) “scanning”, “slurring”, “staccato”, “explosive”, “hesitant”, “garbled” May result from a generalized hypotonia (disorder of muscle spindle function) Hemisphere lesions are associated with speech disorders more often than vermal lesions Posterior Fossa Syndrome Acute, bilateral injury to both cerebellar paravermal regions, including the dentate, may lead to transient muteness Seen in up to 20% of posterior fossa tumor resections in children (“cerebellar mutism syndrome”) May last for several months, with severe dysarthria after return of speech Cerebellar affective disorder Impaired executive function, personality, emotional and behavioral changes Can be seen as part of the mutism syndrome Tremor rhythmic, alternating, or oscillatory movements can be a normal exaggeration of movement, a primary disorder, or a symptom of a cerebellar disorder or Parkinson's disease Diagnosis is usually clinical Treatment varies by etiology Tremor- Framework/ Categories Trigger: Resting or action-- includes postural tremors and intention tremors (triggered by a purposeful movement) Cause: Physiologic, essential, parkinsonism, or secondary to drugs or other disorders (including cerebellar disorders) Amplitude of oscillation: Fine or coarse Tremor- General features Resting tremor : maximal at rest, decreases with activity; usually a symptom of Parkinson's disease Postural tremor : maximal with limb in a fixed position against gravity; gradual onset suggests physiologic or essential tremor; acute onset suggests toxic / metabolic disorder Intention tremor : maximal during movement toward a target (fingerto-nose testing) ; suggests a cerebellar disorder but may result from other diseases (MS, Wilson’s) Tremor- Physiologic Physiologic tremor: present normally -- usually so slight that it is noticeable only under certain conditions ; predominantly postural, fine and rapid (8 to 13 Hz) most visible when hands are outstretched Amplitude may be increased (enhanced) by Anxiety Stress Fatigue Metabolic disorders (eg, hyperadrenergic states such as alcohol or drug withdrawal or thyrotoxicosis) Certain drugs (eg, caffeine, other phosphodiesterase inhibitors, β-adrenergic agonists, corticosteroids) Alcohol and other sedatives usually suppress it Tremor- Essential tremor benign hereditary tremor, senile tremor coarse or fine, medium frequency (4 to 8 Hz); min or absent at rest usually bilateral can affect the hands, head, voice tends to increase with aging In 50% of patients, inheritance is autosomal dominant may be enhanced by any factor that enhances physiologic tremor (not always required) Some consider essential tremor a variant of physiologic tremor Tremor- Cerebellar Disease an intention tremor; no effective drug available; physical measures (eg, weighting the affected limbs or teaching patients to brace the proximal limb during activity) sometimes helps Asterixis: not a tremor; muscle tone lapses when wrist extension is attempted, resulting in repetitive, nonrhythmic, non-oscillatory wrist flexion; a sign of chronic renal or liver failure (differentiate from tremor) 3-5 Hz Usually bilateral Can be a sign of hepatic encephalopathy (inability of liver to metabolize ammonia to urea) Patient is usually drowsy or stuporous Oculomotor dysfunction Nystagmus frequently seen in cerebellar disorders Gaze-evoked nystagmus, upbeat nystagmus, rebound nystagmus, opticokinetic nystagmus may all be seen in midline cerebellar lesions Other ocular lesions seen include opsoclonus, skew deviation, ocular bobbing Most of the disorders giving rise to these affect brainstem structures, too: cerebellar role in their onset not well-defined Overall, most “cerebellar” eye signs cannot be localized to specific areas of the cerebellum Features to Examine Gait Ataxia In cerebellar disease, the walk is staggering/lurching/wavering Not benefitted by patient’s view of his surroundings Lesion in mid-cerebellum: movements are in all directions Lesion in lateral cerebellum: staggering/falling are toward the side of the lesion Somewhat steadied by standing or walking on a wide base (ataxia secondary to vestibular disease may appear similar) Gait Gait have patient walk across room under observation Watch for normal posture + coordinated arm movements ask patient to walk heel-to-toe across room, walk on toes to test for plantar flexion weakness, and on heels to test for dorsiflexion weakness Abnormalities in heel to toe walking: ethanol intoxication, weakness, poor position sense, vertigo -- exclude before poor balance is attributed to a cerebellar lesion elderly patients have difficulty with tandem gait (heel to toe walking) -- general neuronal loss impairs combination of position sense, strength, coordination blumentandemgait blumenTipToeGaitandHopping impairedTandemGait.flv CerebGait.flv Testing of Station (equilibratory coordination) Position of Feet Eyes open or closed Ataxia from spinocerebellar disease is less when the patient stands on a broad base (feet widely apart) Cerebellar ataxia is not improved by visual orientation; ataxia from posterior column disease (disordered proprioception) is worsened with the eyes closed Direction of Falling Disease of lateral lobe of cerebellum causes falling to ispilateral side Lesions of midline/vermis cause indiscriminate falling, depending on initial stance of the patient blumenRhombergTest Diadochokinesia Normal coordination includes ability to arrest one motor impulse and substitute the opposite Loss of this = dysdiadochokinesia Characteristic of cerebellar disease Many simple tests for this: Alternating movements (pronate and supinate forearm + hand quickly): in cerebellar disease, movements overshoot, undershoot be irregular or inaccurate Rapidly tap fingers on table Open and close fists Stewart-Holmes rebound sign blumenFineFingerTap.rm blumenRapidlyAltMovements.rm dysdiadochokinesiamovie Dysmetria Finger to nose test With eyes open, have pt partially extend elbow and rapidly bring tip of index finger in a wide arc to tip of his nose In cerebellar disease, the action may have an intention tremor With eyes closed, sense of position in the shoulder and elbow is tested Heel to Shin test Pt places one heel on opposite knee and slides heel down the tibia with foot dorsiflexed Movement should be performed accurately In cerebellar disease, the arc of the movement is jerky/wavering The slide down the shin has an action tremor blumenFingerNoseTest.rm Coordinationwithpuppets.mp4 Cerebellarintentiontremor.mp4 Heelshintest.mp4 Heelshinabnormal.mp4 Checkreflexmovie.mp4 Checkreflexabnorvideo.mp4 Spasticspeech.flv Cerebellar Syndromes In general, precise clinical localization is difficult in the cerebellum Some syndromes can be classified anatomically: Rostral vermis syndrome (anterior lobe) Caudal vermis syndrome (flocculonodular, posterior lobe) Hemispheric syndrome (posterior lobe, variably anterior too) Pancerebellar syndrome Cerebellar Syndromes- rostral vermis Wide-based stance and gait Ataxia of gait, proportionally little ataxia on heel-shin with pt lying down Normal or slightly impaired arm cooordination Infrequent hypotonia, nystagmus, dysarthria alcoholics (restricted form of cerebellar cortical degeneration) Cerebellar Syndromes- caudal vermis Axial dysequilibrium, staggering gait Little or no limb ataxia Sometimes spontaneous nystagmus Rotated postures of head Seen in diseases that damage the flocculonodular lobe (esp medulloblastoma in children)—as tumor grows, a hemispheric cerebellar syndrome may be superimposed Need to also consider other signs of ICP (obstruction of CSF) Cerebellar Syndromes- hemispheric Incoordination of ipsilateral limb movements More noticeable with fine motor skills Incoordination affects most noticeably muscles involved in speech and finger movements Etiologies include infarcts, neoplasms, abscesses Cerebellar Syndromes- pancerebellar Combination of all the other syndromes Bilateral signs of cerebellar dysfunction involving trunk, limbs, cranial musculature Etiologies usually infectious/parainfectious processes, hypoglycemia, paraneoplastic disorders, toxic-metabolic disorders Cerebellum: 4th ventricle The fourth ventricle is ventral to the cerebellum Anatomically and clinically important Mass lesions located in the cerebellum, or swelling of the cerebellum (eg. Edema from an infarct) can compress the 4th ventricle and result in obstructive hydrocephalus My patient: Tamra • 15 yr, R-handed ♀ previously healthy from Woodstock • 3 wk progressive gait unsteadiness, ataxia, dizziness • 6 wk H/A, holocephalic, worse when coughing or sneezing, 5/10, takes Advil • 20 lbs weight loss over 3 wks • admitted to Woodstock General • Dx Mono, D/C home,next day H/A 10/10 HR 76, RR 16, BP 135/76 mmHg, T-35.9 Awake, alert, oriented x3, speech OK Pupils 4mm bilat., brisk, full EOM Nystagmus up & lateral gaze Bilateral papilledema Symetrical facial features N bulk & tone, full power arms & legs 5/5 Reflexes symmetric, Plantars equivocal Difficulty pointing bilat., dysmetric, past pointing, heel to shin good Broad based gait Cerebellar dysarthria video clip Nystagmus video clip Finger to nose- Tamra Heel to shin- Tamra Lower extremity ataxia- Tamra Upper extremity ataxia- Tamra