Eating
Disorders
Psychological
and Clinical Perspectives: Assessment,
diagnosis, treatment and explanations.
A critical look- what has been ignored?
Devinder Rana BSc (Hons) Psychology LM40507 Psychopathology and Abnormal Psychology
Aims
By the end of the session you will be able to
do the following:
Describe how the DSM-IV-TR defines and
distinguishes different eating disorders.
Describe and compare how the biological,
psychological and sociocultural perspectives
explain the aetiology of eating disorders.
Analyse the different treatments and
perspectives and their legal and ethical
implications.
Eating Disorders
1. Anorexia Nervosa
2. Bulimia Nervosa
3. Eating Disorder Not Otherwise Specified
(EDNOS) Binge-eating disorder (proposed
diagnosis requiring further study).
Anorexia Nervosa
Criteria DSM-IV-TR
Refusal to maintain a body weight that is normal
for the person’s age and height (i.e., a reduction
of body weight to about 85% of what would be
normally expected).
Intense fear of gaining weight or becoming fat,
even though underweight.
Distorted perception of body shape and size.
Absence of at least three consecutive menstrual
cycles.
Source: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (2000). American
Psychiatric Association.
In-text citation: APA (2000)
Sub-types (APA, 2000).
2 sub-types –
how they
maintain weight
Binge/eating,
purging type
Out of control eating
Food amounts far greater then
average consumption
Followed by efforts to purge
Restrictive Type
Calorie in-take controlled
Limit food in-take
Avoid eating in the presence of other people
Eat slowly, cut and play with food
(Beaumont, 2002)
In Context DSM-VI-TR (2000)
Criteria
A 5’11 adult weighing
11 stone (70 kilos)
falls into the OK
category.
A deviation of 15%
results in the
individual now
weighing just over 9
stone and is
subsequently classed
as anorexic.
Epidemiology
80-90% of suffers are female with typical
age onset between 14-18 years old (Pike,
1998).
Weight control remains a long-term issue.
Links with Obsessive Compulsive Disorder
Occur in young children
Occur in boys
Ballet dancers (Gelsey Kirkland)
and gymnasts (Christy Henrich)
Characteristics of Anorexia
Anorexic’s develop eating habits typical of
bulimia nervosa (e.g. maintenance of ‘normal’
weight through abnormal eating habits).
Socio-economic and academic achievement
link.
Pre-occupation with food- thoughts of eating,
preparation of food or watching others eat.
High ‘calorie consumption’ behaviours e.g. gym,
running or swimming.
Young, European American Women .
Distorted body image
Over estimation
of body
proportion and
distorted body
image (Gupta &
Johnson, 2000).
Link with
depression,
anxiety and OCD.
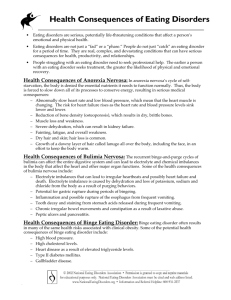
Effects of Anorexia
Amenorrhea (lack of menstruation).
Immune infections
High/low blood pressure
Cracked Skin
Brittle hair and bones
Cardiotoxicity (heart damage)
Consequences
Mortality rate is 12x higher than the
mortality rate for females aged 15 to 24 in
the general population (Sullivan et al
1995).
Death results from:
Physiological consequences from starvation
Intentional suicidal behaviour
Historical Account and Definition
Anorexic nervosa means:
“ lack of appetite induced by
nervousness”.
(Butcher et al, 2007).
Lack of appetite is not the real problem.
“Self-starvation, resulting in a minimal
weight for one's age and height or
dangerously unhealthy weight”.
Hudson et al (2006).
Greek
An: without
Orexis: a desire for
“ without desire for food”
Nevid et al (2008).
Central to anorexia nervosa
Fear of gaining weight
or becoming fat
Refusal to maintain
even a minimal low
body weight.
Historical Accounts
Accounts in early religious literature
(Vandereycken, 2002).
First medical account published in 1689 Richard
Morton.
18 year old girl and 16 year old boy- described
as having a:
“nervous consumption that
caused wasting of body tissue”.
1873 Sir William Gull in London & Charles
Lasegue in Paris independently describe the
clinical syndrome and receive its current name.
Gull (1888)
Described a 14 year old girl:
“Without apparent cause, to evidence a
repugnance to food, and soon afterwards
declined to take whatever, except half a
cup of tea or coffee”.
Problems with the diagnostic tool:
DSM-IV-TR
Women who continue to menstruate but
meet all the other diagnostic criteria for
anorexia nervosa are just as ill as those
who have amenorrhea (Cachelin & Maher,
1998; Garfinkel, 2002).
For men, the equivalent of the
menstruation criterion is diminished sexual
appetite and lowered testosterone levels
(Beaumont, 2002).
Bulimia Nervosa
Criteria DSM-IV-TR
Recurrent episodes of binge eating.
binges in a fixed period of time, food far greater than normal circumstances.
Lack of control and unable to stop.
Recurrent and inappropriate efforts to
compensate for the effects of binge eating.
self induced vomiting
laxatives
excessive exercise
thyroid medication
Self-evaluation is excessively influenced by
weight and body shape.
Source: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (2000). American
Characteristics
Food is eaten rapidly, secretively, without pleasure in
binges where in excess of 5000 calories can be
consumed (2x the recommended daily male intake).
Bulimics demonstrate a fear of weight gain and consider
themselves to be heavier than they actually are
(McKenzie et al 1993)
Approximately 80-90% of individuals will vomit following
a period of binging, one third adopt laxative use and
others constantly exercise (Anderson et al, 2001).
Long-term problems include digestive issues,
dehydration, damage to stomach lining and damage to
the teeth.
Fairburn & Beglin (1994) estimate prevalence between
0.5-1%.
Anorexia Vs. Bulimia
Anorexia
Bulimia
Weight loss not driven by
desire to appear feminine.
High self-control
Social concept of femininity
drives behaviour
Impulsive and emotional
instability
Body weight significantly
(>15%) below age/height
Less likely to have been
overweight
Underweight (severe)
Weight fluctuation (remains
relatively close to norms)
More likely to have been
overweight
Normal weight (slightly
overweight)
Less likely to abuse
drugs/alcohol
More likely to abuse
drugs/alcohol
Bulimia and Purging anorexia
nervosa
Meets the criteria for binging/purging, also
meets the criteria for anorexia nervosa,
anorexia nervosa will be diagnosed.
Common anxiety with fear of being fat.
2 types
Bulimia
Purging (80%)
Non-purging
Vomiting
Fast/exercise
Use of laxatives
Explanations
Complex Interaction
Psychological
Biological
Socio-cultural
family
Individual
Biological Factors
Genetics
Genetics
Runs in families (Bulik & Tozzi, 2004)
Risk of anorexia nervosa for relatives of people
with anorexia nervosa was 11.4x more greater.
Bulimia 3.7X higher, than relatives with healthy
controls. (Strober et al, 2000).
Relatives of patients with eating disorders are
more likely to suffer from other problems,
especially mood disorders (Mangweth et al
2003).
However, eating disorders are not densely
clustered as are mood disorders and
schizophrenia.
Twin studies
Anorexia nervosa and
bulimia nervosa are
hereditable disorders
(Bulik & Tozzi, 2004;
Fairburn & Harrison,
2003).
Genes
Chromosome 1 linked to
the susceptibility to the
restrictive type of
anorexia (Grice et al,
2002).
Bulimia (purging) linked
to chromosome 10
(Bulik et al, 2003).
Eating disorders linked to
chromosomes involved
Genes responsible for
serotonin: low serotonin
level (Kaye et al., 2005)
Brain: Hypothalamus and GLP-1
Regulates bodily functions
Lateral hypothalamus: produces
hunger when activated
Ventromedial Hypothalamus:
reduce hunger when activated
Each part electrically stimulated in
animals they decrease/increase
eating behaviour (Duggan &
Booth, 1986)
Glucagon-like peptide-1 (GLP-1)
natural appetite suppressant.
Inject rats they will not eat even
after a 24hr fast
Block GLP-1 in the hypothalamusdouble food intake (Turton et al.,
1996).
Weight Set Point Theory
LH, VMH, GLP-1, work together
comprise a weight thermostat
Weight set point theory (WSP)
(Hallschmid et al., 2004).
Genetic inheritance and early eating
patterns determine WSP.
Weight falls below the WSP, hunger
increases and metabolic rate
decrease.
Diet and fall below WSP, hypothalamic
activity produces a preoccupation with
food and desire to binge.
Trigger bodily changes- harder to lose
weight however little is eaten (Spalter
et al., 1993)
Restricting-type anorexia: shut down
their inner thermostat and control their
eating completely.
Binge-purge pattern: battle spirals
(Pinel et al., 2000)
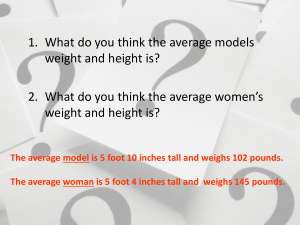
The average American
woman is 5’4” and 140
pounds.
The average American
model is 5’11” and 117
pounds.
Societal
Pressures
Current Western standards of female attractiveness have contributed
to increases in eating disorders (Jambor, 2001).
Decline Miss America Pageant, average decline of 0.28 pound per
year (Garner et al., 1980).
Fashion models, actors, dancers, certain athletes: more prone to
eating disorders (Couturier & Lock, 2006).
20% of gymnast surveyed had an eating disorder (Johnson, 1995).
White upper socioeconomic expressed more concerns about thinness
(Mrgo, 985)
Recent years increased in all classes and minority groups (Germer,
2005).
Double standard has made women more inclined to diet and more
prone (Cole & Daniel, 2005)
Cruel jokes targeted as obesity are standard in the media (Gilbert et
al., 2005)
Deep rooted (Grilo, 2006)
Parents more likely to rate a picture of a chubby child as less friendly,
energetic, intelligent and desirable.
61% of secondary school girls are dieting (Hill, 2006)
Battle of Brittan's
Timeline
1639 - The Three Graces; Pieter Pauwel Rubens
1887 - Pierre Auguste Renoir, The Bathers
1920 - Thin, short haired flapper
1950 - Monroe (Size 14/16)
1960 - Twiggy Lawson (Aka the beginning of the end.) This was the first
time in history that an under weight woman became the standard for the
ideal body image.
1988 - Cosmopolitan
2002 - Harper’s Bazaar
Modern day Fashion Model
Family Environment
Important role in the development of eating
disorders (Reich, 2005)
½ families: emphasise thinness, physical
appearance and dieting.
Mothers diet frequently and be perfectionist
(Woodside et al., 2002).
Abnormal interactions and communication (Reich,
2005)
Family systems theory: dysfunctional family,
person with eating disorder is representative of a
larger problem (Rowa et al., 2001)
Enmeshed family pattern (Minuchin et al., 1978):
over involved with in each other’s affairs and over
concerned with details of each other’s lives.
Teenagers push for independence which threaten
the harmony of the family.
Family may subtly force the child to take on a sick
role- develop eating disorder or other illness.
Enables the family to maintain its appearance of
harmony.
Some case studies support this view (Wilson et
al., 2003)
Systematic research fails to support this link .
Ego Deficiencies and Cognitive
Disturbances
Bruch built on psychodynamic and cognitive notions.
Disturbed mother-child interactions lead to serious ego deficiencies
in the child (poor sense of control and independence) serve
cognitive disturbances (Bruch, 2001).
Effective parents: attend to their child’s biological and emotional
needs
Ineffective parents: fail to attend to needs, misinterpreting i.e., being
hungry rather than seeing the actual condition- grow up confused.
Not being control of their behaviour, not rely on internal signs, not
self-reliant instead during adolescence when looking for
independence seek control with weight and body image.
Pearlman (2005) eating disorder parents define children needs
rather than the child.
Bruch (1973) interviewed 51 mothers of a child with an eating
disorder, many recalled how they never allowed the child to feel
hungry and anticipated their child’s needs.
Perceive internal cues inaccurately (Bydlowski et al., 2005)
Anxious or upset- think they are hungry so eat
Worry how others view them, seek approval, be conforming and feel
lack of control over their lives (Button & Warren, 2001).
When do people seek junk food? When they feel bad.
Lyman (1982)
boredom
depression
anxiety
nurition
junk food
love
happiness
self-confidence
0
20
40
60
80
100
Mood Disorders
Eating disorders, especially bulimia nervosa,
experience symptoms of depression (Perinea et al,
2005)
Eating disorder also qualify for a clinical diagnosis of
major depressive disorder (Duncan et al., 2005)
Close relatives of people with eating disorders seem to
have a higher rate of mood disorders than do close
relatives of people without such disorders (Moorhead
et al., 2003).
Eating disorders, especially bulimia nervosa have low
activity of serotonin, similar to serotonin abnormalities
found in depressed people.
People with eating disorders are helped by some of
the same antidepressant drugs that reduce
depression.
Treatments for Anorexia
Nervosa
How is proper weight and normal
eating restored?
Past in hospitals, today in outpatient settings (Vitousek &
Gray, 2006)
Life-threatening cases: force tube and intravenous
feedings on a patient who refuses to eat (Tyre, 2005)
Can result in distrust in the patient (Robb et al., 2002).
Weight restoration approaches: clinicians use rewards
whenever patients eat properly or gain weight (Tacon &
Caldera, 2001)
– Combination of supportive nursing care, nutritional counselling &
high calorie diet (no more than 2,500 calories a day). Herzog, et
al., 2004).
– Help them to recognise that the weight gain is under control and
will not lead to obesity..
– Gain the necessary weight in 8-12 weeks.
How
are
lasting
changes
achieved
Overcome their underlying
psychological problems in order to
achieve lasting improvement
Therapy and education: individual,
group and family approaches
(Hechler et al., 2005).
Recognise need for independence
and teach them more appropriate
ways to exercise control (Dare &
Crowther, 1995).
Trust their internal sensations and
feelings (Kaplan & Garfinkel,
1999)
Correcting disturbed cognitions:
change attitudes about eating and
weight (McFarlane et al., 2005).
Identify, challenge and change
maladaptive assumptions (Lask et
al., 2000)
Changing family interactions: meet
with the family, point out
troublesome family patterns,
separate feelings and needs from
those of other family members
Aftermath of Anorexia Nervosa
Use of combined approaches has improved the outlook but the road to
recovery is difficult (Fairburn, 2005)
Positive
Weight is often restored once treatment begins (McDermott & Jaffa, 2005)
83% improvement, several years later, 33% fully recovered and 50%
partially improved (Herzog et al., 1999)
Menstruate again (Fombonne, 1995)
Death rates are decreasing (Neumarker, 1997).
Negative
20% remain seriously troubled for years (Haliburn, 2005)
When recovery occurs it is not always permanent
1/3 triggered again by new stresses (Fennig et al., 2002)
½ continue to experience emotional problems- depression, social anxiety,
obsessive which are common when reaching normal weight (Steinhausen,
2002)
Treatment Bulimia Nervosa
Treatments
Eating disorder clinics
Eliminate binge-purge patterns and establish god eating patterns,
Education as much as therapy (Davis et al 1997)
Individual insight therapy: cognitive-recognise and change
maladaptive attitudes (Cooper, 2006)
Not respond then use interpersonal psychotherapy- improve
interpersonal functioning.
Psychodynamic therapy- limited support.
Behavioural therapy: supplement with cognitive
Dairies- note sensations of fullness etc
Exposure and response prevention
Anti-depressant medication: Prozac help 40%
Group therapy: self-help groups- helpful to 75% when combined with
individual sight therapy
Aftermath
Treated successfully, relapse is a common
problem triggered by new life stresses.
1/3 treated relapse 6months later
(Olmsted et al., 1994)
Former patients less depressed then time
of diagnosis (Halmi, 1995)
Depends on history, length and frequency
of vomiting.
Karen Carpenter: 1970’s
Reading Seminar
Should individuals with Anorexia
Nervosa Have the Right to Refuse LifeSustaining Treatment?
Yes: Heather Draper from “Anorexia Nervosa
and Respecting a Refusal of Life-Prolonging
Therapy: A Limited Justification”, Bioethics (April
1, 2000)
No: J.L. Werth, Jr., Kimberly S. Wright, Rita J.
Archambault, and Rebekah J. Bardash, from
“When Does the ‘Duty to Protect’ Apply with a
Client Who Has Anorexia Nervosa?” The
Counselling Psychologist (July, 2003).
Petrie, T., Greenleaf, C., Reel, J., & Carter, J. (2008,
October). Prevalence of eating disorders and disordered
eating behaviors among male collegiate athletes.
Psychology of Men & Masculinity, 9(4), 267-277.
Retrieved January 22, 2009, doi:10.1037/a0013178
Tibon, S., & Rothschild, L. (2009, January). Dissociative
states in eating disorders: An empirical Rorschach study.
Psychoanalytic Psychology, 26(1), 69-82. Retrieved
January 22, 2009, doi:10.1037/a0014675
Hepworth, J., & Griffin, C. (1995). Conflicting opinions?
'Anorexia nervosa,' medicine and feminism. Feminism
and discourse: Psychological perspectives (pp. 68-85).
Thousand Oaks, CA US: Sage Publications, Inc.
Retrieved January 22, 2009, from PsycINFO database.
Wu, K. (2008, December). Eating
disorders and obsessive-compulsive
disorder: A dimensional approach to
purported relations. Journal of Anxiety
Disorders, 22(8), 1412-1420. Retrieved
January 22, 2009,
doi:10.1016/j.janxdis.2008.02.003
Reading
Nevid, J.S., Rathus, S.A., & Greene, B.
(2008). Abnormal Psychology In A
Changing World. (7th ed.). Pearson
Prentice Hall: London. Chapter 10, pp.
330-357.
End