PBIS Implementation Strategies

Implementation of PBIS in a Children’s Residential
Mental Health Treatment Program
Lisa Davis, LMFT, Clinical Director
Eleanor Castillo, Ph.D., Director, Outcomes & Quality Assurance
3 rd International Conference on Positive Behavioral Supports
Reno, NV
March 2006
1
Overview
I. Description a. EMQ and Residential Services b. Population Served
II. Context for redesign a. Overview of change process and changes implemented b. Detail of PBIS implementation
III. Review data and case examples
IV. Lessons learned a. Facilitative factors b. Challenges
V. Next steps
2
EMQ Mission and Vision
To work with children and their families to transform their lives, build emotional, social and familial well-being and to transform the systems that serve them.
EMQ will lead the nation in service excellence, innovation and social policy improvement for children and families.
3
EMQ Children & Family Services
Services in 18 California counties
Wraparound
Residential Treatment
Therapeutic Behavioral
Services
School Based Mental
Health Services
Mobile Crisis
Intervention
Outpatient Treatment
Chemical/Alcohol
Dependency Education &
Prevention
In Home Family
Treatment
Sexual Abuse Treatment
Foster Care-Professional
Parent, ITFC
Family Partnership
Institute
4
Core Philosophy
Consistent with the Child and Adolescent Service
System Program Principles (CASSP)
• Strengths Based
• Family Centered
• Community Based
• Culturally Competent
• Individualized
• Natural Supports
• Team Based/Collaborative
• Persistence
• Outcome Based
5
Agency-wide # of Youth
(FY2004-2005)
Crisis
Wraparound
FFA
Outpatient
Sexual Abuse Treatment
System of Care
Addiction Prevention Service
School Based
Residential
Matrix
Total
150
150
129
102
778
503
471
227
85
46
2,641
6
EMQ Referral Sources
(FY2004-2005)
DFCS
Education
Self/Family
EMQ
1019
409
329
321
JPD
County MH
179
174
Medical Facility 94
Other 213
N = 2738
37%
15%
12%
12%
6%
6%
3%
9%
7
Residential Referral Sources
(FY2004-2005)
DFCS
EMQ
JPD
County MH
Medical
Facility
Other
50
7
9
13
3
3
59%
15%
4%
8%
11%
4%
8
Logic Model
EMQ Residential Program Logic Model
03/13/06
Youth, Family, and System
Conditions
1.1 Target Population
Youth (ages 6-17) who are unable to
maintain safely at home or in the
community due to severe mental
health needs that interfere with
the youth and family functioning
1.2 Referral Sources
Department of Child and Family
Services, County Mental Health,
Juvenile Probation, Kaiser and EMQ
UPLIFT Program
1.3 Authority
RCL Level 14 licensed by State
Department of Social Services
1.4 Target Services
Intensive 24/7 mental health treatment
Program
Components
2.1
Universal
2.2
Targeted
Key Activities and
Processes
3.1
3.1a. 10-step Domain Planning
3.1b. PBIS Structured Milieu
3.1c. MH Treatment Plan
3.1d. Caregiver Education Support
3.1e. Comprehensive and Ongoing Assessment
3.1f. Experiential Therapy
3.1g. Rehabilitation Groups
3.1h. Psychotherapy Services; ind, family & group
3.1i. Medical/Nursing Assessment and Follow-Up
3.1j. Psychiatric Assessment and Follow Up
3.1k. Case Management
3.1l. Home Visits and Family Involvement
3.1m. Academic Support
3.1n. Therapeutic Recreation/Community Activities
3.1o. 24/7 On-call Support
3.1p. Discharge Planning and Coordination
3.2
3.2a. CBT (individual/group)
3.2b. Specialized Group Therapy
3.2c. Intensive Family Therapy
3.2d. Functional Behavior Assessments
3.2e. Individualized PBIS Behavior Plans
3.2f. Specialized Visitation Plans
3.2g. Aftercare Transition Services
3.2h. Family Finding
3.2i. Safety Planning
Expected Outcomes
Youth will:
Demonstrate improved functioning
Demonstrate increased satisfaction in various domains of youth’s life
Develop portable skills
Have increased # of connections w/ family and significant others
Report more involvement in community activities
Families will:
Report a reduction in stress
Have more effective strategies & skills to meet youth’s needs
Maintain youth in the home and community
Report being actively involved in youth’s treatment
2.3
Intensive
3.3
3.3a. TBS Services
3.3b. Crisis Management
3.3c. Medication
Program draws from the following theories: Positive Behavioral Intervention and Supports, Bronfrenbrenner,
Love & Logic Parent Training Program, Family Finding Model of Catholic Community Resources, and systems theory
9
Residential Service Goals
Establish permanency for youth in a safe, loving and supportive family.
Provide 24-7 structure, supervision and therapeutic intervention.
Stabilize acute behaviors and improve daily functioning.
10
Residential Services Description
4 RCL (Rate Classification Level) 14 cottages
Two units for children ages 6-12 years
Two units for youth ages 12-18 years
3 are co-ed and 1 is all male
Each unit has capacity to serve up to 10 children
11
Staff Resources
Clinical Director
Clinical Program Manager
Clinician/Case Manager
Residential Cottage Supervisor
Milieu Activity Therapist
Psychiatrist
Educational Resources
Recreational Therapist
Registered Nurse
12
Array of Services
Comprehensive assessment of all life domains
Family Therapy
Individual Therapy
Intensive case management and linkage to community activities
Nursing services
Psychiatric Assessment and
Treatment
Psychoeducational and psychotherapeutic groups
Academic support
Family Finding
Family Partner Services
Medical/Dental Assessment and
Linkage
Recreational, Music and Art
Therapy
Therapeutic milieu based on
PBIS principles
13
Cottage Structure
Schedule of activities
Points system
Level system
Incentive and behavior management system
Team meetings
Day treatment
Mental health model
14
Overview
I. Description a. EMQ and Residential Services b. Population Served
II. Context for redesign a. Overview of change process and changes implemented b. Detail of PBIS implementation
III. Review data and case examples
IV. Lessons learned a. Facilitative factors b. Challenges
V. Next steps
15
Residential Targeted Population
Children with Severe Emotional Disturbances
Youth who are experiencing:
Maladaptive response to trauma
Severe impairment in capacity to function in their daily activities
Psychotic features or dangerousness to self or others
Need repetitive, consistent interventions that structure their environments and teach adaptive behaviors
Many with co-morbid disorders (primarily mood disorders and behavioral disorders)
Need 24/7 supervision, support, and observation under clinical direction of a therapist and psychiatrist, to maintain safety
16
Youth Characteristics
Gender Male
Female
Language English
Spanish
Other
Ethnicity African American
Asian/Pacific Islander
Caucasian
Latin American
Native American
Other
Residential
59%
41%
95%
3%
3%
13%
8%
30%
46%
1%
3%
17
Youth Characteristics
(cont.)
Age at
Program
Entry
% of Outof-Home
Placements
CAFAS at
Program
Entry
6 to 12 Years Old
13 to 18 Years Old
Less than 3
3 or More
Not Applicable
Marked (100 to 130)
Severe 140 and
Higher)
Residential
46%
54%
16%
79%
5%
31%
69%
18
Youth Characteristics
(cont.)
History of
Abuse
Physical No
Yes
Sexual No
Yes
Drug/Alcohol No
Yes
Residential
36%
64%
60%
40%
23%
77%
19
Overview
I. Description a. EMQ and Residential Services b. Population served
II. Context for redesign a. Overview of change process and changes implemented b. Detail of PBIS implementation
III. Review data and case examples
IV. Lessons learned a. Facilitative factors b. Challenges
V. Next steps
20
Context for Change
Concern sited nationally regarding poor outcomes for residential services
Concern regarding the negative effects of congregate care for certain youth
High cost of services, particularly in context of diminishing resources
Effectiveness of community based services, which highlights the question of the need for residential services
Focus on the right for permanency and the result foster care has had on severing family connections
The need to re-conceptualize residential in thinking about services as a 24/7 clinical intervention versus an emphasis on a living environment
21
Why Re-design Residential Services?
To implement evidence based services including PBIS,
Trauma Focused CBT, and Parent Management Training
To utilize residential services as an intervention, not as a placement
To achieve improved outcomes
Increase youth and family connections
Develop sustainable community supports
Ensure permanency for youth in a loving, supportive family
To ensure consistent implementation of a strength based, needs driven, family centered, individualized and culturally relevant philosophy in all aspects of care
To partner with families and ensure family involvement in all aspects of care
Maintain families connection with their community and increase natural supports
22
SAMHSA’S Residential Best
Practice Principles
Strengths imbedded in ALL aspects of care
Focus on resiliency and developmental needs
Families are full partners
Focus on permanency planning
Truly individualized and culturally competent
Focus on the need to be successful in community
Full integration of residential services into the community and continuum of services
Comprehensive developmentally appropriate assessments
(psychosocial, trauma, physiological, cognitive, language, safety, etc.)
Use of specific evidence-based interventions
Respectful, strength-based relationships and interactions are a cornerstone
23
The Role of Residential Services
In partnership with the family and youth, meet unmet needs with the goal of returning youth to the home and community as soon as possible.
Short-term stabilization when all other resources have been unable to maintain safety.
To provide short-term intensive services to sustain family stability and maintain permanency. The level of intensity of service supports accelerated healing and change.
Multidisciplinary assessment to understand the youth and family’s needs.
Frequent psychiatric intervention and observation to stabilize functioning and meet needs so that community resources can be effectively utilized.
24
Change Process
Work team approach with inclusive decision making
Established a leadership team
Well developed communication plan
Use of change methodology-Implementation
Management Associates (IMA)
Business Case for Action
Charter
Use of quality improvement techniques
3 phase change process:
Gathering data/information
Implementation
Evaluation
25
Redesign Work Teams
Phase I Work Plan
Residential Redesign Team
Completed 5/1/05
Questionnaire
Work Team
Customer Survey
Work Team
Focus Groups with Current Post
DC Youth/Family
Population
Analysis Work
Team
Integration Team
Core Leadership
Team
Charter
Development
Best Practice
Conference Work
Team
Larry North Marina Boliaris
LEAD
Michelle
McNerney
LEAD
Jeff Reichenthal
LEAD
Jason Glover
CO-LEAD
Lisa Davis
LEAD
Lisa Davis
Andrew Pane
Larry North
Lisa Davis Andrew Pane Lanetta Smyth Larry North Jason Glover
MAT Focus
Group
Simon Purse
LEAD
Lanetta Smyth
Nancy Minister Charlotte
Hendricks
Marina Boliaris Lanetta Smyth Lisa Wilson Laura Palmer Lisa Wilson Andrew Pane
Simon Purse
Amalia Ferriera
Jeff Reichenthal Roger Bundlie Jennifer Miller Lisa Wilson Susannah Folcik
Charity Packer Charity Packer
Jennifer Miller
Jennifer Pitt Lisa Davis Jason Glover
Cheryl Sanwo
Chris Mullins
Janet Atkins
DFCS
Al Miranen
DFCS
John Crowder
Chris Mullins John Crowder
Michelle
McNerney
Connie Wright Simon Purse
Cheryl Sanwo Nancy Minister
Connie Wright
Jennifer Miller
Charlotte
Hendricks
Literature Search
E.B.P. Work
Team
Lisa Davis
CO-LEAD
Andrew Pane
CO-LEAD
Laura Palmer
Lanetta Smyth ?
Linda Owens
Judy Palen
Veronica Padilla
Michelle
McNerney
Family Inclusion
Work Team
Simon Purse
LEAD
Jennifer M. Miller
Tom Burgis
John Crowder
Michelle
McNerney
Sherrie Tullsen
Charity Packer
Jennifer Best
Craig Wolfe?
Jessica Weiler
Carly Mitchell
CO-LEAD
26
Redesign Work Teams
Residential Redesign
Implementation Work Plan
Phase II
In Progress
Program
Procedures
Andrew Pane
LEAD
Tom Burgis
Connie Wright
Laura Palmer
Charity Packer
Visitation Work
Team
Chris Mullins
LEAD
Roger Bundlie
Nancy Minister
Lanetta Smyth
Connie Wright
Susannah Folik
Family Event
Planning Team
EBP Work Team
Connie Wright
CO-LEAD
Andrew Pane
CO-LEAD
Teresa Barstow
Bobby Dehn
Lisa Davis
LEAD
Andrew Pane
Laura Palmer
Michelle
McNerney
Monica Martin
F.S/Sequoia
Penn East MAT
Tom Burgis
Linda Owens
Veronica Padilla
Eleanor Castillo
Larry North
Jon Oakes
Carl Sumi
Family Finding
Lisa Davis
LEAD
Chris Mullins
Andrew Pane
Connie Wright
M.H. Pilot
Jason Glover
LEAD
Lisa Davis
Integration Team
Core Leadership
Team Charter
Development
Publish/Present
Redesign
Craig Wolfe
LEAD
Lisa Davis
Lisa Davis
LEAD
Larry North
Lisa Davis
CO-LEAD
Eleanor Castillo
CO-LEAD
Lisa Wilson Veronica Padilla Laura Palmer
Andrew Pane
Tanisha Clarke
Laura Champion
Jean Riney-
Niewiadomski
Deb Beaucox
Jason Glover
Michelle
McNerney
Carl Sumi
Lanetta Smyth
John Crowder
Tanisha Clarke
Lisa Wilson
Laura Palmer
Lanetta Smyth
Jennifer Wilson
Rodney Tabares
Monica Martin
Jessica Weiler
Sherrie Tullsen
Kevin Campbell Laura Palmer
Clinician
27
Phases of Change Process
Phase 1 - Data Gathering
Focus groups with families and children
Staff questionnaires
Customer questionnaires
Reviewed 7 years of internal data
Literature review of Evidence-Based Practices
Benchmarking other residential programs
Attendance at “Best Practices” conferences
28
Phases of Change Process
Phase 2 – Implementation
Implemented PBIS
Family Finding
Family Inclusion Practices and Procedures
Community Based Practices
Switch to Mental Health Model vs. Day TX.
Developed Transitional Services
29
Why PBIS?
Evidence in schools that approach creates pro social positive environments
Alignment with agency philosophy
Goodness of fit: congruent with behavioral approach already utilized
Focus on increasing quality of life, achieving broad goals and supporting portable skills
Use of a proactive and educative approach to support elimination of “control based” interventions including restraints
Eber, Sugai, Smith, & Scott (2002); Scott & Eber (2003 a & b)
30
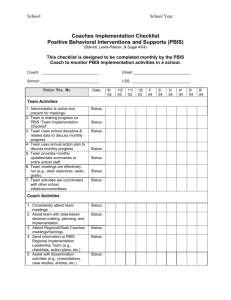
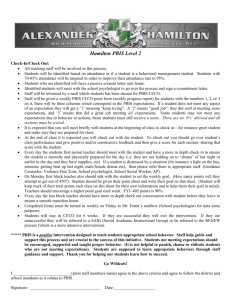
PBIS Implementation Strategies
PBIS Overview Training for all staff
Consultant Role:
Observed each cottage to understand current operations, staff skills and
knowledge and population
Provided 3 8-hour trainings for all 60 staff
on development of Functional Behavioral
Assessment and Behavior Support Plans
Between trainings staff practiced skills and brought plans back to each training
31
PBIS Implementation Strategies
Training Model
Booster
Training
Consultation
Staff – FBA, BSP
CPMs
Directors
Exposure
32
PBIS Implementation Strategies
PBIS implementation work team created to discuss operational issues (director, managers, program sups, clinicians, MATs and consultant)
Meet two times a month
Developed “Support team”
Consultant/Trainer provides bi-monthly consultation
Membership includes 4 line staff and 2 therapists
Consultant attended team meetings to discuss plans and provided booster trainings
33
PBIS Implementation Strategies
Management Infrastructure
Develop behavior and cottage management system
Reviewed past point and level system, develop new systems based on values matrix
Establish core values/expectations and settings
Develop universal rules
Provide consultation and problem solve barriers
Development of internal training capacity to sustain PBIS
Develop and adapt all program policies and procedures to reflect PBIS implementation
34
PBIS Implementation
Currently entering daily point sheets into SPSS database to analyze trends
Goal is to revise point and level system using newly developed behavioral goals and expectations and have point and level system support the positive values and expectations
Ultimate goal is to have staff enter daily point totals into the agencies electronic record system for each child at the end of each shift
This will enable real time analyses of data trends within each cottage
35
PBIS Implementation
Core values/expectations chosen
Respect, Safety, Responsibility and Cooperation.
Process of choosing settings
Examples are meal times, community time, family visits, hygiene, chores etc.
Translation from school based to residential based different
Settings activity based vs. physical environment
Accommodate 24-7 vs. school hours
Focus on daily living skills, participation in treatment program etc.
36
Overview
I. Description a. EMQ and Residential Services b. Population served
II. Context for redesign a. Overview of change process and changes implemented b. Detail of PBIS implementation
III. Review data and case examples
IV. Lessons learned a. Facilitative factors b. Challenges
V. Next steps
37
Living Situation at Exit
100%
90%
80%
70%
60%
50%
40%
30%
20%
10%
0%
Pre-
EBP
Post-
EBP
Willow
Pre-
EBP
Post-
EBP
Sequoia
Pre-
EBP
Post-
EBP
Penn East
Pre-
EBP
Post-
EBP
Ruth Mallery
Other
Shelter/Homeless
More Restrictive
Residential
Foster Family
Home
38
Reason for Discharge
100%
90%
80%
70%
60%
50%
40%
30%
20%
10%
0%
Pr e-
EBP
Post -
EBP
Willow
Pr e-
EBP
Post -
EBP
Sequoia
Pr e-
EBP
Post -
EBP
Penn East
Pr e-
EBP
Post -
EBP
Rut h Maller y
Missing Inf or mat ion
Neut r al
Tx Goals Not Met
Planned Disc har ge
39
Average Number of Runaways Per Month
5
4
3
2
1
0
1
0
Willow
1 1 1
0 0 0
Sequoia Penn East Ruth Mallery
Pre-EBP Post-EBP
40
Average Number of Restraints Per Month
14
12
10
8
6
4
2
0
0
1
Willow
12
9
8
6
3
0
Sequoia Penn East Ruth Mallery
Pre-EBP Post-EBP
41
Average Number of Assaultive Behaviors
Per Month
20
16
15
11
10 8
7
5
5 3
2
0
0
Willow Sequoia Penn East Ruth Mallery
Pre-EBP Post-EBP
42
Case Presentation 1: “Roger”
Male, 13 years old
Caucasian
Referred from The Dept of Social Services as a result of failed foster home placement and lower group home level
Primary Diagnosis-
ADHD
Co-morbid diagnosesODD, Tourette’s
43
Case Presentation 1: “Roger”
Broad goals : Making and keeping friends
Strengths : Friendly, cares about others
Challenges : Low cognitive ability, no strong familial relationships
Target behaviors : hitting, kicking, throwing playground equipment
Baseline frequency- 6-10 times a day during activities
Types of data collected
Interviews with the Milieu Activities Therapist
Observations conducted by several staff
Record reviews
44
Case Presentation 1: “Roger”
Antecedents
: When in a physical activity involving peers, specifically when there is down time or during a transition and he has easy access to sports equipment
Consequences
: Usually staff attention for misbehavior and peer agitation
Hypothesized function
: Self-stimulation or adult attention
45
Case Presentation 1: “Roger”
Proactive strategies
Keep tactile object in pocket to use during transition times
Engage in energy release prior to transitions
Educative strategies
Describe what happens when he throws an object without others awareness
Teach how to use equipment appropriately
Functional/consequence-based strategies
Earn sticker as a reward for positive behaviors;
Get more staff attention at bedtime if he uses equipment safely
46
Case Presentation 1: “Roger”
Outcomes of Plan :
Behavior has reduced to 1-2 times daily during activities
Increased more self esteem and enjoys physical activities more often
Improved peer interactions during physical activity
Other positive effects
Made one friend
Seeks positive attention from staff more frequently
47
Case Presentation 2: “Charles”
Male, 9 years old
Latino American
Referred from the Dept of Social Services
Primary Diagnosis
: ODD
Co-Morbid Diagnoses: Depressive D/O NOS,
Anxiety D/O NOS, Cognitive Disorder NOS,
ADHD
48
Case Presentation 2: “Charles”
Broad goals : Decrease aggressive behaviors and make friends.
Strengths : Intelligent, cute, good sense of humor, strong sense of loyalty.
Challenges : Disrespectful of others feelings, rude and defiant.
Target behaviors : Telling others what to do
Baseline frequency- 15-20 times a day
Types of data collected
Interviews with the Milieu Activities Therapist, therapist, Foster
Parent and Social Worker.
Observations conducted by several staff using ABC scatter plots.
Record reviews
49
Case Presentation 2: “Charles”
Antecedents
: Interacting with peers and when others are getting negative attention.
Consequences
: Looses points, staff engage with him/set limits and give time outs.
Hypothesized function
: Attention seeking
50
Case Presentation 2: “Charles”
Proactive strategies
Attention cards
Staff check ins particularly during transitions
Educative strategies
Taught him positive ways to get staff and peer attention
Role played how to talk with others, how disengage, what tone of voice to use and the difference between telling and asking.
Functional/consequence-based strategies
Received stickers every time he walked away or didn’t do target behavior
Received a certificate with stickers
Earned one on one time with staff
51
Case Presentation 2: “Charles”
Baseline frequency for target behavior 15-20 times a day.
After implementation target behavior reduced to
2-3 times a day.
Other positive effects
Improved school behaviors and earned student of the month
Made a friend
Number of restraints reduced from 1-3 times per week to 1 time a month.
52
Case Presentation 3: “Jason”
Male, 11 years old
Latino American
Referred from the Dept of Mental Health
Primary Diagnosis
: Dysthymic Disorder
Co-Morbid Disorders: ODD, Asperger, Rett
53
Case Presentation 3: “Jason”
Broad goals : Decrease social anxiety and improve social skills and interactions
Strengths : Smart, quick to learn, good verbal skills
Challenges : Can be egocentric, rude to others
Target behaviors : Manipulating, arguing with staff, not following staff directions
Baseline frequency- 2-3 times every 15 minutes
Types of data collected
Interviews with parents and youth
Observations conducted by several staff
Record reviews
54
Case Presentation 3: “Jason”
Antecedents
: Attention is on other youth, when Jason is in unfamiliar situations
Consequences:
After interrupting or arguing Jason received attention from staff (usually in the form of reprimands and redirections)
Hypothesized function
: Attention from staff
55
Case Presentation 3: “Jason”
Proactive strategies
Predicted for Jason that he would use nice words
Reminded him of the incentives
Educative strategies
Taught positive ways to get attention
Taught him to ask for what he wants directly
Taught skills to be appreciative
Functional/consequence-based strategies
Praise when he is engaging in positive behavior
Gets one puzzle piece per 15 minutes if not engaging in target behaviors (arguing, not following directions) and for demonstrating replacement skills. After 32 pieces, he gets
Jamba juice
56
Case Presentation 3: “Jason”
Time 2 frequency
: Target behavior reduced to 2-3 times per day
Other positive effects
Family visits: More successful family visits, less rude, increased safety
School: Increased participation
Made a friend in the unit
57
Overview
I. Description a. EMQ and Residential Services b. Population served
II. Context for redesign a. Overview of change process and b. changes implemented
Detail of PBIS implementation
III. Review data and case examples
IV. Lessons learned a. Facilitative factors b. Challenges
V. Next steps
58
Facilitative Factors
Agency and PBIS philosophy alignment
Outcome and evaluations department
Data management practices
Use of change methodology and quality improvement techniques
Trainer/consultant thoroughly learned operations, built relationship with staff
On going support from consultant
Sponsorship and resources from management
59
Facilitative Factors
Structuring discussions of BSP in team meetings
Development of a “Support Team” and an
Operations work team
Key staffs’ skill sets and enthusiasm
Resource binders and books
Clearly delegating tasks to specific people with timelines
Being open to concerns and seeing resistance as helping to inform the change process
60
Facilitative Factors
Building PBIS job expectations into staff evaluations
Acknowledging staff and celebrating successes
Developing Program Procedures to support implementation
Using electronic record to gather and report data
61
Challenges
Implementing significant change while caring for children 24-7
Deciding what practices to discontinue to make room for new practices
Development of a sustainability plan
Considering multi-systemic needs and regulations, particularly in terms of documentation
Maintaining focus and prioritizing PBIS implementation with multiple other demands
62
Challenges
Learning curve on how to utilize data to inform practice
Establishing consistency and accountability across three shifts, 20 staff and registry
Overcoming agency culture “flavor of the day”
63
Overview
I. Description a. EMQ and Residential Services b. Population served
II. Context for redesign a. Overview of change process and changes implemented b. Detail of PBIS implementation
III. Review data and case examples
IV. Lessons learned a. Facilitative factors b. Challenges
V. Next steps
64
NEXT STEPS
Continue to evaluate outcomes
Continue evaluation of universal interventions and individual FBAs/BSP
Develop a system to incorporate documentation of BSP into current documentation
Continue development of sustainability plan
Start implementation in other EMQ programs
65
REFERENCES
Scott, T.M. & Eber, L. (2003). Functional
Assessment and Wraparound as Systemic School
Processes: Primary, Secondary, and Tertiary
Systems Examples. Journal of Positive Behavior
Interventions, Vol 5 (3), pp 131-143.
Eber, L., Sugai, G., Smith, AC.R., & Scott, T.M.
(2002). Wraparound and Positive Behavioral
Interventions and Supports in the Schools.
Journal of Emotional and Behavioral Disorders,
Vol 10 (3), pp 171-180.
66
CONTACT INFORMATION
Lisa Davis, LMFT, Clinical Director
Email: ldavis@emq.org
Eleanor Castillo, Ph.D., Outcomes & Quality
Assurance Director
Email: ecastillo@emq.org
67