Eating Disorders in Children and Adolescents
advertisement

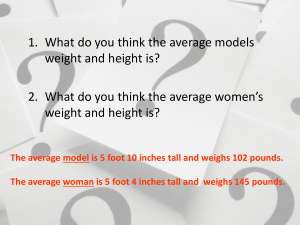
Eating Disorders in Children and Adolescents Gretchen Dubes MSN, RN Learning Objectives Participants will be able to: Define eating disorders delineated in the diagnostic and statistical manual of mental disorders fifth edition (DSM-V) Recognize the pathophysiology, clinical features, assessment processes, and treatment modalities related to adolescents at risk of Anorexia Nervosa and Bulimia Nervosa Identify the supportive role of the nurse in the management of eating disorders which include effective communication strategies to empower patients to take charge and responsibility for their behavior. True or False about Eating Disorders Eating Disorders are complex illness, and successful treatment often requires a multidisciplinary approach from professionals including (psychologists, nutritionist, nurses, pediatricians, psychiatrist and social workers) Tor F Early intervention is important and a predictor for full recovery Tor F More people die from eating disorders than any other psychiatric illness T or F Persons with Anorexia are up to ten times more likely to die as a result of their illness. The most common complications that lead to death are cardiac arrest, electrolyte imbalance and suicide T or F Binge Eating Disorder is the most common ED in the U.S. T or F Purging is a fairly effective way to lose weight T or F It is possible to fully recover from an ED T or F ED’s are primarily about food & weight T or F Case Study-Suzie Anorexia Nervosa Suzie is a Fourteen-year-old who has been losing weight for 8 months. At first her mother thought this was normal teenage dieting as she was trying to lose weight since joining the dance team for high school. She is 5 ft 8 inches and weighs 100 lbs. She has stopped eating with her family because she is becoming a vegetarian and her family eats meat and processed foods. She enjoys baking cookies and desserts for her family but does not eat them. She carries with her a book of calories with a list of foods she is willing to eat. She is on the honor role at school. She is getting straight “A’s” and says she does not settle for anything less. She eats an apple for breakfast, a cup of ramen noodles for lunch and 4 leafs of lettuce with a half a cup of cheese cubes and salad dressing. She snacks on raw carrots and is proud to say her evening snack consists of one oreo cookie. She admits that she eats the same meal everyday. Her daily exercise routine is going for a five mile run but this has decreased in the past few weeks because her energy is diminished. She does sit ups before bed and has been ignoring calls from her friends. When her mother encourages her to eat she becomes defensive and angry shouting she is “ok”, “looks fine” and is eating. Case Study-Sally Bulimia Nervosa Sally is a 16 year old who has been excusing herself from the dinner table after eating. Her mother reports that she has been hearing Sally throw up for quite sometime. She said Sally was overweight since age 8 and since joining soccer she has lost weight. She recently was asked to a dance and believes she needs to lose10 more pounds to look good in a dress. Her mother reports finding various food wrappers in Sally's waste basket from the snacks she purchases every week and has to go shopping more often as a result. In addition, her mother reports that she has found empty packages of Laxatives hidden in her closet. Sally has complained at times to her mother that she feels her heart is racing. She is 5ft 4 inches and weighs 135 lbs. She has callouses on her knuckles and says this is due to her playing soccer. She is often anxious about school and fitting in with her peers. She is often commenting on her weight and thinks she would look better if she weighed 10 pounds lighter. COMMON QUESTIONS This presentation will cover the following questions: 1. What are the risk factors that increase the probability of developing an eating disorder? 2. Which screening questions can be used to detect Eating Disorders? 3. What is the difference between Anorexia Nervosa and Bulimia Nervosa? 4.What are the signs and symptoms of an eating disorder? 5. What are medical complications from an eating disorder? 6. What is the treatment and criteria for hospitalization of an eating disorder? 8. What is the role of the nurse when working with patients suffering from an eating disorder? What are the risk factors that increase the probability of developing an Eating Disorder? Gender More females than males Age Pre adolescent begins to show some signs however, teens and 20’s most likely Location Westernized societies valuing thinness Personality Anorexia-Sensitive, persevering, self-critical features, perfectionistic Bulimia-Unstable mood, impulsivity, and anxious Family History Depression, obesity, eating disorders, substance abuse Interest groups Ballet dancers, gymnasts, wrestlers, models, jockeys Onset of drive for thinness Fifty one percent of girls age 9-10 feel better about themselves if on a diet What are the risk factors that increase the probability of developing an Eating Disorder? Warning signs of high risk behaviors: Reading diet books Evidence of visiting various website about anorexia Sudden decision to become a vegan, or vegetarian Eliminating various food groups Skipping meals Going to the bathroom after eating Purging in the shower Notice large amounts of food missing in the cupboards and refrigerator When to intervene: ACT NOW Fasting and skipping meals Refusing to eat with the family Argumentative when expressing concerns Refusing to eat with family and friends Discovery of laxatives and diet pills Weighing and measuring food Persistent refusal of food Excessive exercise Excessive calorie counting Lock, J & Le Grange, (2015). Help Your Teenager Beat and Eating Disorder. NY: Guilford Press. Pg. 24 Which screening questions can be used to detect Eating Disorders? To better identify eating disorders, the American Academy of Pediatrics (AAP) advocates the routine use of screening questions for all preteen and adolescent patients. Weight History Maximum weight and when? Desired Weight? How does the patient feel about his/her current weight? How frequently does he or she weigh him/herself? When did the patient begin to lose weight? What weight methods have been tried? Diet History Current dietary practices? Ask for specific amounts, food groups, fluid restrictions. Any binges? Frequency, amount? Any purging? Frequency, amount? Abuse of diuretics, laxatives, diet pills? Exercise History-types, frequency, duration Menstrual history-age of menarche, regularity of cycles Physical exam-dizziness, bruising, cold intolerance, vomiting, diarrhea, bloating, epigastric pain, hair loss, dry skin, cold intolerance, weakness, chest pain, palpitations 2.Which screening questions can be used to detect Eating Disorders? Cont. To better identify eating disorders, the American Academy of Pediatric (AAP) advocates the routine use of screening questions for all preteen and adolescent patients. Psychological symptoms/history Adjustment to pubertal development Body image/self esteem Anxiety, depression, obsessive compulsive disorder Past medical history Family history Obesity Eating Disorders Depression Substance Abuse Social History Home-relationships Sexual History-sexual abuse Substance abuse 3.What is the difference between Anorexia and Bulimia? Anorexia Nervosa Eating Disorders- DSM V Criteria for Anorexia Nervosa Anorexia Nervosa is characterized by self starvation and excessive weight loss. DSM V Criteria: 1. LOW WEIGHT--The refusal to maintain a minimally normal weightsignificantly low body weight in the context of age, sex, developmental trajectory, and physical health. 2. FEAR OF WEIGHT GAIN/and or BEHAVIOR TO PREVENT WEIGHT GAIN ---Intense fear of gaining weight or becoming fat, even though underweight. 3. BODY IMAGE DISTURBANCE--Disturbance in the way in which one's body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or denial of the seriousness of the current low body weight. Subtypes Restricting Binge eating/purging Child and Adolescent Psychiatric Nursing Epidemiology and Anorexia Child and Adolescent Psychiatric Nursing Eating Disorders -Epidemiology It is estimated that 8 million Americans have an eating disorder—seven million women and one million men One in 200 American women suffers from anorexia Two to three in 100 American women suffers from bulimia Prevalence of age: 12-25 (NAMI) Rates of diagnosed eating disorders has doubled since 1960’s Eating disorders have the highest mortality rate of any mental illness. The most common behavior that will lead to an eating disorder is dieting. Natalia Zunino, Ph.D, of American Anorexia and Bulimia Association, Inc. 81% of 10 year olds are afraid of being fat. 51% of 9 and 10 year old girls feel better about themselves if they are on a diet. Mellin LM, Irwin CE & Scully S: Journal of the American Dietetic Association. 1992; 92:851-53. The mortality rate among people with anorexia is 5-15%. Mortality is from starvation, electrolyte imbalance, and suicide. Child and Adolescent Psychiatric Nursing Eating Disorders-Anorexia Nervosa Common behaviors associated with Anorexia: Eat only 'safe' foods, usually those low in calories and fat Have odd rituals, such as cutting food into small pieces and excessive chewing Spend more time playing with food than eating it Cook meals for others without eating · Engage in compulsive exercising Dramatic weight loss Dress in layers to hide weight loss Denies that there is a problem Anxiety about gaining weight or being fat Consistent excuses to avoid mealtimes or situations involving food. Preoccupation with weight, food, fat grams, and dieting Denial of hunger Spend less time with family and friends, become more isolated, withdrawn, and secretive Child andAdolescent Psychiatric Nursing Complications due to Anorexia Nervosa Bradycardia, hypotension Arrhythmias Hypokalemia Hypocalcemia Dehydration Amenorrhea Lanugo,dry skin, hair loss Hypoglycemia Hypothermia Edema Constipation Osteoporosis Effects from Starvation Minnesota Starvation Experiment AIM: To Characterize the physical and Mental effects of starvation on healthy men Study: Enrolled 36 males Procedure: For 3 months the men were put on observation and given 3200 kcal diet For 6 months their caloric intake was reduced to semi starvation diet of 1500kcal Exercise was increased to 22 miles of walking/week For remaining 3 months they were place on refeeding plan During the time researchers looked at labs, physical effects and psychological effects Findings—very similar to what we see with Anorexia Nervosa Psychological- apathy, mood swings, irritability, depression, anxiety, obsessions, delusions Physical effects- anemia, cold intolerance, bradycardia, constipation and edema Behavioral effects-perseveration with food, food rituals, hoarding food Kalm, L. , Semba, R. (2005) They Starved So That Others Be Better: Remembering Ancel Keys and the Minnesota Experiments Fed, Journal of Nutrition , 135 (6) : 1347-52 Child and Adolescent Psychiatric Nursing-Biology of Anorexia GeneticsFamily studies have shown that first-degree relatives have a 6 -10 times greater lifetime risk of developing AN than relatives of healthy controls. Bulik, C., Slof-Op’t Landt, M., van Furth, E., & Sullivan, P. (2007). The Genetics of Anorexia Nervosa Annual Review of Nutrition, 27 (1), 263-275 Hypothalamus Key center for regulating hunger. Dysregulation can cause hyposecretion of various hormones: Low-Follicle stimulating hormone and luteinizing hormone are responsible for menstruation- low levels result in amenorrhea. Low-Growth hormone levels-result in stunted growth and osteoporosis. Low –Thyroid stimulating hormone results in decreased energy and coldness. Low- Cortical releasing hormone results in fatigue and depression. Low-Leptin Levels. Leptin is a hormone that appears to trigger the hypothalamus to stimulate appetite, and low levels have been observed in people with anorexia and bulimia. Neurotransmitters Serotonin- Dysregulation of Serotonin (5-HT) pathways. Dopamine- “Increased dopamine activity has been implicated in food repulsion, hyperactivity, weight loss, absence of menstrual cycles and obsessive-compulsive disorder, and is known mediate reward states.” Bulik, C., Slof-Op’t Landt, M., van Furth, E., & Sullivan, P. (2007). The Genetics of Anorexia Nervosa Annual Review of Nutrition, 27 (1), 263-275 The time course and phenomenology of Anorexia Nervosa Walter, K., Fudge, J., and Paulus, M., (2009). The time course and phenomenology of Anorexia Nervosa, Nature Review Neuroscience 10, 573-584 Child and Adolescent Psychiatric Nursing Anorexia Nervosa Psychological Vulnerabilities Cognitive Features-personality traits Misperception of body image Rigid all-or-nothing thinking Obsessive-compulsive thoughts and rituals Perfectionism - Particularly concern for mistakes Difficulty expressing emotions Control Issues = Over Control Puberty- Avoidance of maturity Brain development Child and Adolescent Psychiatric Nursing Anorexia Sociocultural Factors 3. What is the difference between Anorexia and Bulimia? Bulimia Nervosa Eating Disorders- DSM V Criteria for Bulimia Nervosa Bulimia Nervosa is characterized by binge eating WITH compensatory behaviors. DSM V Criteria: Bulimia Nervosa 1. BINGE EATING-Recurrent episodes of binge eating characterized by BOTH of the following: Eating in a discrete amount of time (within a 2 hour period) large amounts of food. Sense of lack of control over eating during an episode. 2. COMPENSATORY BEHAVIOR--Recurrent inappropriate compensatory behavior in order to prevent weight gain (purging, over exercising, abuse of laxatives etc..). 3. BINGE PURGE CYCLE 1X WEEK FOR 3 MONTHS---The binge eating and compensatory behaviors both occur, on average, at least once a week for three months. Self-evaluation is unduly influenced by body shape and weight. . Child and Adolescent Psychiatric Nursing Epidemiology and Bulimia Nervosa Bulimia Nervosa About 4-20% in Females and 0.1-0.2 % in males Bulimia appears during late teens to mid 20’s Some estimates of up to 40% college women have tried purging Katie Couric “I wrestled with bulimia all through college.” Child and Adolescent Psychiatric Nursing Bulimia Nervosa Biological Factors Serotonin- Binging behavior is consistent with reduced serotonin function. Psychological Factors Control Issues = Out of control Hiding Self-esteem Sexual Abuse Family Factors Parents described as neglectful and rejecting. Some research has shown a higher than normal rate of substance abuse in families of bulimics, especially alcohol abuse. Learned response to stress. Some bulimics report that their parents used "comfort food" to manage stress and negative emotions. (See next Slide) Child and Adolescent Psychiatric Nursing Bulimia Nervosa Person experiences stress and tension leads to loss of control “Vicious Cycle of Bulimia” Child and Adolescent Psychiatric Nursing Eating Disorders-Bulimia Nervosa Common Behaviors associated with Bulimia: Recurrent episodes of uncontrollable binge eating Become very secretive about food, spend a lot of time thinking about and planning the next binge Takes repeated trips to the bathroom, particularly after eating Steal food or hoard it in strange places Engage in compulsive exercising Abuse Laxatives and diuretics Anxiety escalates before eating Child and Adolescent Psychiatric Nursing Eating Disorders-Bulimia Nervosa Complications due to Bulimia Nervosa Bradycardia Arrythmias Hypokalemia Hypocalcemia Dehydration Irregular menses Hoarseness Dental caries Enlarged parotid glands Tears in esophagus Hyponatremia Constipation Calluses on the back of hands and knuckles from self-induced vomiting Adolescent Psychiatric Nursing Eating Disorders-Recovery Rates Anorexia: among adolescents, 50–70% recover. 20% partially recover. 10–20% develop chronic anorexia (Steinhausen, 2002). Bulimia: in a six-year treatment study, 60% had a good outcome. 29% had an intermediate outcome. 10% had a poor outcome (Fichter and Quadflieg 1997). What is the treatment and criteria for hospitalization of an eating disorder? Treatment Evidenced Based Treatment Modalities Eating Disorders-Anorexia And Bulimia Treatment for Eating Disorders-Outpatient, Day Treatment (Partial Program), Inpatient Hospitalization Nutrition therapy=Education Cognitive Behavioral Therapy Family TherapyMaudsley Family Based Treatment-Evidenced Based Approach for adolescents living at home with parents Three Stages: Stage I-Establish healthy eating patterns; Stage II- Return control of eating and weight management adolescent; Stage III -Address family and normal developmental issues. Pharmacologic Treatment: What criteria are used for hospitalization of an eating disorder? The American Psychiatric Association (APA) Practice Guidelines According to the APA guidelines: “The decision about whether a patient should be hospitalized on a psychiatric versus a general medical or adolescent/pediatric unit should be made based on the patient’s general medical and psychiatric status, the skills and abilities of local psychiatric and general medical staff, and the availability of suitable programs to care for the patient’s general medical and psychiatric problems.” Suggested Guidelines for Inpatient Treatment Admission Criteria for Hospitalization-medical and psychiatric hospital <75% Ideal Body Weight, Unstable Pulse<50, May be dehydrated Hospitalize. Here it is essential for nursing staff to be included in the plan of action, to take a supportive role and to not bargain with the patient or keep information from the treatment team. Restore nutrition through food trays planned by dietician with expectation of completion. NG backup if patient unable or unwilling to take in prescribed nutrition. Provide calories through 3 meals and 3 snacks over the course of a day. Calories will be determined by REGISTERED DIETICIAN. MONITOR CLOSELY FOR REFEEDING SYNDROME Supervision-the patient should be closely monitored during and for one hour after eating to provide support and ensure compliance. Educate-educate the patient about eating disorder and relaxation techniques to use before and after eating. Educate the patient about nutrition and provide support as needed. ROME, E. S., S. AMMERMAN, D. S. ROSEN, R. J. KELLER, J. LOCK,K. A. MAMMEL, J. O’TOOLE, J. M. REES, M. J. SANDERS, S. M.SAWYER, M. SCHNEIDER, E. SIGEL, and T. J. SILBER. Children and adolescents with eating disorders: the state of the art. Pediatrics 111:e98–e108, 2003. Suggested Guidelines by American Academy of Pediatrics REMEMBER- “Hospitalization needs to be long enough to enable the patient to stop losing weight, establish a gaining weight trend, normalize vital signs and laboratory studies, and be able to self select and eat independently to continue to gain weight as and outpatient.” ROME, E. S., S. AMMERMAN, D. S. ROSEN, R. J. KELLER, J. LOCK,K. A. MAMMEL, J. O’TOOLE, J. M. REES, M. J. SANDERS, S. M.SAWYER, M. SCHNEIDER, E. SIGEL, and T. J. SILBER. Children and adolescents with eating disorders: the state of the art. Pediatrics 111:e98–e108, 2003. Goals for Treatment of Eating Disorders Goals of treatment: Restore patients to a healthy weight-Clinical consensus suggests that realistic targets are 2–3 lb/week for hospitalized patients. Treat physical complications Enhance patients’ motivation to cooperate in the restoration of healthy eating patterns and participate in treatment Provide education regarding healthy nutrition and eating patterns Help patients reassess and change core dysfunctional cognitions, attitudes, motives, conflicts, and feelings related to the eating disorder Treat associated psychiatric conditions, including deficits in mood and impulse regulation and self-esteem and behavioral problems Enlist family support and provide family counseling and therapy where appropriate What is the role of the nurse when working with patients suffering from an eating disorder? 1. Conduct a health history including screening questions. 2. IDENTIFY child or adolescent with risk factors or risky behaviors 3. Based upon information gathered from assessment Collaborate with the health care team—questions to ask? Is this an Eating Disorder? Is the patient medically and psychiatrically stable? Does this patient meet criteria for inpatient admission? 4. Nursing Interventions –therapeutic communication-Do’s and don’ts when communicating with patients with Eating Disorder Providing support , empathy and education Collaborate with health care team to provide resources and link with health care professionals to monitor and stop progression of eating disorder. Nursing Assessment of Children and Adolescents with Eating Disorders Assessment focuses on the following Data: Interview-from family and patient Screening questions Records from pediatrician Developmental History School functioning Family relationships Mental Status Physical Exam Nutritional intake—Breakfast-lunch-dinner Labs-CBC, UA, Chem 7 with Mg and Phos etc.. EKG Vital Signs Eating Disorders- Nursing Interventions Develop a therapeutic relationship- provide empathy and nonjudgmental attitude Try to gain insight into the patients strengths and weaknesses and how the patient uses their disorder to communicate. Monitor the patients physical and mental status Observe vital signs, EKG and electrolytes, BUN, Creatinine, CBC TSH Monitor activity level Weigh daily with back to scale Lock bathroom door 1 hour after eating Do not allow patients to bargain with food; set limits The dietician will determine number of calories required to provide adequate nutrition and realistic weight gain. Encourage verbalization of thoughts and feelings—Do not focus on food and eating-The real issues have little to do with food or eating pattern. Explore the correlation between use of food and dealing with feelings. Focus on CONTROL issues that have precipitated these behaviors Explain benefits of compliance with routine and consequences for noncompliance Teach patient to recognize signs of increasing anxiety and ways to intervene Monitor for refeeding syndrome—see next slide Eating Disorders- Nursing Interventions Refeeding Syndrome occurs when the malnourished body has inadequate nutrients for rebuilding. Typically, patients are at greatest risk from 3 days post initiation of refeeding and then for 2 weeks or until stable. Deficiencies in potassium, magnesium, and phosphate can cause death and need to be monitored and prevented. Other symptoms of refeeding syndromeIncreased Pulse Increased Respiratory Rate Increased Peripheral Edema Decreased gastric motility Dyspnea Delirium Coma Seizures See handout treatment guidelines from Medical Management of Eating Disorders by C. Laird Birmingham and Pierre Beumont (2004). Approaching a patient you are concerned about and is suffering from Eating Disorder Shifting your attitude—a new approach If you suspect ED is present or developing: Approach the person with concerns using observations-Remember the patient may not be in agreement and will try to persuade you to think as they are. Their cognitive distortions may interfere with reality. Don’t expect insight into illness. Be prepared for denial and anger and don’t take it personally Use “I” language vs. “You” language Get family involved in the conversation—Maintain united front with family and staff. Avoid “splitting”. Provide support for meals Encourage therapy to treat disordered eating and distorted thinking Provide information—the National Eating Disorder Association (NEDA) Parent tool kit Adolescent Psychiatric Nursing Eating Disorders- Nursing Interventions During meal times Light hearted conversation Provide distractions from the food Avoid comments related to food, calories, body Avoid being the food police Discretely monitor for behaviors during mealtime Observe for signs of resistance Talking about food/calories/body Not eating in a timely manner, stalling Cutting/shredding food into small pieces; Moving food around the plate Hiding food in napkins, pockets or “Accidentally” dropping food on floor Overconsumption of fluids >2 beverages Bargaining for different foods Slide adapted from ALLISON REED, RD-Forest View-Eating Disorder Program Coordinator Therapeutic Communication Eating Disorders- Nursing Interventions Direct comments to avoid “You look so much better” “You are looking much healthier” “I’m glad you’re starting to put on some weight” “I can see your bones, eat a cheeseburger” “I’m glad to see you eating again” “We need to bulk you up” “Have you lost more weight?” “You don’t look like you have an eating disorder” “You are so thin” “You look good today” “Just eat something” Slide adapted from ALLISON REED, RD-Forest View-Eating Disorder Program Coordinator Therapeutic Communication Eating Disorders- Nursing Interventions Eating disorders tend to be made up of irrational thoughts, behaviors and beliefs. It’s challenging for support people to know what to say, and what not to say. Many well intentioned comments can come across as very triggering Slide adapted from ALLISON REED, RD-Forest View-Eating Disorder Program Coordinator Therapeutic Communication Eating Disorders- Nursing Interventions DO: Do consider the person’s feelings/opinions and show that you value his/her input Do express love and support Do try to understand Do take time to listen Do communicate honestly, with support and understanding Do let the person have control over their own issues Do accept your limitations Do encourage the person to seek help Do gently encourage proper eating Do provide positive reinforcement Slide adapted from ALLISON REED, RD-Forest View-Eating Disorder Program Coordinator Therapeutic Communication Eating Disorders- Nursing Interventions Don’t: Don’t try to force the person to eat Don’t blame the individual or get angry Don’t comment on weight or appearance Don’t be afraid to talk about the problem Don’t make the person feel bad or guilty Don’t make threats or use punishment Don’t be impatient and expect instant recovery Don’t purchase food solely to accommodate the one struggling with an ED. Slide adapted from ALLISON REED, RD-Forest View-Eating Disorder Program Coordinator Link to support groups Eating Disorders-Anorexia And Bulimia Support Groups Forest View Hospital, 1055 Medical Park Drive SE. Use the Partial Hospitalization Program entrance on the South side of the building. Group meets in the community room 7-8:15pm 2nd and 4th Mondays of each month. On the 4th Monday, Gail Hall, LMSW, owner and therapist at CTED (Comprehensive Treatment for Eating Disorders) attends and leads a separate forum for family members and support individuals. Yellow House at Cavalry Church, 707 East Beltline NE 2nd Monday of the month, 7-8:30pm This guided discussion group for women 18+ offers a spiritual perspective on eating and body image issues as well as prayer and support utilizing the FINDING balance curriculum. The group is led by Jennifer Lane, who is fully recovered and free from an eating disorder. Slide adapted from ALLISON REED, RD-Forest View-Eating Disorder Program Coordinator Questions and Comments?