Chapter 5: The Skeletal System
advertisement

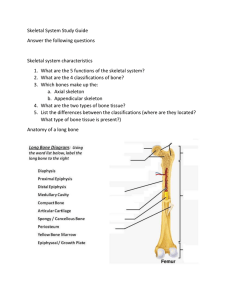
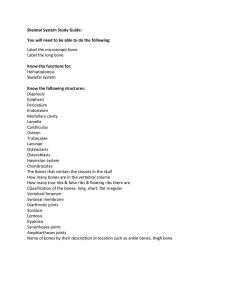
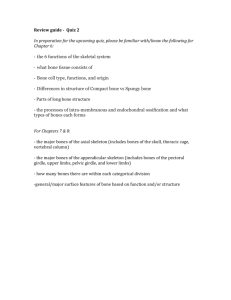
Chapter 5: The Skeletal System Anatomy & Physiology Ms. Halbohm The Skeleton: The Skeleton is divided into two subdivisions: 1) The axial skeleton, the bones that form the longitudinal axis of the body 2) The appendicular skeleton, the bones of the limbs and girdles In addition to bones, the skeletal system includes joints, cartilages, and ligaments.( fibrous cords that bind the bones together at joints.) Functions of Bones: 1) Support: bones form the internal framework that supports and anchors all soft organs. 2) Protection: Bones protect soft body organs. The skull for example protects your brain. 3) Movement: Skeletal muscles are attached to bones by tendons and use the bones as levers to move the body and its parts. 4) Storage: Fat is stored in the internal cavities of bones. Bones also store minerals, the most important being calcium and phosphorus, although others are also stored. 5) Blood cell formation: Blood cell formation, or hematopoiesis, occurs within the narrow cavities of certain bones. Classification of Bones: There are 206 bones in the adult skeleton and two basic types of osseous, or bone tissue: 1) Compact bone is dense and looks smooth and homogenous. 2) Spongy bone is composed of small needlelike pieces of bone and lots of open space. Classification of bones: 3. Long bones: are typically longer than they are wide. Long bones are mostly compact bones. All the bones of the limbs, except the wrist and ankle bones, are long bones. 4. Short bones: are generally cube-shaped and contain mostly spongy bone. The bones of the wrist and ankle are short bones. 5. Flat bones: are thin, flattened, and usually curved. They have two layers of compact bone sandwiching a layer of spongy bone between them. Most bones of the skull, the ribs, and the sternum (breastbone) are flat bones. 6. Irregular bones are bones that do not fit into any other category. The vertebrae and the hip bones are examples of irregular bones. Structure of the long bone: 1. The Diaphysis, or shaft, makes up most of the bone’s length and is composed of compact bone. 2. The periosteum is a fibrous connective tissue membrane that covers and protects the diaphysis. 3. Hundreds of connective tissue fibers, called perforating, or Sharpey’s fibers, secure the periosteum to the underlying bone. 4. The epiphyses are the ends of the long bone, each consisting of a thin layer of compact bone enclosing an area filled with spongy bone. Structure of Long Bone: 5. Articular cartilage covers the surface of the epiphyses. Articular cartilage is glassy, hyaline cartilage which provides a smooth, slippery surface that decreases friction at joint surfaces. 6. The epiphyseal line is a thing line of bony tissue in adult bones spanning the epiphysis that looks different from the bone in that area. 7. The epiphyseal line is a remnant of the epiphyseal plate (a flat plate of hyaline cartilage) seen in young, growing bone. 8. In adults, the cavity of the shaft is primarily a storage are for fat (adipose) tissue and is called yellow marrow or medullary, cavity. Structure of Long Bone: 9. In infants, the cavity of the shaft forms red blood cells and red marrow is found there. 10. Bones are covered with bone markings that reveal where muscles, tendons, and ligaments were attached and where blood vessels and nerves passed. 11. There are two categories of bone markings: 1) Projections, or processes which grow out from the bone surface 2) depressions, or cavities, which are indentations in the bone. Microscopic Anatomy: 1. Osteocytes are mature bone cells and are found in tiny cavities within the matrix called lacunae. 2. The lacunae are arranged in concentric circles called lamellae around central Haversian canals. 3. Each complex consisting of central canal and matrix rings is called an osteon, or Haversian system. Microscopic anatomy: 4. Tiny canals, canaliculi, radiate outward from the central canals to all lacunae. Because of this elaborate network of canals, bone cells are well nourished in spite of the hardness of the matrix, and bone injuries heal quickly and well. 5. The communication pathway from the outside of the bone to its interior (and the central canals) is completed by perforating (Volkmann’s) canals, which run into the compact bone at right angles to the shaft. Bone formation, Growth, and Remodeling: 1) Ossification is the process of bone formation and involves two major phases: A) The hyaline cartilage model is completely covered with a bone matrix by bone-forming cells called osteoblasts. So, for a time during fetal development, the fetus as cartilage “bones” enclosed by “bony” bones. B) Then, the enclosed hyaline cartilage model is digested away, opening up a medullary cavity within the newly formed bone. Bone formation, Growth, and Remodeling: 2) By birth, most hyaline cartilage models have converted to bone except two regions: A) the articular cartilages (that cover the bone ends) B) the epiphyseal plates The articular cartilage remain for life resisting friction at the joint surfaces. The epiphyseal plates provide for longitudinal growth of the long bones during childhood. Bone formation, Growth, and Remodeling: As new cartilage is continuously being formed on the external surface of the articular cartilage and epiphyseal plate, the old cartilage that is on the inside of the articular cartilage and the medullary cavity is broken down and replaced by bony matrix. Growing bones must widen as they lengthen as well. This process is done by the osteoblasts in the periosteum when they add bone tissue to the external face of the diaphysis as osteoclasts in the endosteum remove bone from the inner face of diaphysis wall. Bone formation, Growth, and Remodeling: Since the process of bony formation and bone widening happens at the same rate, the circumference of the long bones expands, and the bones widen. 3) The process by which bones widen is called appositional growth. This process is controlled by hormones , the most important being growth hormone and, during puberty, the sex hormones. It ends during adolescence when the epiphyseal plates are completely converted to bone. Bone formation, Growth, and Remodeling: 4) Bones are remodeled continually in response to changes in two factors: a) Calcium levels in blood b) the pull of gravity and muscles on the skeleton. How these factors influence bone remodeling involves a number of things. Bone formation, Growth, and Remodeling: 5) When blood calcium levels drop below homeostatic levels, the parathyroid glands (in your throat) are stimulated to release parathyroid hormone (PTH) into the blood. 6) PTH activate osteoclasts, giant bone-destroying cells in bones, to break down bone matrix and release calcium ions into the blood. When blood calcium levels are too high, (hypercalcemia), calcium is deposited in bone matrix as hard calcium salts. Bone formation, Growth, and Remodeling: 7) Bone remodeling is essential if bones are to regain their normal proportions and strength during long-bone growth as the body increases in size and weight. Bones also become thicker and form large projections to increase their strength in areas where bulky muscles are attached. At these sites, osteoblasts lay down new matrix and become trapped within it, and once they are trapped they become osteocytes, or mature bone cells. The bones of people who are bedridden or inactive, tend to lose mass and to atrophy because they are no longer subjected to stress. 8) PTH is the ultimate determinant of when (or if) bone is to be broken down or formed in response to the need for more or fewer calcium ions in the blood. Homeostatic Imbalance: Rickets is a disease of children in which the bones fail to calcify. As a results, the bones soften and a definite bowing of the weight-bearing bones of the legs occurs. Rickets is usually due to a lack of calcium in the diet or a lack of vitamin D, which is needed to absorb the calcium in the bloodstream. Rickets is not usually seen in the US where we put such an emphasis on nutrition. Bone Fractures: 1. Despite the remarkable strength of our bones, they are subject to fractures, or breaks all throughout our lives. Fractures are usually the cause of exceptional trauma caused by sports or other injuries. 2. A fracture in which the bone breaks cleanly but does not penetrate the skin is a closed (or simple) fracture. 3. When the broken end protrudes through the skin, the fracture is open, or compound. Bone Fractures: 4. A fracture is treated by reduction, which is the realignment of the broken bone ends. In closed reductions, the broken ends are coaxed back into position by the physicians hands. In open reductions, surgery is performed and the bone ends are secured together with pins or wires. After the broken bone is reduced, it is held into place by a cast or traction to allow the healing process to begin. Healing time of a closed fracture is 6-8 weeks, but is much longer in larger bones and bones of the elderly due to poor circulation. Bone Fractures: 5. The repair of bone fractures involves 4 major events: A) A hematoma is formed: Blood vessels are ruptured when the bone breaks. As a result, a blood-filled swelling called a hematoma forms. Bone cells deprived of nutrition die. B) The break splinted by a fibrocartilage callus: As we learned about in chapter 3, the first step in tissue repair is the growth of new capillaries into the clotted blood at the site of the damage, and the disposal of dead tissue by phagocytes. As this goes on, connective tissue cells of various types form a mass of repair tissue, the fibrocartilage callus. Bone Fractures: C) The bony callus is formed: As more osteoblasts and osteoclasts migrate into the area and multiply, the fibrocartilage callus is gradually replaced by one made of spongy bone, the bony callus. D) Bone remodeling occurs: Over the next few weeks to months depending on the bone size and the site of the break, the bony callus is remodeled in response to the mechanical stresses placed on it, so that it forms a strong permanent “patch” at the fracture site. The Axial Skeleton: The axial skeleton forms the longitudinal axis of the body and can be divided into three parts: 1) The skull 2) The vertebral column 3) bony thorax The Skull: The skull is formed by two sets of bones: 1) The cranium encloses and protects the fragile brain tissue. 2) The facial bones hold the eyes in an anterior position and allow the facial muscles to show our feelings through smiles or frowns. All but one of the bones of the skull are joined together by sutures, which are interlocking, immovable joints. Only the mandible (jawbone) is attached to the rest of the skull by a freely moveable joint. Cranium: The boxlike cranium is composed of eight large, flat bones except for two paired bones (the parietal and temporal), they are all single bones. 1) The Frontal Bone: The forehead, the bony projections under the eyebrows, and the superior part of each eye’s orbit. 2) Parietal Bones: the paired parietal bones form most of the superior and lateral walls of the cranium. A) They meet in the midline of the skull at the sagittal suture and form the coronal suture where they meet the frontal bone. 3) Temporal Bones: The temporal bones lie inferior to the parietal bones; they join them at the squamous sutures. Cranium: Several important bone markings appear on temporal bone: a) External acoustic (auditory) meatus is a canal that leads to the eardrum and middle ear. b) Styloid Process is a sharp, needlike projection, just inferior to the external auditory meatus. Many neck muscles use the Styloid process as an attachment point. c) Zygomatic Process: is a thin bridge of bone that joins the cheek bone (zygomatic bone) anteriorly. Cranium: d) The mastoid process is a rough projection posterior and inferior to the external acoustic meatus, which is full of air cavities (mastoid sinuses). The mastoid sinuses are so close to the middle ear – a high risk spot for infections – that they may become infected too, a condition called mastoiditis. Also, this area is so closed to the brain, mastoiditis may spread to the brain itself. Cranium: e) Jugular foramen: at the junction of the occipital and temporal bones, and allows passage of the jugular vein, the largest vein of the head, which drains the brain. f) Just anterior to the cranial cavity is the internal acoustic meatus, which transmits cranial nerves VII and VIII . g) Anterior to the jugular foramen on the skull’s inferior aspect is the carotid canal, through which the internal carotid artery runs, supplying blood to most of the brain. Cranium, Occipital Bone: 4) Occipital Bone: The most posterior bone of the cranium and forms the back wall of the skull. A) The occipital bone joins the parietal bones anteriorly at the lamboid suture. B) In the base of the occipital bone is a large opening, the foramen magnum which surrounds the lower part of the brain and allows the spinal cord to connect with the brain. C) Lateral to the foramen magnum on each side are the occipital condyles which rest on the vetebra of the spinal column. Sphenoid Bone: 5) The butterfly shaped sphenoid bone forms part of the floor of the cranial cavity. In the midline of the sphenoid is a small depression, the sella turcica, or Turke’s saddle, which holds the pituitary gland in place. A) The foramen ovale, a large oval opening in line with the posterior end of the sella turcica allows fibers of the cranial nerve V to pass to the chewing muscles of the lower jaw (mandible). B) Parts of the sphenoid, seen exteriorly forming part of the eye orbits, have two important openings, the optic canal, which allows the optic nerve to pass to the eye, and the slitlike superior orbital fissure through which the cranial nerves controlling eye movements pass. C) The central part of the sphenoid bone is riddles with air cavities, the sphenoid sinuses. Ethmoid Bone: 6) The ethmoid bone is very irregularly shaped and lies anteriorly to the sphenoid. It forms the roof of the nasal cavity and part of the medial walls of the orbits. A) Projecting from its superior surface is the crista galli in which the outermost covering of the brain attaches to. B) On each side of the crista galli are many small holes called cribiform plates, which allow nerve fibers carrying impulses from the olfactory (smell) receptors of the nose to reach the brain. C) Extensions of the ethmoid bone, the superior and middle nasal conchae, form part of the lateral walls of the nasal cavity and increase the turbulence of air flowing through the nasal passages. Facial Bones: There are fourteen bones that compose the face, and twelve of these are paired. Only the mandible and vomer are single. 1) The two Maxillae or Maxillary bones fuse to form the upper jaw. All facial bones except the mandible join the maxillae, therefore they are the main bones of the face. A) The Maxillae carry the upper teeth in the alveolar margin. Facial Bones: B) Extensions of the maxillae called the palatine processes form the anterior palate of the hard palate of the mouth. C) The maxillae contain sinuses that drain into the nasal passages known as paranasal sinuses, which serve to lighten the skull bones and act to amplify the sound we make as we speak. 2) The palatine bones lie posterior to the palatine processes of the maxillae and form the posterior part of the hard palate. Failure of these or the palatine processes to fuse medially results in cleft palate. Facial Bones: 3) The zygomatic bones are often referred to as the cheekbones, but they also form a good part of the lateral surface of the eye sockets. 4) The lacrimal bones are fingernail-size bones forming part of the medial walls of each eye socket. Each has a groove that serves as a passageway for tears. 5) The nasal bones are small rectangular bones forming the bridge of the nose. 6) The vomer bone is a single bone in the medial line of the nasal cavity. 7) The inferior nasal conchae are thin, curved bones projecting from the lateral walls of the nasal cavity. Facial Bones: 8) The mandible is the lower jaw and is the largest and strongest bone of the face. It joins the temporal bones on each side of the face, forming the only freely movable joints in the skull. A) The lower teeth lie in the alveoli (sockets) in the alveolar margin at the superior edge of the mandibular body. The hyoid bone: The hyoid bone is closely related to the mandible and temporal bones. The hyoid bone is unique in that it is only bone of the body that does not articulate directly with any other bone. Instead, it is suspended in the midneck region about 1 inch above the larynx where it is anchored by ligaments to the stolid process of the temporal bones. 9) The hyoid bone serves as a movable base for the tongue and an attachment point for the neck muscles that raise and lower the larynx when we swallow and speak. Fetal Skull: The skull of an infant is very different from an adult. The face of an infant is very small compared to the size of the cranium, but the skull as a whole is large compared to the infant’s total body length. An adult skull is 1/8 the total body length, but a newborn is ¼ their body length. 1) In a newborn, the skull also has fibrous regions that have yet to be converted to bone called fontanels. The rhythm of the babies heart can be felt in their fontanels. 2) The fontanels allow the fetal skill to be compressed slightly during birth as well as become flexible to allow the infant’s brain to grow during the later part of pregnancy and early infancy. Labeling: Color and label the skull on your worksheet. Use the colors to help you identify the different parts of the skull. It is on pages 141-143 in your book. We will have a quiz tomorrow over the skull. Vertebral Column (Spine): 1) The vertebral column or spine, extends from the skull, which it supports, to the pelvis, where it transmits the weight of the body to the lower limbs. The Spine is formed from 26 irregular bones connected and reinforced by ligaments in such a way that a flexible, curved structure results. The spinal cord runs through the central cavity of the vertebral column where it is supported and protected. The Spine: Before birth, the spine consists of 33 separate bones called vertebrae, but 9 of these eventually fuse to form the two composite bones, the sacrum and the coccyx. These structure the inferior portion of the vertebral column. 2. Of the 24 single bones: 1. 7 vertebrae are in the neck and are known as the cervical vertebrae. 2. The next 12 are the thoracic vertebrae 3. The remaining 5 support the lower back and are the lumbar vertebrae. Remember common meal times of 7am, noon, and 5pm might help you remember these!! The Spine: 3. The single vertebrae are separated by pads of fibrocartilage known as the intervertebral disks which cushion the vertebrae of and absorb shocks while providing the spine with flexibility. In a young person, the disks have high water content (about 90 percent) and are spongy and compressible. As a person ages, the water content of the discs decreases, and the discs become harder and less compressible. Homeostatic Imbalance: Drying of the disks, along with a weakening of the ligaments of the vertebral column, predisposes older people to herniated (“slipped) disks. Herniation also may result when the vertebral column is subject to exceptional twisting forces. If the protruding disk presses on the spinal cord or the spinal nerves exiting from the cord, numbness and excruciating pain can result. The Spine: 4. The discs and the S-shaped structure of the vertebral column work together to prevent shock to the head when we walk or run. They also make the body trunk flexible. 5. The spinal curvatures in the thoracic and sacral regions are called the primary curvatures because they are present when we are born. 6. Later, the secondary curvatures develop. The cervical curvature appears when a baby begins to raise its head, and the lumbar curvature develops when a baby begins to walk. Homeostatic imbalance: The reason they do “spine checks” in middle school is they are looking for abnormal spinal curvatures. 1. There are several types of abnormal spinal curvatures: A. Scoliosis (s-shaped) B. Kyphosis (hunched) C. Lordosis (reverse hunch) These abnormalities may be present at birth or a result from disease, poor posture, or unequal muscle pull on the spine. Vertebrae Structure: 1. Body, or centrum: is the disc-like, weight bearing part of the vertebra facing anteriorly in the vertebral column. 2. Vertebral arch: the arch formed from the joining of all posterior extensions, the laminae and pedicles, from the vertebral body. 3. Vertebral foramen: the canal through which the spinal cord passes. Vertebral Structure: 4. Transverse processes: two lateral projections from the vertebral arch. 5. Spinous process: single projection arising from the posterior aspect of the vertebral arch. 6. Superior and inferior articular processes: paired projections lateral to the vertebral foramen, allowing a vertebra to form joints with adjacent vertebrae. Cervical Vertebrae: The seven cervical vertebrae form the neck region of the spine. The first two vertebrae (atlas and axis) are different because they perform functions not shared by the other cervical vertebrae. 1. The atlas (C₁) has no body. The superior surfaces of its transverse processes contain large depressions that receive the occipital condyles of the skull. This joint allows you to nod “yes”. Cervical Vertebrae: 2. The axis (C₂) acts as a pivot for the rotation of the atlas (and skull). 3. It has a large, upright process, the dens, or odonoid process, which acts as a pivot point. 4. The joint between C₁ and C₂ allows you to rotate your head from side to side to indicate “no”. Cervical Vertebrae: 5. The “typical” cervical vertebrae are C₃ through C₇ and are the smallest, lightest, vertebrae, and most often their spinous processes are short and divided into two branches. 6. The transverse processes of the cervical vertebrae contain foramina (openings) through which the vertebral arteries pass on their way to the brain above. Any time you see the foramina in the vertebra, you should know that it is a cervical vertebrae. Thoracic Vertebrae: 1. The 12 thoracic vertebrae (T₁ through T₁₂) are all typical. 2. They are larger than the cervical vertebrae, and the body is somewhat heart-shaped and has two costal facets (articulating surfaces) on each side, which receive the heads of the ribs. 3. The spinous process is long and hooks sharply downward, causing the vertebra to look like a giraffe’s head viewed from the side. Lumbar Vertebrae: 1. The five lumbar vertebrae (L₁ to L₅) have massive, blocklike bodies, and have short, hatchet-shaped spinous processes that make them look like a moose head from the side. These are the sturdiest of the vertebrae because most of the stress of the vertebral column occurs in the lumbar region. Sacrum: 1. The sacrum is formed by the fusion of five vertebrae. Superiorly, it articulates with L₅ and inferiorly it connects with the coccyx. 2. The wing-like alae articulate laterally with the hip bone, forming the sacroiliac joints. The sacrum forms the posterior wall of the pelvis. 3. Its posterior midline surface is roughened by the median sacral crest, the fused process of the sacral vertebrae. 4. The vertebral canal continues inside the sacrum as the sacral canal and terminates in a large inferior opening called the sacral hiatus. The coccyx: 1. The coccyx is formed from the fusion of three to five tiny, irregularly shaped vertebrae. It is the human “tailbone”, a remnant of the tail that other vertebrate animals have. Bony Thorax: 1. The sternum, ribs, and thoracic vertebrae make up the bony thorax. 2. The bony thorax is often called the thoracic cage because it forms a protective cone-shaped cage of slender bones around the organs of the thoracic cavity (heart, lungs, and major blood vessels.) Sternum: 1. The sternum (breastbone) is a typical flat bone and the result of the fusion of three bones: 1) Manubrium 2) Body 3) Xiphoid Process It is attached to the first seven pairs of ribs. Sternum: 2. The sternum has three important bony landmarks: 1) The jugular notch – generally at the the level of the third thoracic vertebrae 2) The sternal angle – results where the mubrium and body meet at a slight angle to each other, so that the transverse ridge is formed at the level of the second ribs. 3) Xiphisternal joint – the point where the sternal body and the xiphoid process fuse, lies at the level of the ninth thoracic vertebrae. Ribs: 1. Twelve pairs of ribs form the walls of the bony thorax. (Contrary to popular belief, males do not have one rib less than females!) 2. The true ribs are the first seven ribs and attach directly to the sternum by costal cartilages. 3. The false ribs are the next five pairs, and either attach indirectly to the sternum or are not attached to the sternum at all. The intercostal spaces (the spaces between the ribs) are filled with the intercostal muscles that aid in breathing. Appendicular Skeleton: 1. The appendicular skeleton is composed of 126 bones of the limbs (appendages) and the pectoral and pelvic girdles, which attach the limbs to the axial skeleton. 1. Each shoulder girdle, or pectoral girdle, consists of two bones – a clavicle and a scapula. 2. The clavicle, or collarbone is a slender, doubly curved bone that attaches to the sternum and to the scapula where it forms the shoulder joint. When the clavicle is broken, the whole shoulder region caves in medially, which shows how important its bracing function is. The shoulder girdle: The scapulae are triangular and are commonly called wings because they flare when we move our arms posteriorly. 3. Each scapula has a flattened body and two important processes: 1) the acromion process, which is the enlarged end of the spine of the scapula 2) the coracoid process which is shaped like a beak. The acromion connects with the clavicle laterally at the acromioclavicular joint. The coracoid process points over the top of the shoulder and anchors some of the muscles of the arm. The shoulder girdle: 4. Just medial to the coracoid process is the large suprascapular notch, which serves as a nerve passageway. The scapula is not directly attached the the axial skeleton; it is loosely held in place by the trunk muscles. 5. The glenoid cavity, is a shallow socket that receives the head of the arm bone, is in the lateral angle of the scapula. The shoulder girdle: The shoulder girdle is very light and allows the upper limb to have exceptionally free movement. This is due to the following factors: 1) Each shoulder girdle attaches to the axial skeleton at only one point – the sternoclavicular joint. 2) The loose attachment of the scapula allows it to slide back and forth against the thorax as muscles act. 3) The glenoid cavity is shallow, and the shoulder joint is poorly reinforced by ligaments. This also has a drawback, because the shoulder girdle is very easily dislocated. Bones of the upper limbs: Thirty separate bones form the skeletal framework of each upper limb. They form the foundations of the arm, forearm, and hand. 1. The arm is formed by a single bone, the humerus, which is a long bone. At its proximal end, is a rounded head that fits into a shallow glenoid cavity of the scapula. 2. On the opposite head are two bony projections – the greater and lesser tubercles, which are sites of muscle attachment. 3. In the midpoint of the shaft, is a roughened area called the deltoid tuberosity, where the large, fleshy deltoid muscle of the shoulder attaches. The Arm: 4. Near the deltoid tuberosity is the radial groove, which runs obliquely down the posterior aspect of the shaft. This marks the course of the radial nerve, an important nerve of the upper limbs. 5. At the distal end of the humerus, is the medial trochlea, which looks like a spool, and the lateral capitulum. Both of these processes articulate with the bones of the arm. The Arm: 6. Above the trochlea anteriorly to the depression, is the coronoid fossa; and on the posterior surface is the olecranon fossa. 7. These two depressions are flanked by medial and lateral epicondyles, which allow the corresponding proceses of the ulna to move freely when the elbow is bent or extended. The Forearem: 1. When the body is in the anatomical position, the radius is the lateral bone of the forearm, that is, the thumb side. When the hand is rotated, the radius and ulna will crisscross each other. 2. Both proximally, and distally, both the radius and ulna articulate at small radioulnar joints, and the two bones are connected along the entire length by the interosseous membrane. 3. Both the radius and ulna have a styloid process at their distal end. The Forearm: The disc-shaped head of the radius also forms a joint with the capitulum of the humerus. 4. Just below the head is a radial tuberosity, where the tendon of the biceps muscle attaches. 5. When the upper limb is in the anatomical position, the ulna is the medial bone (on the finger side) of the forearm. 6. On its proximal end are the anterior coronoid process and the posterior olcranon process, which are separated by the trochlear notch. Together, these two processes grip the trochlea of the humerus in a pliers-like joint. Hand: The skeleton of the hand consists of the carpals, the metacarpals, and the phalanges. 1. The eight carpal bones, arranged in two irregular tows of four bones each, form the part of the hand called the carpus or, more commonly, the wrist. The carpals are bound together by ligaments that restrict movements between them. 2. The palm of the hand consists of the metacarpals and phalanges are the bones of the fingers. Hand: The metacarpals are numbered 1 to 5 from the thumb side of the hand toward the little finger. When the fist is clenched, the heads of the metacarpals becomes obvious as “knuckles”. Each hand contains 14 phalanges: 3 in each finger (proximal, medial, distal), except in the thumb, which only has two (proximal and distal). Bones of The Pelvic Girdle: 1. The Pelvic Girdle is formed by two coxal bones, or ossa coxae, commonly called hip bones. 2. Together with the sacrum and coccyx, the hip bones form the bony pelvis. Note the terms pelvis and pelvic girdle have slightly different meanings. Pelvic Girdle: The bones of the pelvic girdle are large and heavy, and they are attached securely to the axial skeleton. The sockets, which receive the thigh bones, are deep and heavily reinforced by ligaments that attach the limbs firmly to the girdle. Bearing weight is the most important function of the girdle; the total weight of the upper body rests on the pelvis. The reproductive organs, urinary bladder, and part of the large intestine lie within and are protected by the bony pelvis. Pelvic Girdle: Each hip bone is formed by the fusion of three bones: ilium, ishium, and pubis. 1. illium – which connects posteriorly with the sacrum at the sacrioiliac joint, and is a large, flaring bone that forms most of the hip bone. When you put your hands on your hips, they are resting on the alae or winglike portion of the ilia. 1) The upper portion of the alae is the iliac crest, an important anatomical landmark for injections. 2) The iliac crest ends anteriorly in the anterior superior iliac spine and posteriorly in the posterior superior iliac spine. Pelvic Girdle: 2. The ischium is the “sit-down bone”, since it forms the most inferior part of the coxal bone. 1) The ischial tuberosity is a roughened area that receives body weight when you are sitting. 2) The ischial spine, superior to the tuberosity, is important in pregnant women because is narrows the outlet of the pelvis through which the baby must pass during the birth process. 3) The greater sciatic notch allows blood vessels and the large sciatic nerve to pass from pelvis posteriorly into the thigh. Any shots in this area must avoid the sciatic nerve as it can cause paralyzation if it is hit. The Pelvic Girdle: 3. The pubis or pubic bone, is the most anterior part of the coxal bone. 1) Fusion of the rami of the pubis anteriorly and the ischium posteriorly forms a bar of bone enclosing the obturator foramen, an opening that allows blood vessels and nerves to pass into the anterior part of the thigh. 2) The pubic bones of each hip bone fuse anteriorly to form a cartilaginous joint, the pubic symphysis. 3) The ilium, ischium, and pubis fuse at the deep socket called the acetabulum, which receives the head of the thigh bone. The Pelvic Girdle: 4. The body pelvis is divided into two regions: 1) The false pelvis is superior to the true pelvis; it is medial to the flaring portions of the ilia. 2) The true pelvis is surrounded by bone and lies inferior to the flaring parts of the ilia and the pelvic brim. The dimensions of the true pelvis of a women are very important because they must be large enough to allow the infant’s head to pass during childbirth. The dimensions of the cavity, particularly the outlet (inferior) and the inlet (superior) are critical, and are carefully measured by the obstetrician. Differences between males and females: The female inlet is larger and more circular The female pelvis as a whole is shallower, and the bones are lighter and thinner. The female ilia flare more laterally. The female sacrum is shorter and less curved. The female ischial spines are shorter and farther apart; the outlet is larger. The female pubic arch is more rounded because the angle of the pubic arch is greater. Bones of the Lower Limbs: The lower limbs carry our total weight when we are standing up. Therefore, it is not surprising that the bones of the lower limbs are the thickest bones in the body. 1. The femur is the only bone of the thigh and is the heaviest, strongest bone in the body. 1) Its proximal end has a ball-like head, a neck, and a greater and lesser trochanters which are separated anteriorly by the intertrochanteric line and posteriorly by the intertrochanteric crest. The trochanter, intertrochanteric crest, and gluteal tuberosity, located on the shaft, all serve as sites for muscle attachment. The Lower Limbs: The head of the femur articulates with the acetabulum of the hip bone. The head of the femur is a common fracture site especially in old age. 2) Distally on the femur are the lateral and medial condyles, which articulate with the tibia below. 3) Posteriorly these condyles are separated by the deep intercondylar fossa. 4) Anteriorly on the distal femur is the smooth patellar surface, which forms a joint with the patella, or kneecap. Leg: Two bones that are connected by an interosseous membrane form the bones of the leg; the tibia and fibula. 1. The tibia, or shinbone, is larger and more medial. 1) At the proximal end, the medial and lateral condyles are separated by the intercondylar eminence and articulate with the distal end of the femur to form the knee joint. The patellar (kneecap) ligament attaches to the tibial tuberosity, a roughened area on the anterior tibial surface. 2) Distally, a process called the medial malleolus forms the inner bulge of the ankle. The anterior surface of the tibia is a sharp ridge, the anterior border, that is unprotected by muscles, thus is easily felt beneath the skin. Leg: 2. The fibula lies alongside the tibia and forms joints with it both proximally and distally, and is thin and sticklike. The fibula has no part in forming the knee joint. 1. Its distal end, the lateral malleolus, forms the outer part of the ankle. The Foot: The foot is composed of the tarsals, metatarsals, and phalanges has two functions; it supports our body weight, and serves as a lever that allows us to propel our bodies forward when we walk and run. 1. The tarsus forms the posterior half of the foot, and is composed of seven tarsal bones. 2. Body weight is mostly carried by the two largest tarsals, the calcaneus, or heelbone, and the talus, which lies between the tibia and the calcaneus. 3. Five metatarsals form the sole, and 14 phalanges form the toes. Like the fingers of the hand, each toe has three phalanges, except the greater toe, which has two. The foot: The bones of the foot are arranged to form three strong arches: two longitudinal and one transverse. Ligaments, which bond the foot bones together, and tendons of the foot muscles help to hold the bones firmly in the arches position but still allow a certain amount of give or springness. Weak arches are referred to as “fallen arches” or “flat feet” Flat feet can tend to be painful after long periods of time on your feet. Joints: With one exception (the hyoid bone of the neck), every bone in the body forms a joint with at least one other bone. 1. Joints, also called articulations, have two functions: 1) They hold the bones together securely 2) Give the rigid skeleton mobility Joints: 2. Joints are classified in two ways – functionally and structurally. The functional aspect focuses on the amount of movement allowed by the joint and has three categories: 1) Synarthroses are immovable joints 2) Amphiarthroses are slightly movable joints 3) Diarthroses are freely movable joints. Freely movable joints predominate in the limbs, where mobility is important. Immovable and slightly movable joints are restricted mainly to the axial skeleton, where firm attachments and protection of internal organs are priorities. Structural Joints: Structurally there are fibrous, cartilaginous, and synovial joints based on whether fibrous tissue, cartilage, or a joint cavity separates the bony regions of the joints. 1. In Fibrous joints, the bones are united by fibrous tissue. The best examples are the sutures of the skull. 1) In syndesmoses, the connecting fibers are longer that those of sutures, thus the joint has more “give”. The joint connecting the distal ends of the tibia and fibula is a syndemosis. Joints: 2. In cartilaginous joints, the bone ends are connected by cartilage. Example: pubic symphysis of the pelvis and intervertebral joints of the spinal column, where the articulating bone surfaces are connected by pads of fibrocartilage. Hyaline cartilage of the growth plates and cartilaginous joints between the ribs are immovable cartilaginous joints. Joints: 3. Synovial Joints are those in which the articulating bone ends are separated by a joint cavity containing synovial fluid. They account for all joints of the limbs. 4 distinguishing features: 1) Articular cartilage covers the ends of the bones forming the joint. 2) Fibrous articular capsule: the joint surfaces are enclosed by a sleeve or capsule of fibrous connective tissue, and the capsule is line with a smooth synovial membrane. 3) Joint cavity: the articular capsule encloses a cavity, called the joint cavity, which contains lubricating synovial fluid. 4) Reinforcing ligaments: The fibrous capsule is usually reinforced with ligaments. Joints: 5) Bursae are flattened fibrous sacs lined with synovial membrane and contain a thin film of synovial fluid. Bursae are common where ligaments, muscles, tendons, or bones rub together. 6) A tendon sheath is an elongated bursa that wraps completely around a tendon subjected to friction, like a bun around a hot dog. Homeostatic Imbalance: A dislocation happens when a bone is forces out of its normal position in the joint cavity. The process of returning the bone to its proper position is reduction, and should be done by a physician. Attempts by an untrained person to “snap” the bone back in place are usually more harmful than helpful. Types of Synovial Joints: Synovial joints can be classified by their shape, which allows for certain types of movement. 1) In a plane joint, the articular surfaces are flat, and only short slipping or gliding movements are allowed. The intercarpal joints of the wrist are the best example. 2) In a hinge joint, the cylindrical end of the bone fits into a trough-shaped surface on another bone. Angular movement is allowed in just one plane, like a hinge. Examples: elbow, ankle, and phlanges. Types of Synovial Joints: 3) In a pivot joint, the rounded end of the bone fits into a sleeve or ring of bone (and possibly ligaments). The rotating bone can only turn around its long axis. Examples: proximal radioulnar joint and the joint between the atlas and the axis. 4) In a condyloid joint, the egg-shaped articular surface of one bone fits into the oval concavity in another. Both are oval. The bone can move side to side and back and forth. Example: Knuckle joints. Types of synovial joints: 5) In saddle joints, each articular surface has both convex and concave areas, like a saddle. Allows for the same movement as condyloid joints. Example: the joint you use when you twittle your thumbs. 6) In a ball-and-socket joint, the spherical head of one bone fits into a round socket in another. These allow movement in all axes, including rotation. Examples: shoulder and hip. Homeostatic Imbalance of Joints: 1. Arthritis refers to over 100 different inflammatory or degenerative diseases that damage the joints. In all forms, arthritis is the most widespread, crippling, disease in the U.S. All forms have the same symptoms: pain, stiffness, and swelling of a joint. Acute (short term) forms of arthritis are usually caused by a bacterial invasion and are treated with antibiotic drugs. Chronic (long term) forms of arthritis include osteaoarthritis, rheumatoid arthritis, and gouty arthritis. Arthritis: 1) Osteoarthritis (OA), is the most common form of arthritis, and is a chronic degenerative condition that typically effects the aged. Over the years, there is softening, fraying, and eventually breakdown of the cartilage. As the disease progresses, the exposed bone thickens and extra bone tissue, called bone spurs, grows around the margins of eroded cartilage and restricts joint movement. The course of OA is slow and irreversible, but is rarely crippling. The disease can usually be treated by aspirin, moderate activity to maintain joint mobility, and rest when the joint becomes very painful. Arthritis: 2) Rheumatoid Arthritis (RA) Is a chronic inflammatory disorder. Its onset usually occurs between the ages of 40 and 50, but may occur at any age. RA is an autoimmune disease – a disorder in which the body’s immune system attempts to destroy its own tissues. RA begins in the synovial joints as the membrane thicken and the joints swell and synovial fluid accumulates. White blood cells enter the joint cavity from the blood and release inflammatory chemicals that destroy tissues when released inappropriately. In time, the inflamed synovial membrane thickens into pannus, an abnormal tissue that clings to and erodes articular cartilage. As the cartilage is destroyed, scar tissue forms and connects the bone ends. The scar tissue eventually ossifies, and the bone ends become firmly fused and often deformed. Arthritis: 3) Gouty Arthritis, or gout, is a disease in which uric acid (a normal waste product of nucleic acid metabolism) accumulates in the blood and may be deposited as needle-shaped crystals in the soft tissues of joints. This leads to a painful attack that typically affects a single joint, often in the great toe. Gout is most common in males and rarely appears before age 30. It tends to run in families. Untreated gout can be very destructive; the bone ends fuse and the joint becomes immobilized. Patients are advised to lose weight if obese, to avoid foods such as liver, kidneys, and sardines, which are high nucleic acids, and avoid alcohol, which inhibits excretion of uric acid by the kidneys. Developmental Aspects of the Skeleton: As described earlier, the first “long bones” in the very young fetus are formed of hyaline cartilage and the earliest “flat bones” of the skull are actually fibrous membranes. As the fetus develops, and grows, both the flat and long bone models are converted to bone. By the end of adolescence, the epiphyseal plates of long bones that provide for longitudinal growth in childhood have become fully ossified, and long bone growth ends. Developmental Aspects of the Skeleton: The skeleton changes throughout life, but changes in childhood are most dramatic. At birth, the baby’s cranium is huge relative to its face. The rapid growth of the cranium is related to the growth of the brain. By 2 years, the skull is three-quarters of its adult size and proportions. Between the ages of 6 and 11, the head appears to enlarge substantially as the face literally grows out from the skull. The jaws increase in size, and the cheekbones and nose become more prominent as respiratory passages expand and the permanent teeth develop. Developmental Aspects of the Skeleton: The primary curvatures of the vertebral column are present at birth and are convex posteriorly, so an infant’s spine is arched. The secondary curvatures are convex anteriorly and are associated with a child’s later development. They result from misshaping of the intervertebral discs rather than from modifications of the bony vertebrae to produce the S-shaped spine typical of the adult. Developmental Aspects of the Skeleton: During youth, growth of the skeleton not only increases overall body height and size, but changes body proportions as well. The lower limbs then grow more rapidly than the trunk. During puberty, the female pelvis broadens in preparation for childbearing, and the entire male skeleton becomes more robust. Once adult height is reached, a healthy skeleton changes very little until late middle ages. Developmental Aspects of the Skeleton: Bones need to be physically stressed to remain healthy. When we remain active physically, and muscles and gravity pull on our skeleton, the bones respond by becoming stronger. If we are totally inactive, they become thin and fragile. Osteoporosis is a bone-thinning disease that afflicts half of the women over 65 and 20 percent of men over the age of 70. Osteoporosis makes the bones so fragile that even a hug or a squeeze can cause bones to fracture. The bones of the spine and neck and of the femur are particularly susceptible. Vertebral collapse typically results in a hunched-over position. Developmental Aspects of the Skeleton: Estrogen helps to maintain the health and normal density of a women’s skeleton, and the estrogen deficiency that occurs after a women goes through menopause is a strong factor in causing osteoporosis. Other factors could be a diet poor in calcium and protein, lack of vitamin D, smoking, and insufficient weight-bearing exercise to stress the bones. Staying active in old age is the best thing you can do for osteoporosis and joint decay. Succumbing to inactivity will only increase the symptoms and the severity of the disease. Essay Question: 1) The fetal skeleton is made up of hyaline cartilage in the long bones and fibrous membranes in the flat bones. 2) As the fetus develops, these membranes turn to bone and by the end of adolescence, the growth plates ossify. 3) The fetal cranium is huge relative to their face. The skull must make adjustments as the brain grows. 4) Later, facial bones must grow as permanent teeth come in. 5) Primary curvatures of the spine are present at birth, and secondary curvatures develop later. 6) The skeleton grows throughout childhood, increasing in both height and weight. 7) Female and male skeletons make changes during puberty to get ready for childbirth and adulthood. 8) Bones begin to decay later in life but an active lifestyle will keep them strong. http://www.youtube.com/watch?v=yfSkOF_DAfA http://www.youtube.com/watch?v=7WXnCS7rBZ4 http://www.youtube.com/watch?v=ntwAUA4HuwY http://www.youtube.com/watch?v=GRSWV57u9eg