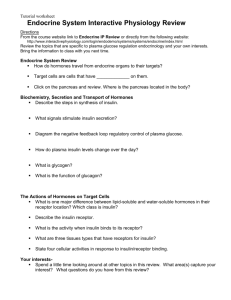
Endocrine Review
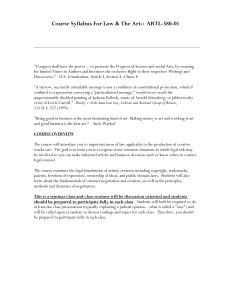
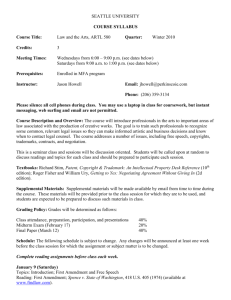
advertisement

Ryan Holzhauer Endocrine physio 2009 Endocrine Review I. GENERAL PRINCIPLES Classical endocrine cell types o Pituitary o Adrenal o Gonadal o Parathyroid o Pancreatic islet Non endocrine tissues with some endocrine function: o Renal cells (erythropoietin) o Cardiac atrial and ventricular (natriuretic hormones) o Gastrointestinal (secretin, glucagon-like peptides, CCK) o Endothelial cells (endothelin, NO) o Lymphocytes, monocytes, macrophages (ILs, interferon’s, tumor necrosis factors) o Platelets and mesenchymal (GFactors, annexins, integrins) o Adipose (leptin, resistin) Endocrine- from classic endocrine cell through blood to distant target cell Neurocrine- from neuron down axon and into blood to distant target cell Paracrine- from one cell type to a neighbor different cell type by diffusion through intercellular fluid channels or gap junctions Autocrine- through intercellular fluid or gap junctions to neighboring identical cells or back to cell of origin Types of Hormoneso Amines- originate from tyrosine thyroid hormones- ionidation of benzene ring chatecholamines- add hydroxyl group to benzene ring o Steroids- cholesterol precursor Adrenal cortical horms Reproductive horms Active metabolites of Vit. D o Prostanoids- cyclization of the unsat FA arachidonic acid Prostaglandins- horm-like signaling molecules. Unstable and rapidly metabolized- action limited to local (paracrine). Important actions: ↑ contraction or relax smooth musc (uterus, bv), modulate neurotransm release, sensitize pain receptors, generate fever, immune responses, induce sleep, GI motility, ion transport in kidney, cell diff, apop, oncogen, platelet activity. Phospholipase A2- enzyme that releases arachidon acid from PLs, cyclooxgenase converts arach to precursor of prostag PGG2. o PGE2 and PGI2 are the most important prosta involved in inflammatory response and sensitization to pain. o PGI2- from endothel cells causes vasodil and inhibits platelet activity (thromboxane A2 vasoconstric and stim platelet) o Proteins/peptidesHormone Synthesiso Protein/Peptide: Protein/peptide horms- made on RER like other prots from mRNA from single gene or different genes in different cells (and 1 gene can give rise to multiple mRNAs and thus multiple peptide horms via different exon splicing and excision) Mature mRNA message begins with N-terminal signal peptide sequencesignal seq docks to receptor on RERtranslation resumes until preprohormone formedsignal peptide cleaved making prohormone while it is directed into cisternae and transported to golgiprohorms and horms sorted into those to be secreted at basal rate and those to be secreted by exocytosis in response to stimuliaccumulate in vesicles packaged for storage in secretory granules (some of which contain proteolytic enzymes like carboxypeptidases for subsequent conversion of prohorm to horm. Golgi processing may also include glycosylation, phosphorylation, palmitoylation, isoprenylation). Peptide horms can be produced in circulation from a precursor (ie angiotensin made from lung and kidney ACE action on angiotensinogen from liver) o Amine and Steroid: requires series of enzymatic reactions, and further modifications to ↑ activity of horms may occur outside gland of origin. Hormone Release: o Both protein and catecholamine horms are stored in secretory granules and released by exocytosis. Extracellular stimulus usually followed by ↑ in Ca+ in cell first from intracellular bound stores, then from extracell through memb channelsthis initiates vesicle movement to sites and fusion with memb Vesicle fusion facilitated by specific vesicle-associated proteins: GTP-binding protein and microtubules and filaments. A secondary rise in cAMP usually follows o Steroid and thyroid hormones- no storage in granules (although compartmentalization may occur). These leave the cell through the membrane when they are made. Horms may be modified in an adjacent cell to produce a different horm with different action (ie estrogens from androgens) o Regulation of Secretion Negative feedback- most common- limits output (ie Horm A stimulates secretion of Horm B which in excess inhibits release of Horm A. Deficit of Horm B causes release of A) Positive Feedback- less common- amplifies initial effect of horm. Neuronal control- evokes or suppresses horm secretion- senses, emotions, fright, injury, etc. Many horms secreted in pulses. Also circadian, diurnal, and ultradian (multiple in a day) rhythms. (SCN in hypothal regulates circadian rhythmintrinsic and entrained. Entrained by light-dark input from nerves from eyes separate from rods and cones. Pineal gland is link between SCN and various physio processes under circadian control- pineal gland cells make melatonin from serotonin which is made from tryptophan) Hormone Action- binds to receptor, horm/receptor complex coupled to signal-generating mechanism (SGM), signal changes cellular processes. o A certain minimal threshold concen needed to elicit measureable response. o Effect obtained at saturating doses of horm is maximal responsiveness of target cell and horm conc needed for half-maximal response is the index of sensitivity of target cell. in maximal responsiveness can be due to in # target cells, # receptors/cell, or in conc of required precursor, or ↑ in a noncompet inhibitor in sensitivity can be from in # or affinity of horm receptors, alteration of conc of cofactors, ↑ in rate of horm degredation, ↑ in antagonistic horm, ↑ in compet inhibitor 2 schemes for hormone action: o 1. Receptor and SGM located within or adjacent to plasma memb- classical of peptide/protein and catecholamine horms and others. Info for response in receptor. When occupied horm changes receptor conformation. Response in seconds to minutes. o 2. Classical of steroid and thyroid horms- hormone enters cell, occupies receptor, and both interact with DNA to alter gene expression. DNA is second messenger. Info for response in horm and receptor together. Response in minutes/hours to days. o Receptor Kinetics: large number of receptors per cell guarantees receptor availability is not rate limiting for horm action. Graph of ratio of bound horm to free horm plotted against bound horm is a Scatchard Plot. Horm occupancy of small number of receptors decreases affinity of nearby unoccupied receptors (occupancy of 5-10% of total available receptors is usually enough to yield full action of horm) so this decrease in affinity does not decrease action of horm but duration of effects and protects cell from overload. An ↑ in receptor # (at saturating concentrations of horm) raises # of occupied receptors and thus raises maximal responsiveness of cell when receptor binding is rate limiting (steroid and thyroid). At submaximal horm concentrations ↑ receptor # enhances sensitivity of cell (like with peptide horms) Downregulation- sustained excess of horm decreases the number of its receptors per cell. However intermittent exposure of target cell to low [horm] can recruit receptors (to ↑ sensitivity of cell) Affinity altered by phosphorylation of receptor, pH, osmolarity, [ions], substrate levels. Plasma Membrane Receptor Systems- plas memb receptors large glycoprots, concentrated on microvilli, binding causes them to cluster. o Extracellular N-term portion binds horm o Intracellular C-term tail (after 1 or many passes through memb) may contain SGM. o After receptor activation complete, complex internalized by endocyt. Then lysosomal degradation of complex, horm and receptor destroyed or receptor recycled back to memb. G-Protein Coupling o 3 classes of plas memb receptors that exert actions via G-proteins and all make 7 passes through memb and have ExC disulfide bridges between cysteins. o G-prots are trimers- , , and subunits binds to receptors, effector molecules, and GDP/GTP. and dimer attach receptor to memb. Inactive G-prot bound to GDP. When horm binds receptor, binds to receptor and releases GDP and binds GTP. This activates G-prot and dissociates from horm/receptor complex and from -. -GTP then binds to nearby memb effector molecule such as adenylyl cyclase and phospholipase C or to ion channel. -GTP activates or inhibits effector as it hydrolyzes GTPGDP. -GDP then reassociates with dimer. This continues as a cycle until horm leaves receptor. Mg+ is required for G-prot cycle. Effector generates many intracellular second messenger molecules- signal amplification from original horm molecule. Second messengers: G-prots couple receptors to at least 3 effector systems: 1. Adenylyl cyclase-cAMP system- PM enzyme adenylyl cyclase catalyzes formation of cAMP from ATP with Mg+ as cofactor. (Gs ↑ cAMP, Gi decreases cAMP). o ↑ in cAMP activates protein kinase A which in turn activates (or deactivates) a number of enzymes in numerous metabolic pathways via phosphorylation. o cAMP may also alter gene expres via CRE (cAMP regulatory element) on DNA that binds transcription factor cAMP response element binding protein (CREB), which is phosph by PKA. o cAMP actions end when it is hydrolyzed by phosphodiesterase o cAMP may also ph PM receptors decreasing their affinity for horms- negative feed-back to limit magnitude or duration 2. Calcium-calmodulin system- G-prot opens Ca+ channels in PM and ER Ca+ acts as 2nd messenger on binding prots and effectors- mainly calmodulinCa+/Calmodulin complex activates or deactivates various Ca+ dependent enzymes. o Ca+/Calmod stim adenylyl cyclase AND phosphodiesterase- so the response is stimulated and dampened later as phsphdiester breaks it down- controls duration of response 3. PM Phosopholipid intermdiates- namely phosphatidylinositol, which is phosph to PIP2. G-prot activates memb bound enzyme phospholipase C which splits PIP2 into IP3 and DAG. o DAG potent activator of PKC. It is also hydrolyzed later into arachidonic acid which makes prostaglandins. o PKC is Ca+ dependant and DAG ↑ its affinity for Ca+. IP3 binds to IP3 receptor on ER, which opens Ca+ channels. So the two together activate and enhance PKC. PKC then ph many enzymes. G-protein linked receptors also activate kinases that promote growth, differentiation, proliferation, apoptosis- MAPK (precursors are MAPKK and MAPKKK)- which ph other cytopl prots and cytoskel prots and nuc transcription factors. Non-G-Prot PM Receptor Mechanisms- extracellular receptor, single transmemb portion, intracytoplasmic C-terminal portion. o 1. binding of horm changes conformation of receptor and receptor becomes tyrosine kinase and autophosphorylates at tyrosine residues or ph other proteins in cell at threonine and serine residues (i.e. insulin receptor). o 2. Binding of horm changes intracell C tail which ph/activates proteins or cytoplasmic tyrosine kinases (i.e. JAK and STAT) docked to tail (GH acts this way) o guanylyl cyclase is another second messenger activated by horm reception on PM. Guanylyl cyclase makes cGMP from GTP. Guanylyl cyclase also binds NO and cardiac and brain natriuretic horms and cGMP mediates their actions. cGMP activates PKG also and cGMP phosphodiesterase breaks cGMP down. Intracellular Receptor Systems- thyroid, adrenal, gonadal steroid horms, vit D. o Horm enters cell, bind receptor usually in nucleus (or cytopl and complex transferred to nuc) o Receptors are large prots, often phosphorylated. o N-term domain binds horm, C-domain binds DNA DNA binding domain has 2 Zn fingers (each with a Zn atom surrounded by 4 cysteine residues) o Unoccupied receptor may inhibit or stimulate transcription of a gene and binding of the horm will then cause the opposite. o DNA in nucleosomes wrapped around histones preventing DNA transcription. Acetylation of lysine res on histones releases DNA and allows for transcription. o Once activated by horm/receptor, promotor nucleotide squences initiate trascrip at start site by RNA polymerase II. Causes regulation of production up or down of enzymes, structural prots, receptor prots, other trascrip factors, etc. o Steroids, thyroid horms, and vit D may have some nongenomic actions, believed to involve G-prots. Hormone Transport- o After secretion, horms circulate either bound or free. Catechols and prot horms are unbound. Steroid and thyroid and vit D bound to globulins made in liver. Bound or unbound changes half-life. Horm Disposalo Irreversible disposal- Target cell uptake and breakdown of horm and urinary or biliary excretion. (MCR-metab clearance rate- vol plasma cleared/unit time). Kidney and liver major sites of hormone extraction and degredation. Horm measuremento Secretion measured by arterial-venous concentration gradients and flow rates across gland. Plasma and urinary excretion rates used as indirect indices of horm secretion rates (valid if metabol or renal clearance is normal) II. HORMONES OF PANCREATIC ISLETS- insulin and glucagon, amylin, pancreastatin, somatostatin, pancreatic polypeptide. Islet from duodenal part of foregut. Proximity of islets to acini permits local effects on exocrine pancreatic func. Islets very vascularized. Capillaries fenestrated. Islet horms secreted into pancreatic vein and then portal vein. 1 million islets- 4 types of cells (gap junct between them): o cells- insulin, make up 60-70% of islet. Core of islet- insulin released bathes other cells. o cells- glucagon, 25% of islet o - somatostatin, 10% o PP cells- pancreatic polypep. and cells have basal (arterial) and apical (venous) face. Between them canliculi that carries interstitial fluid in venous direction. Islets innervated by PS, S, and peptidergic nerves. Islet cells store hormones in granules in apical/venous part. Insulin- 2 straight peptide chains A and B connected by 2 disulfide bonds. (B chain has bio activity) Insulin monomers form crystalline hexameric units with 2 Zn atoms. o Gene has 4 exons/2introns- preproinsulin. N-terminal signal, B chain, A-B connecting peptide C, and A chain. N-terminal signal cleaved at synthesis- proinsulin. A and B chains and C peptide sent to golgi, disulfide bridges made. Packaged in golgi and proinsulin cleaved by proconvertase-1 and carboxypeptidase-H to remove C peptide (stays in granule with insulin), released together. (insulin associates with Zn in granule) Insulin synthesis stimulated by glucose/feeding. Glucose upregulates insulin gene and enzyme genes that promote glycolysis and downregulates those of gluconeogenesis. o Secretion- within 1min of exposure to gluc. Cells in center of islet respond faster. Insulin release also follows an intrinsic cycle of oscillation of cell memb potential (which opens Ca+ channels)- controlled by unknown pacemaker. 1- Glut-2 transporter in canaliculi between cells facilitates diffusion of gluc into cell to maintain conc in cell equal to interst fluid. 2glucokinase is gluc sensor that controls cell response (also in endocrine cells of gut and hypothal nuclei), it ph gluc, and is rate limiting step. Then glycolysis yields pyruvate and lactateinsulin release signal. Release parallels rate of gluc oxidation. (pyruv and lactate made INSIDE not from outside cell stim insul release). 3-oxid of gluc ↑ ATP/ADP ratio, NADH, and NADPH, and H+. (when UCP-2 uncouples oxphos from ATP production insul release is decreased). 4-ATP-sensitive K+ channel closes, less K+ leaving, cell depolarizes which opens voltage sensitive Ca+ channel, Ca+ ↑ in cell, granule movement on microtubules, GTPase on granule interacts with PM protein fusin which fuses granule to PM, insuline hexamer release which dissociate to dimers and bioactive monomers in portal vein. (a similar mech occurs, with respective specific transporters, in response to AAs – esp arginine and lysine- and ketoacids). Also after gluc exposure a rise in cAMP causes insul release via cAMP dependent protein kinase that ph exocytosis prots and facilitates GTP/GDP exchange. Glucagon stimulates insulin release through Gs and somatostatin inhibits insulin release through Gi prot. Ach stim insul release via Gs linked to PLC which generates DAG, IP3, and ↑ PKC activity. Gluc and FA oxid ↑ acetyl-CoA and FFA-CoA and this leads to ↑ DAG and more activation of PKC. (although long-term cell exposure to FFA stimulates apoptosis) o Regulation of Secretion- feedback mech with nutrient/glucose supply (no response when gluc below 50mg/dL, half-max response at 150mg/dL, max response at 300mg/dL) Biphasic response to continuous gluc stim- initial immediate pulse of insulin peaks at 1min and returns toward baseline. At 10min second phase, levels rise more slowly and maintained for hours. Oral gluc causes greater response than plasma infusion of gluc because of GI horms (GLP-1 and GIP) released in response to meal capable of potentiating gluc-stimulated insulin secretion. Somatostatin released within pancreatic islets (paracrine or neurocrine) and from intestinal cells (endocrine) may dampen insulin response to meals. Symp nerves/epinephrine stimulate insulin secretion via -adrenergic receptors but inhibit insulin via receptors. PS vagus ↑ insulin release. ↑ in cells (hyperplasia) ↑s insulin release- caused by antagonistic horms that block insulin action ↑ing the need of tissues for insulin releaseinclude cortisol, GH, hman placental lactogen, and thyroid horms. cell has insulin receptors- insulin negative feedback on its own secretion. Can also cause cell hyperplasia however (positive FB). Leptin inhibits insulin synth and release- opens K+ channel Basal insulin level= 10U/mL. Circulates unbound- half life 5-8min. Cpeptide release equally with insulin but has higher levels in blood due to lower clearance rate (func unknown) o Action- rate limiting step is transport of insulin through cap. wall. Main targets are muscle, liver, adipose. Combines with PM glycoprot receptor (member of gene superfam that codes for growth factor receptors)-alternate splicing gives: Insulin receptor A- fetal cells, then all brain, lymphocytes, and spleen. Receptor B- muscle, adipose, liver, kidney. Insulin combines with receptor, conf change in recept, they aggregate, horm-recept complex internalized, horm degraded, recept degraded, stored, or recycled to PM. Insulin downregulates receptor by ↑ rate of degradation and suppress synth. Receptor tyrosine kinase activity (in cytopl subunit) activated by binding of insulin and ATP inside- autoph subunit at 3 tyrosines. Now fully active receptor. Ph tyrosines on 4 insul receptor substrates (IRS-1 nad IRS-2 in muscle/adipose and IRS-3 in brain). These are activators of other prot kinases, phosphatases, phospholipases, and other G-prot linked prots involving serine/threonine phos. Ultimately this activates PI-3-kinase and PI-3 causes synthesis of and translocates gluc trasporters to PM (via PKB?) from cytopl pool of vesicles and activates/deactivates enzymes in gluc metab, and represses or transcribes genes in nucleus. Glut-4- transporter in muscle and adipose (insul stimulates Glut-4 gene). Vesicles in cyto with receptors have snare protein VAMP-2 which docks to syntax-4 on PM. At low insul, gluc transport into cell is rate limiting step of gluc use- Glut trasporters facilitate diffusion. IRS-1 also activates growth recept binding prot-2 (GRB-2) which binds GTP to ras which goes on to stimulate glycogen synthase and cell growth and diff via MAPK (inhib apop) Sometimes PLC generated 2nd messengers (DAG, IP3) needed for insulin action In some cells insulin lowers cAMP by activating phosphodiesterase. ↑s celluptake of K+, Mg+, and phosphate (all required for prot anabolism and glycogen synthesis). Also ↑ uptake of these ions in kidney. stimulates gluc conversion in cell to glycogen, pyruvate, lactate, and to FA. (glycogen production ↑ by dephosph of glycogen synthase via insulin inhibition of glycogen synthase kinase and by insulin stimulation of a phosphatase) Synthesis of albumin and casein ↑. Inhibition of proteolytic and lipolitic enz protects prot and TG stores. Stimulates translocation of Na+K+ATPase to PM, increasing energy expenditure. Inhibits translocation of its own receptor Inhibits glucagon release from pancreas Insulin circulates CSF reaching receptors in brain causing decrease of neuropeptides-Y release and decrease of hunger (food intake can be stimulated in other ways when hyperinsulemia pursues. o Action in Liver- EC gluc equilib quickly with IC gluc via Glut-2 transporter Insulin enhances uptake of gluc by inducing hepatic glucokinase (glucgluc-6-phosphate), then insulin promotes storage as glycogen by activating glycogen synthase complex. stimulates glycolysis by stim phosphofructokinase and pyruvate kinase (committed steps). Stimulates ox of pyruvate and lactate by ↑ pyruvate dehydrogenase activity. Inhibits glycogenolysis by decr glycogen phosphorylase and gluc-6phosphatase activity Inhibits hepatic uptake of AA and therefore gluconeogenesis. Pyruvate shuttled to acetyl-CoA (not to gluconeogen) Opposing processes when gluc levels fall after insulin action: portal vein and hypothalamic sensors sense hypoglycemia and stimulate glucose output via symp ns. Pancreatic islets also sense hypoglycemia which then secret glucagon. FFA that enter liver in circulation are shunted away from oxidation and ketogenesis, rather they are reesterified with glycerol from glycolysis to make TGs. GlucoseFA stimulated. Acetyl-CoA in mito (from pyruvate) transferred to cyto by citrate and changed to malonyl-CoA (by acetyl-CoA carboxylase which is a rate limiting step in FA synthesis that insulin stimulates). Malonyl CoA also inhibits carnitine acyl transferase which is used to move FA into mito for oxidation and ketoacid production (so this is inhibited) stimulates Hexose monoph shunt to make NADP (necessary for FA synthesis) o Action in muscle- stimulates transport into muscle. Pyruvate dehydrog activated for gluc oxidation Glycogen synthase activated Muscle blood flow ↑ via NO synthesis (although this is partly countered by insulin stimulation of endothelin-1 a vasoconstrictor) Suppresses lipoprotein lipase, FFA uptake, FFA release from TGs and FFA oxidation. o Action in adipose- enhance storage and block oxid of FA. Blood flow ↑ via NO Inhibits hormone-sensitive lipase activity by decr cAMP and inhibiting PKA (this decr FFA flow to liver thus decr in generation of ketoacids by liver) Stimulates use of ketoacids by tissues- only antiketogenic horm Stimulates deposition of circulating fat by activating lipoprotein lipase (which breaks VLDLs and chylomicron TGs to FFA making them available for transfer into adipose cells) o Insulin effect on protein Anabolic- causes sequestration of AA and protein in all tissues (in muscle stimulates Na+dependent transport of neutral AAs. Stimulates synthesis of macromolecules in tissues like carilage and bonethus directly contributes to growth (also by directly stimulating transcription of other growth factors like IGF-1) Other -cell Products- packaged and secreted with insulin o Amylin- non-competitive antagonist to insulin by decreasing gluc uptake in muscle o Pancreastatin- inhibits insulin secretion- auto-feedback regulation Glucagon- single straight chain peptide. N-terminal for receptor binding and bioactivity. Made from preproglucagon precursor of -cells. o Glucose/insulin inhib glucagon synth- repress gene transcrip (via a CRE and insulin-responsive element on gene). Blood flow carries insulin released to cells which inhibits glucagon. o Glucagon stored in secretory vesicles released with Ca+ ↑ o Regulation of Secretion- maintain glucose levels in the face of ↑ tissue demand released in hypoglycemia, and after protein meal (esp arg and ala). Response to prot dampened if gluc or insulin is also present. FFA and gluc suppress glucagon. Glucagon stimulates production/release of glucose, FFA, ketoacids which neg feedback on glucagon. AA stimulate glucagon and glucagon stimulates conversion of AA to glucose. GLP-1 (a proglucagon product of GI) and secretin inhibit glucagon release. Glucagon levels after meal change much less than insulin- because protein and carbs have opposite effect on cell and same effect on cell. Several day fast = 2x plasma glucagon levels. Exercise ↑ glucagon. PS vagal/Ach- stimulates glucagon. Symp/ adrenergic stim- ↑ glucagon a lot Neurohorm somatostatin inhibits glucagon. Circulates unbound- half-life of 6min. Binds to hepatic PM glycoprot receptorGsadenylyl cyclase/cAMPcAMP dependent PKAphos numerous enz kinases or phosphatases activating or deactivating them i.e. PKAactivates phosphorylase kinaseactivates glycogen phosphorylaseglycogenolysis ↑. (glucose-1-phosphate released is prevented from returning to glycogen by inhibition of glycogen synthase) phos of phosphofructokinase and pyruvate kinase decreases their activity and thus glycolysis. Glucagon affects liver (muscle and adipose almost not at all- no effect on peripheral tissue glucose usage and no influence on BCAA levels so no effect on muscle proteolysis). Mainly ↑ glycogen breakdown. Also ↑ AA uptake (esp alanine). Lowers fructose-2,6-bisphosphate levels which decr phosphofructokinase and ↑ fructose-1,6-bisphosphatase activities, thus ↑ gluconeogenesis and decr glycolysis (opposite insulin) Glucagon effects transient- hepatic autoreg by hyperglycemia stim insulin release which turns off glucagon. In liver directs incoming FFA to -oxidation, away from TG synth. Inactivates acetyl-CoA carboxylase which catalyz the rate limiting step in FFA synth from cytoplasm acetyl-CoAresults in lower level malonylCoA the inhibitor of carnitine acyltransferase, so faster influx of fatty acyl-CoA into mito for conversion to ketoacids. Activates adipose tissue lipase which ↑ lipolysis and FFA delivery to liver. Decreases hepatic cholesterol synth. Inhibition of renal Na+ absorption (natriuresis) Activates myocardial adenylyl cyclase↑ in CO Insulin:Glucagon Ratio- normal is 2.0. During mobilization and ↑ use it drops to .5 (in fasting and exercise). After a meal may ↑ to 10. Only small change after high protein meal. Fat almost no effect. Glucagon-like Peptide-1- product of preproglucagon expressed in intestinal L-cells (esp of ileum and colon)- half life 2min. o Released into blood stream. o PreproglucagonGLP-1 by enzyme proconvertase-1. o Released in response to nutrient intake (AA, gluc, galac- not intravenous) and to cholinergic and -adrenergic stim. o Acts on PM receptor linked to aden cycl/G-prot↑ cAMP. o Actions include stim of insul release by augment cell response to gluc, stim of insul synth and cell prolif by ↑ expression of IPF-1. Also decr glucagon and gastric emptying. (all tend to lower plasm gluc). o Also expressed in hypothal and brainstem. In CNS acts to decr food and water intake, ↑ diuresis. Somatostatin- hypthal neuropeptideo inhibits GH, insulin, glucagon, HCl, pepsin, gastrin, secretin, GI juices secretion, pancreatic exocrine func, and gastric, duodenal, and gallbladder motility, and inhib absorption of gluc, xylose, and TGs across mucosal memb. (these all help to prevent rapid nutrient overload). o Also made in cells of pancreatic islet (SS-14) and a larger version in intestinal cells (SS-28). Release stim by cAMP. o Gene product prosomatostatin. o Stimulated by gluc, AA, FFA, some GI horms, glucagon, adrenergic and cholinergic. Inhibited by insulin and adrenergic. Pancreatic Polypeptide- product of PP cells (same fam as neuropep Y in hypothal) o Secreted in response to food via GI secretions and cholinerg stim. Also stim by hypoglycemia and inhib by gluc. o Action- to inhibit exocrine pancreatic secretion by inhibiting AA uptake by panc acinar cells. III. REGULATION OF CA+ AND PHOSPHATE METABOLISM Calcium- IC storage pool- free calcium total= .2mg, 9g bound in ER, mito, PM. 4x more free EC Ca+. Skeleton/teeth- 1-2kg Ca+ (99% of total). In plasma total Ca+ (bound+free)=9mg/dL (40% bound albumin, 50% free ionic bioactive form). Plasma pH ↑↑ in Ca+ bound to prot (alkalosis) (acidosis ↑ ionic free form of Ca+). Recom min daily intake= 800mg. decreased plasma free/ionic [Ca+] causes neuromusc irritability, numbness, tingling, tetanic musc contractions, larynx muscle spasms can obstruct airway, CNS irritabilityseizures. o Demonstrates adaptive absorption- high intake, lower fraction absorbed (and vice versa). o Bone remodeling- EC pool of Ca+ 1000mg in equilib with skeletal pool. o Ca+ sensing PM receptor- G prot linked- on surface of endocrine and other cells that have imp roles in Ca+ homeost- incl cells that secrete PTH, calcitonin, vit-D, bone cells, renal tubular and intestinal Ca+ reabsorbing cells. Ca+ binds to EC N-term portion of receptor at 2 serine residues. IC portion has sites to be ph by PKA and PKC (PKC ph reduces func of receptor) Gprotaden cyclase, phospholipases A2, C, and D, and MAPK and tyrosine kinases. Overall effect to alter rates of entry or exit of Ca+ to and from ECF to protect against hypo and hypercalcemia. Phosphate- integral component of intermediates in metab of carbs, lipids, prot, forms part of high-energy transfer compounds (ATP), cofactors (NAD, NADP), second messengers (cAMP, IP3), DNA/RNA. Important anion to balance K+ and Mg2+ in cell. 85% total ph in body in bone, 6% in muscle. Depletion results in skel muscle weakness, cardiac/resp muscle disfunct, loss of RBC memb integrity, abnormal bone formation. o Normal plasma [ph]= 3.5mg/dL. 70% of ph ingested is absorbed consistently (adaptive absorption not significant like for Ca+). Renal tubules can reabsorb up to 100% of filtered ph (average 90%). Total EC pool 500mg. Magnesium- divalent (Mg2+)- related to Ca and ph- essential in neuromusc transmission, cofactor in many enzyme rxns esp. those involved with energy transfers from ATP and prot synth. Mg depletion from intest malabsorption, alcoholism, diuretic overuseneuromusc irritability, vent arrithmias. o Normal plasma- 2.0mg/dL- 1/3 bound to protein. Body total- 25g, 50% in skeleton, 50% in ICF. o Usual daily intake 400mg, 40% absorbed, same amount excreted in urine. o Mg regulates its own concentration prob via Ca receptor (lower sensitivity binding to receptor than Ca) Bone Dynamics- 75-80% bone mass is cortical bone- the dense concentric outer layers of appendicular skel (long bones) and thin outer layer of flat bones. 25% is trabecular bone- bridges spicules that make up large inner parts of axial skel (skull, ribs, vert, pelvis) and smaller interior of shafts of long bones (trabec bone has 5x more total surface area than cortical bone- greater accessibility so more imp in bone turnover (cotical bone turns over much slower) o Linear growth at long bone ends by replacement of cartilage (endochondral bone form) at epiphyseal plates. Growth plates closed at end of puberty. Bone width added to periosteum. o Remodeling- bone turnover- Ca+ homeost maintenance. o Cell types: Osteoblast- from pluripot stem cells within con tissue of mesenchyme which can differentiate into adipocytes, myoblasts, chondrocytes, osteoprogenitor cells depending on influence of BMF (bone morphogenic factors/proteins). 1/3 of osteoblasts become lining cells or Osteocytes, 2/3 apoptosis. Lifespan 3mo. Osteocyte-lifespan 20 years. Lining cells-initiate cycle of remodeling in each osteon Osteoclast-from same bone marrow stem cells that also become macrophages and circulating monocytes. A factor secreted by differentiating osteoblasts is required for osteoclast differentiation from precursor. 2wk lifespan. o Bone Formation and Resorption- occurs within osteons or bone modeling units. During embryo and growth years formation exceeds resorption- skel mass ↑. After age 35 resorption>formation (esp women). Bone formation- done by active osteoblasts Synth and extrude type I procollagen molecule into EC space where it is processed to interconnecting collagen. o Line up in regular arrays to produce organic matrix called osteoid. Calcium then deposited as masses of calcium phosphate10 days for mineralization. Then hydroxide and bicarbonate ions added to mineral mix to slowly form mature hydroxyapatite crystals. Osteoblasts also secrete alkaline phosphatase, osteocalcin, and osteonectin which regulate bone quantity and quality (osteoblastic activity measured by plasma levels of osteocalcin and alkaline phos) o Osteonectin- binds to collagen and complex in turn binds hydroxyapatite crystals. o Osteocalcin- has -carboxyglutamate residues which bind Ca+ and uncrystallized hydroxyapatite. Mineralized bone accumulates and surrounds osteoblast and cell decr synthetic activity and becomes interior osteocyte. (osteoblastic activity at bone surface- either concentric lamellae of cortical bone or linear lamellae of interior bridging trabeculae. Lining cells on these surfaces). Mineralization requires adequate plasma Ca+ and ph and is dependent on vit D. Interior osteocytes remain connected with surface lining cells and other osteocytes via syncytial processes that run in canaliculi. Permits transfer of Ca+ from enormous surface area of interior to exterior of bone and then to ECF- transfer called osteocytic osteolysis (which does not decrease bone mass bone removes Ca+ from most recently formed crystals). Resorption- not just removing Ca+ but destroys matrix of bone- decr bone mass. Done by osteoclast- multinucleated (10-20 nuc) big cell formed by fusion of precursors. Before resorption begins thin outer layer of unmineralized osteoid must be removed via collagenase released from lining cells- they also release molecules that attract osteoclasts to site of now denuded bone. Osteoclast attaches to endosteal and periosteal surfaces of bone modeling units- this is mediated by integrins. Ruffled border is created by infolding of oclast membrane. Then bone dissolution via type 4 collagenase, phosphatase, and lysosomal enzymes. Essential local acidic environ created by ATP proton pump. Oclast literally tunnel way into mineralized bone. Ca+, ph, hydroxyproline and hydroxylysine (unique to collagen) and col cross-linkage products pyridinolines are released into ECF. Transforming growth factor stimulates apoptosis in oclasts, inhibits apop in oblasts. o Remodeling- Coordination of Resorption and Formation- remodeling occurs in areas of bone that have been structurally weakened by fatigue, mechanical stress, or disuse. Mechanism of coupling- if resorption is stimulated, will be at least partially balanced by a secondary ↑ in formation. Deep osteocytes are mechanoreceptors- pick up signals transmitted via interstitial fluid (mech stress ↑ flow of fluid in canaliculi) ocytes respond by ↑ PLC, Ca+, and PKC activity which lead to stim of PLA2 and prostaglandin production (PGE2) PGE2 reaches lining cells via syncytial processes/canaliculi- lining cells initiate recruitment and differentiation of oclasts via communication with stromal precursors in bone marrow. Resorption triggered by signals from oblasts and precursors. Oclasts form and secrete annexins- signaling molecules that recruit more oclasts from precursors. After old bone resorption and clean-up by macrophages, formation by oblasts occurs at same site to fill it with new strong bone (resorption lasts 10 days, formation 3mo) Vitamin D- is activated to hormone 1,25-(OH)2-D which ↑ Ca absorption from intestine and resorption from bone- to ↑ plasma Ca. (similar role on ph) o acquired from production in skin from UV irradiation (D3 or cholecalciferol) and from diet (D3 and D2) (fish, liver, irradiated milk- RDintake=10g). Not produced by endocrine gland but undergoes modification, acts on distant cells= hormone. (D2 has extra double bond fro plant sterol ergosterol) o D3 synth in keratinocytes in epidermis- 7-dehydrocholesterolprevitamin D3 (via UV)spontaneously converted over 3days to D3/cholecalciferol (via thermal energy from sun). Continuous exposure to sun also phtodegrades previtamin D3 to inactive products- restrains overproduction. Also inhibited by 1,25 and stimulated by PTH. o Fat soluble so absorption in intestine mediated by bile salts, via lymphatic glands. Excess stored in liver and adipose. o In liver microsomal (ER) and mito enz hydroxylates vitD25-OH-D (rxn requires NADPH and O2)then to kidney to be hydroxylated to either 1,25 (requires flavoprotein renoredoxin or ferredoxin and 1-hydroxylase) or to 24,25(OH)2-D (via 24-hydroxylase) (both are rxns in mitochondria of kidney proximal and straight tubules and require NADPH and O2) 24,25 bioactivity debatable but much less potent than 1,25 Regulation of 1,25 production from kidney. 25-OH-D production in liver inhib by product 1,25 (and1,25 suppresses 1-hydroxylase synthesis and activity as do Ca+ and ph). When vitD, Ca, or ph is lacking 25 directed toward 1,25 production. Ca deprivationhypocalcemiastim PTH hypersecretion. Both PTH ↑ and Ca decr independ stim synth and activity of 1-hydroxylase. Ph deprivationhypophosphatemiadecr renal cortical [ph]directly stim 1-hydroxylase activity Thus supply of active 1,25 is ↑ when mobilization of Ca or ph from intestine and bone into ECF is needed and rxn is shuttled toward prod of inactive 24,25 when vitD, Ca, and ph are plentiful (if 1,25 excess develops 1,25 can still be1,24,25 by 24-hydroxylase. 25/1,25/24,25 all circulate bound to -globulin (half-life 3 days)-binds to 25 w/high affinity and to 1,25 low. 1,25 has shortest half-life and lowest concentration of the three. o Vit D Actions- acts as steroid horm. Receptor in cyto and nucleus. Major action is to stim absorption of Ca from intestine against conc gradient. Binding induces receptor ph and this complex then attaches to 1,25 regulatory elements on target DNA molecules. Vit D receptor upregulated by 1,25, PTH, insulin-like growth factors, estrogen, and cortisol. Vit D may downregulate Ca receptor in some target cells (positive feedback that augments the effect of vit D and raises plasma [Ca]) One major product of 1,25 action is calcium binding proteins calbindins. Bind Ca ions- homology with calmodulin and MyosinLCK. Also has rapid memb effects of ↑ in cGMP and IC Ca levels. 1,25 localizes to nuc of intestinal villus and crypt cells (not to goblet of submucosas). It acts on brush border ↑ # of Ca pumps in basolateral memb. Hrs after Ca entry from lumen to capillaries has ↑, calbindin concent rises to ferry Ca across intestinal cell and or buffer high Ca conc now in cells. Rate of Ca absorption in duod is proportional to cell content of calbindin. Also stim active absorption of Mg and Ph across intestinal cell memb Other major target is bone. Oblasts (NOT oclasts) have 1,25 receptors. Nonetheless it stimulates resorption via stim of cytokine signal that oblasts sends out which ↑ recruitment, different, and fusion of precursors into oclasts which then resorb bone. (PTH is req for 1,25 stim resorption). Also stim osteocytic osteolysis Normal mineralization of bone also depends of vit D. without it excess collagen synth is not inhib by oblasts and bone is weak. (1,25 induces synth of osteocalcin in oblasts) 1,25 may stim cartilage growth in epiphys plates. Neg feedback- inhib gene for PTH and inhib PTH receptor expression in oblasts. Weakly stim renal Ca reabsorption by ↑ # of Ca pumps. Stim Ca transport into skel and cardiac muscle. 1,25 can also be made from 25 in keratinocytes. 1,25 inhib proliferation of these cells and stim their differentiation. Vid D regulates formation of cornified layer epidermis. Macrophages, monocytes, and some lymphos can make 1,25 from 25, which then stim T-helper-2 cell secretion of IL-4 but inhib TGF and Thelper-1 cell secretion of IL-2, interferon, and tumor necrosis factor. T and B cell and Ig production inhibited. Macrophage and oclasts have common precursor so they are probably recruited together to site of resorption. Receptors also in pancreatic islet, ant pit, hypothal, placenta, ovary, aorta endothel, and skin fibroblasts. Parathyroid Hormone: secreted by PT gland. Main effect is to ↑ plasma Ca by direct stim of bone resorp and renal tubular Ca reabsorp and indirect stim of renal 1,25 synth. It also decreases plasma Ph levels by inhib renal tubular Ph reabsorption. o 4 PT glands devel from 3rd and 4th branchial pouches, descend post to thyroid. Chief cell- predominant cell- source of PTH. Oxyphil cell- appears at puberty- eosinophilic. o Synthesis and Release of PTH- single chain prot. Bioactivity in N-terminal portion. Precursor- prepro-PTH. N-term signal seq removed in 2 stepsproPTHto golgi where pro-PTHPTH. Some PTH packaged in secretory granules for later release. Dominant regulator of PT gland activity is plasma Ca levelneg feedback. Maximal PTH release at total Ca levels under 7mg/dL (3.5mg/dL ionized- it is actually the free ion Ca levels that regulate). Normally ↑ in Ca influx into a cell ↑ hormone or vesicle release but opposite is true with PTH more Ca, less PTH release. Ca receptor on PM of PT cells- ↑ in binding of Ca to receptorinhib aden cyclase and activates PLCrise in IP3rise in IC Ca and fall in cAMPinhib exocyt of PTH granules. High Ca binding also represses PTH gene transcrip and proliferation of PTcells. (suppression is lifted at low Ca binding to receptor and PTH release ensues, also low Ca ↑ PTH synth, cell prolif, and decr in PTH degredation in PTcells). Mg influences PTH release same as Ca. Rise in plasma Ph causes immediate fall in plasma Ca which stimulates PTH secretion. Ph also directly causes ↑ in PTH secretion. (Ph shifts PTHCa curve to right- raising set point of Ca suppression of PTH secretion). 1,25 inhib trascrip of PTH gene and decreases secretion, inhib proliferation of PT cells. It upregulates Ca receptor in PT cells (all decreasing plasma Ca level) = neg feedback. (PTH ↑s 1,25 synth). PTH pulsatile- higher at night (indep of Ca levels). Aging decreases Ca absorption↑ PTH secretionbone resorption ↑ PTH secretion stim by- phosphodiesterase inhibitors (↑ cAMP levels), epinephrine (-adren receptor), dopamine, histamine. PTH inhib by- -adrenergic agonists, prostaglandins (both decrease cAMP) PTH split in liver- rapidly metabolized in periph tissues. Plasma conc = 30pg/mL. o PTH Actions: initiated by binding to PM receptor. Overall to ↑ plasma Ca and decr plasma Ph by direct action on bone and kidney and indirect on GI (PTH actually ↑ Ph influx via its action on bone and GI, but this is overwhelmed by efflux action on kidney Constant exposure to PTH downregs receptors but intermittent upregs. Horm binding to receptor causes G-prot activation of aden cyclaseph of prot for Ca/ion transport. Independent of cAMP, PTH stim uptake of Ca into bone cells from fluid. 1,25 presence and IC Mg necessary for full effects of PTH Bone: PTH receptors on oclasts and oblasts. Accelerates removal of Ca from bone 2 ways: Stim osteolysis (Ca only from bonecanaliculi fluidECF) Stim oclasts to resorb mineralized bone (Ca and PhECF) via ↑ activity of collagenase (↑ expression of collagenase gene). PTH induces ↑ in acid phosphatase and carbonic anhydrase and accumulation of lactic and citric acid to lower pH for resorption. Oblasts and oclasts necessary for horm induced resorp- PTH inhib syth of collagen in oblasts. Also stim release of paracrine oblast products that stim oclast resorption. (although in low intermittent dosis, PTH stim bone formation and collagen production via ↑ in IGF and TGFs). So whether PTH causes ↑ or decr in skeletal mass depends on other factors like exercise, and Ca, Ph, vit D levels. Kidney: PTH ↑ reabsorption of Ca in ascending loop of Henle and distal tubule of kidney. Major effect is inhib Ph reabsorp in proximal tubule (↑ ph excretion) by inducing lysosomal degradation of Na-Ph co transporters. Allows for excretion of Ph released by resorption (otherwise Ca/Ph precipitates could form in tissues). In low plasma Ph, Ca ↑ and inhib PTH. PTH inhib reabsorp of Mg, Na, and bicarbonate in prox tubule and stim Na/H exchanger which acidifies blood to prevent alkalosis (from release of bicarbonate from hydroxyapatite crystals in resorp). *Most important action in kidney- stim synth of 1,25 via ↑ cAMP. PKA indirectly activates the dephosphorylation of ferroptorein renoredoxin to activate- required for activity of 1-hydroxylase (which is also enhanced by lower Ph levels caused by PTH). ↑ vitD production ↑s Ca absorption from intestine. PTH-Related Hormone: expressed in keratinocytes, lactating mammary epithel, placenta, fetal PT glands. o Exhibits most of PTH actions except stim of 1-hydroxylase (so vit D levels are not ↑ by PTHrp). o Most important role is regu of endochondral bone formation. Chondrocytes stim to make type 2 collagen but in orderly fashion so lengthening occurs at epiph plates. Also imp in breast development. After puberty and closing of epiph plates, sex horms stop production of PTHrp. Calcitonin: released by parafollicular cells of thyroid (of neural crest origin). Acts to lower plasma Ca. o Gene makes preprocalcitonin. (gene also encodes calcitonin gene related peptide or CGRP a potent vasodilator and cardiac inotropic agent). o ↑ in plasma Ca stim release of calcitonin via Ca receptor on PM and ↑ in cAMP leading to calcitonin release. o Circulating concentration 20pg/mL. o 1,25 and ingestion of food ↑ calcitonin levels (even if food has no Ca- prevents hypercal- caused by gastrin) o Actions: Target in bone is oclastbinds to PM receptor↑ in cAMPcauses deactivation of oclasts and resorption Antagonist to PTH in action of Ca, but same effect on Ph (to lower it in blood)- caused by decr in resorption, promotion of Ph entry into bone, ↑ in urinary excretion. (also ↑ Ca urinary excretion). Effects of PTH and vit D much more pronounced and controlling than calcitonin. If thyroid is removed, hypercalcemia does not occur. But calcitonin does protect against excessive resorption when demand for Ca ↑ like during pregnancy, lactation, growth, etc. Hormonal Regulation of Ca and Phosphate: o Ca deprivationhypocalcemiasignals Ca receptor to stim PTH↑ bone resorption and renal tubular Ca reabsorption, ↑ Ph excretionraise plasma Ca, lower plasma Ph, ↑ plasma PTH↑ 1,25 production↑ GI Ca absorption and osteolysis and resorption. So plasma Ca ↑, and Ph released into plasma with Ca from resorption is excreted by kidney. Recovery of plasma Ca levels turns off PTH secretion by neg feedback and by suppressive effect of 1,25 on PTH synth. 1,25 prod then decr and 24,25 ↑. If plasma Ca overshoots regular levels too high, calcitonin kicks in. o Phosphate deprivationhypophosphatemiastim 1,25 production, inhib PTH↑ Ph absorption in intestine and ↑ bone resorptionCa that also enters blood from resorption also shuts off PTH release which ↑ renal Ph absorption. Lack of PTH also permits renal excretion of Ca. Plasma Ph returns to normal and 1,25 synth inhibited or shuttled to 24,25 o Renal responses to PTH are fastest defense against these ion imbalances. o Renal and intestinal responses defend against imbalance of total body and total bone stores. o Skeletal mechanisms defend against plasma imbalance. IV. Hypothalamus and Pituitary Anatomyo Adenohypophysis(anterior)- ectodermal upward pouching of (Rathke’s) from oral cavity roof- sphenoid bone pinches off. Blood- sup. hypophyseal art- supplies superior part of stalk Caps drain to portal veins extending to AH- portals form new cap plexus which drains to dural sinus. also receive blood from viens from cap plexus in neural stalk (AH has very little direct arterial blood) AH is collection of endo cells regulated by stimuli in blood from neurons of hypothal- horm release from ah requires neuro AND endo cells Hypothal neurons make releasing/inhib hormstravel down axons to median eminence at hypo/pit junchorms stored in neurosecretory granules in terminals hypothal stimulatedreleasing/inhib horms released into med eminenceenter cap plexus of sup. hypoph artportal veinsexit 2nd cap plexus in AH to reach target cells (neurohorm signals from nh also arrive via short portal veins)endo cells respond by releasing or inhib horm granule releasehorms enter same cap plexus short portal veins may also allow reverse flow of blood from AH thru NH back to axons in median eminence and hypothal- allows for short-loop feedback endocrine to neural (feedback to pit from CSF may also occur via ependymal cells from third ventricle that send long processes to to vessels of median eminence and stalk) Precursor (reg by prot Pit-1) give rise to 5 cell types in AH (in order) Corticotrophs Thyrotrophs Gonadotrophs Somatotrophs Mammotrophs AH also has folliculostellate cells- release ILs and TNF- modulate endocrine func Tropic hormones- ACTH, TSH, LH, FSH, GH, prolactin- synth/stored mainly by horm specific endo cells in ah- Release stim/inhib by horms produced in hypothal AH horms- slow metab clearance rates o Neurohypophysis(posterior)- ectoderm downward pouch of ectoderm of floor of 3rd ventricle Axons from cell bodies in hypothal.- bodies make peptide hormstravel down axon in neurosec granulesstored in terminals in NH- term invested by astroglial cells (pituicytes)- horm release of NH requires neuro cell only Stim of cell bodiesgranules releasehorms enter circ via cap plexus Peptide horms- ADH (arginine vasopressin) and oxytocin- made in large neurons in supraoptic and paraventricular nuclei of hypothal; stored and secreted by NH Blood- inf. hypophyseal art.- also serves inf. stalk Fenestrated caps drain into dural sinus o 2 pouches fuse sides into infundibular process separating inferiorly- superiorly stalk expands investing lowest portion of hypothal (median eminence [ME]) o cleft remnant of Rathke’s pouch demarcates ant/post pit (some animals have intermediate lobe next to NH o pit sits in saddle of sphenoid bone- sella turcica- dura matter membrane (diaphragm) stretched across top, separating pit from brain (infund stalk penetrates) Hypothalamic Function- lateral hypothal receives afferent nerves from thalamus, reticular-activating substance, limbic system (amygdala, olfactory bulb, hippocampus, and habenula), the eyes, and neocortex- using norep, Ach, serotonin. Efferent pulses to median eminence use dopamine, Ach, GABA, -endorphin- regulate discharge of releasing/inhib horms into adjacent caps. o Long loop feedback- peripheral gland horms and substrates of metab exert feedback control on hypothal and AH (usually neg) o Neg feedback also exerted by tropic horms themselves on synth or discharge of related hypothal releasing/inhib horms- short loop fb (either via reverse flow or special transport across BBB to hypothal neurons) o Ultra-short-loop feedback-hypothal-releasing horms may inhib own synth by stim discharge of paired inhib horm to suppress its own secretion- via transmission between 2 hypoth cells or transport via pit tanycytes to CSF and back to hypothal o At AH the hypothal releasing horms accelerate AH secretion and peripheral target gland horms inhib o Small cells beneath 3rd vent in arcuate and periventricular nuclei of medial basal hypothal make various hypothal-releasing/inhib horms (some of these neurons also in paraventricular nuc)- axons to median eminence o 1 cell type in hypo produces each neurohorm- except CRH and ADH found together. o AH gland cells make and store some of the hypothal horm that influences themshows autocrine/paracrine control. o Hypothal horms synth via preprohorms- pulsatile release bind to PM receptors on AH cellsIC [Ca+] changed and hence cAMP, IP3, DAG, and arachidonic acidprots ph by activated PKA or PKCgranule exocytosis and tropic horm releasetropic horm synth also stim or inhib by ↑ or decr transcrip of genes PACAP- (pituitary adenylyl cyclase-activating peptide)- hypothal horm found to affect AH horm release and FS (folliculostellate) cell IL-6 release, AH cell development, apoptosis- also widespread effects like insulin secretion, bone metab, melatonin synth, adrenocortical and medullary function, gonad func, vasodilation, erection Adenohypophysis Hormones- peptides o ACTH, GH, prolactin o and 3 glycoprots- TSH, LH, FSH identical -subunit, distinct -subunits- from different genes and gene products must be combined- 3 dimensional form via S-S bonds each has different primary target cell- bind to class 1 PM receptors- linked to G-prot/adenylyl cylcase/cAMP second messenger. All downregulate their recep. Esterified to sulfuric acid and sialic acid- after enzymatic removal of sialic acid in circ- hepatic and renal clearance. degree of glycosylation during synth determines clearance rate- o TSH- 5% of cells of AH, in anteromedial area- regulate growth and metabolism of thyroid gland and secretion of its horms thyroxine (T4) triiodothyronine (T3) TSH synth- separate genes for and subunit- N-term peptide removed from each primary translation product (or prehorm)N-term sugar added to protecttravels thru ERgolgi where sialic and sulfuric acid added, disulfide bonds formedsubunits combine to make TSH and stored in secretory granules Transcription of TSH subunits stim by TRH from hypo, and inhib by thyroid horm. TRH also modulates glycosylation process to ↑ bioactivity, thyroid horm modulates this process to decr bioactivity TSH secretion- TRH ↑ rate of secretion, thyroid decr (neg fb) TRH stored in med. eminreaches PM receptors on target cells (thyrotrophs) via pit portal veintriggers Ca+ influx and ↑ in IP3/DAGTSH exocytosis release- plasma levels rise 10x, back to baseline in 60min. (TRH downreg its own receptors. T3 also decreases # of TRH receptors) Hypothal has 3 kinds of thyroid horm nuclear receptors- T3 in hypothal acts via one of these to inhib synth/release of TRH. Modulation of TSH secretion- fasting and cold. o TRH release and TSH response decr in fasting- causes lower metabolic rate to adjust for no energy intake. o TSH augmented in cold (in animals and probably humans)↑s thermogenesis via thyroid gland stim. o Diurnal variation- highest level at night o TRH stim by leptin o Tonic inhibition of TSH by hypothal peptide somatostatin and hypothal dopamine. o TSH inhib by GH. o TSH/TRH inhib by cortisol (from adrenal cortex). TSH action- binds to PM receptor, cAMP second messenger. Effects are on thyroid gland- promotes growth and differentiation, stim all steps of thy horm secretion: o Iodide uptake and its organification o Completion of thyr horm synth and release o ACTH- polypeptide horm- from corticotrophs (make 20% of AH- found in pars distalis)- ACTH reg growth of adrenal cortex and secretion of its steroid horms (most important cortisol) N-term has bioactivity. C-term protects horm from degredation ACTH Synth- its initial gene product can yield several bioactive molecules. Its mRNA makes preproopiomelanocortin- later processed to ACTH or other products (i.e. -lipotropin, -lipotropin, -endorphin, and the N-terminal peptide- and within these lies melanocyte-stimulating hormone or MSH) ACTH Secretion- reg by hypothalamic CRH made in paraventricular nuc. CRH circ bound to specific protein CRH (via Ca+2 and cAMP) stimulates synth and release of ACTH and of proopiomelanocortin coproducts. (ADH also has corticotropin-releasing activity/enhances CRH action). o CRH also has receptors in CNS- causes CNS arousal, ↑ symp activity, ↑ BP. Decr feeding, growth, and reproductive func. via decr synth of GnRH and gonadotropins and inhib sexual behavior. o CRH also stim activity of immune cells and their release of cytokines ACTH circ unbound- hl 5min ACTH has diurnal pattern- peak 2-4hrs before waking (cortisol entrained in this pattern). o Nocturnal surge generated by activity in suprachiasmatic nuc by CRH- surge can be completely suppressed by excess cortisol (which decreases expression of CRH gene) o ACTH pulses 3/hr- cortisol pulse 10min later- peaks of ACTH caused by ↑ amplitude of pulse Inhibition/neg FB by: o cortisol- it blocks CRH action in pit- also induces lipocortin-1 in FS cells (paracrine inhib in pit) o ACTH inhibits itself- via decr CRH release (short-loop fb) o Atrial natriuretic horm (and analogs)- inhib CRH + ACTH (cortisol also ↑ expression of ANH gene) ACTH stimulation by: o Stress- may override FBI- GABA dampens ACTH response to FBI- hypoglycemia stimulatory effect augmented by norep () and serotonin. o Insulin induced hypoglycemia- stim cort, ACTH, GH o Cytokines from activated lymphos o IL-6 from FS cells ACTH Action- stim growth of cortex (cell hypertrophy not hyperplasia) and synth and secretion of cortisol and other horms Binds to adrenal cell PM receptorcAMP ↑. ↑ skin pigmentation due MSH sequences- MSH acts on melanocytes to disperse melanin granules o Gonadotropic Horms- LH and FSH- glycoprots- reg growth, development, puberty, reproduction, gonad sex horm secretion. Both secreted by gonadotroph cells (15% of AH)- cycles of differential expression at different timessteroidogenic factor-1 stim fetal gonadotrophic development and func LH and FSH have common -subunit, unique - both have carb moities for binding and ↑ rate of degredation of LH, sialic acid res decrease rate of FSH degredation. Also sulfation and sialylation cause variation in bioactivity (more basic forms= higher potency, but shorter hl. In women stores in pit fluctuate and are highes just before ovulation. LH/FSH Secretion- reg by hypothal horm GnRH (aka. LHRH)- causes greater rise LH than FSH- GnRH from arcuate nuc and preoptic of hypstored at ME in granules- GnRH release reg by: Dopamine, serotonin, noradrenergic, endorphinergic influence, phermones (stim and inhib), light input from retina reg light-dark cycle of GnRH release o Melatonin from pineal gland mediates seasonal gonadotropin secretion and reprod cycle based on day length (in some species, maybe humans) Inhibition: o Dopamine- inhib GnRH + LH directly at gonadotrophs o Endorphins- inhib both GnRH and LH o Melatonin- supressed by light, stimulated by dark, inhib GnRH o Stress/CRH- inhib GnRH (sperm production/menstruation inactive during stress) o Gonadal products- (after menopause ↑ in FSH/LH- less FBI by ovaries) Testosterone(androgen from testicular Leydigs + ovarian interstitial cells) and estradiol (estrogen from ovarian granulosa cells + Leydig + sertoli cells)- most important FBI of LH (and partly FSH)inhib transcrip, decr # GnRH receptors, inhib GnRH secretion and pit response to GnRH Progesterone- inhib and stim- depend on timing Inhibin- gonad glycoprot product- main FBI of FSH- inhib FSH transcription, GnRH secretion (much less effect on LH) Follistatin- binds activin to inhibit o Prolactin- inhib GnRH o LH- short-loop inhib Stimulation: o GnRHo Estradiol- stim and inhib- depends on dose o Progesterone- stim and inhib- depend on timing/dose o Activin- gonad/pit product stim FSH synth and release GnRH-triggered release begins with binding to class 1 PM receptor on gonadotrophCa+/calmodulin, IP3/DAG, PKCgranule release o GnRH also stim transcrip of LH/FSH genes o GnRH downreg and upreg its receptor (receptors also found in gonads and prostate) GnRH causes biphasic response in LH and uniphasic for FSHboth pulsatile due to pulsatile GnRH o Women response much greater during ovulation o Men 8-10 LH bursts/day o Pulses amplitude greater in puberty. o FSH pattern synchronized with LH but lesser magnitude Differences in LH and FSH secretion due to either: another unknown stimulating horm of FSH, different gonadotroph responsiveness to GnRH, pulse pattern of GnRH (shorter pulses favor LH, longer FSH), or temporal influences of sex steroids. FSH/LH circ unbound- higher levels in women in first half of menstrual cycle (sharp peak on day of ovulation)- MCR- 36(LH) and 20 (FSH) L/day- 1 (LH) and 3(FSH) hr half-lives (slower degradation of FSH due to high sialic acid content) FSH/LH Action- class 1 PM G-prot PM receptorcAMPCREB/CREM-P transcrip factors initiate expression of target genes FSH- stim ovarian granulosa/testic Sertoli cells to syth estradiol and inhibin and other speermato/oogenisis proteins LH- stim ovarian interstitial (thecal) and testic Leydigs to secrete testosterone and other products for reproduction o LH action requires fast turn off- accompolished by arrestin which inactivates receptor/horm complex Both downregulate their receptors o GH (somatotropin)- stim postnatal somatic growth and development; protein, carb, fat metabolic actions. From somatotrophs (40-50% of AH)- (tumor secreting GH can cause acromegaly)- regulated by GHRH GH Synthesis- transcription factor Pit-1 (specific to pit) necessary for GH transcripmRNAprehormonesignal pep cleavedstored in granules Synthesis stim by GHRH, inhib by somatostatin (from hyp) GHRH acts via cAMP and Pit-1 in ↑ PKA ph of CREB on GH gene. (histone actylase activity also ↑ to expose gene on DNA) GH Secretion- stim by GHRH- secreted in 10-20 pulses/day GHRH binds to PM receptorCa+/cAMP cause release, IP3/DAG mediate action Inhibito Somatostatin- blocks GHRH stimulation through its own PM receptordecrease cAMP/Ca+ o Carb rich meal- (and FFA)- ↑ somatostatin release o -adrenergic stimo NPYo GH- inhibit self by stim somatostatin o Somatomedins (insulin-like growth factors)- inhib GHRH and stim somatostatin o GHRH- inhib GH in doses too small to stimulate o Cortisol and thyroid horm- in large doses o Insulin- represses GH gene transcrip o Obesity- dampened GH response to all stimuli Stimulateo Prostaglandinso Fall in plasma glucose or FFAo Prot rich meal- or AA (esp arg- inhib somatostatin) o Fasting- stim due to decr gluc/insulin and decr FBI o Exercise and stresses- surgery, fever, etc- augmented by adrenergic stim o Nocturnal peak- 1hr after deep sleep peak in GHRH o GHRP- growth hormone-releasing peptide- ↑s pulse burst, not frequency o Neurotransmitters- dopamine, norep, Ach (inhib somatostatin), serotonin, GABA, histamine- all stim GHRH or inhib somatostatin o Leptino Cortisol and thyroid horm- at basal doses Greater in premenopausal women than men (more per burstexplained by greater affect of estradiol than testosterone on GH secretion), greatest just before ovulation. GH greater in children, rises through puberty, decreases in adults and further in elderly o Decrease in elderly responsible for decrease in body mass, fitness, prot synth, metabolic rate, and ↑ in adipose. 1 circ GH binds to 2 plasma prot identical to receptor- GH hl 20min, MCR 350L/day GH Actions- anabolic!- many actions carried out by somatomedins IGF-1 and 2 Stimulation of linear growth- action on epiphiseal plates o Stim all actions of chondrocytes, their differentiation, proliferation, hypertrophy, DNA/RNA/prot synth Stim cellular uptake of AA ↑ activity and # of bone remodeling units o Stim bone resorption and formation (more formation) Hypertrophy/hyperplasia of visceral organs (↑ in func), glands, muscle, heart (CO ↑), skin, CT Sensitizes gonads to LH/FSH- promotes sex maturation GH required for normal pancreatic islet func o Creates insulin resistance, ↑ hepatic gluconeogen/glycogenolysis (glucose release), faster clearance of insulin o ↑ lipolysis- plasma FFA o Metab rate ↑- gluc oxid decr, FA oxid ↑ ↑ plasma vol- stim renin-angio-aldos axis by suppressing ANP ↑ plasma Pi- (prox tubular reabsorption ↑) ↑ in vitD production and thus Ca+ reabsorp from intestine GH Mechanism of Action- 1 GH must bind 2 receptors-(thus excess GH inhib its own action)- also excess GH downregs its receptors o Receptor recruits IC tyrosine kinases (Janus kinases), docks them, activates STAT prots via ph o Receptor induced by insulin + estrogens, inhib by fasting o Responses to GH delayed 12-18hrs- transcription of somatomedins (IGF) required (related to proinsulin)- made primarily in liver (also locally in tissue) HL of IGFs long- bound to 6 carrier prots (IGFBP16)- insulin and IGFs suppress IGPBP expression. Cortisol, glucagon, and cAMP ↑ it. Thus in fasting when insulin levels fall, IGFBP levels rise so free IGF levels fall- promotes substrate flow o IGFs stimulate growth responses in cartilage, muscle, adipose, fibroblasts, etc, and enhance nitrogen retention. Bind to their own PM receptors- some similar to insulin’s- intrinsic tyrosine kinase activityph IRS1activates PI3 kinase and PKB and mitogenactivated kinaseinhibit apoptosis in target cells IGF-2 receptor not like insulin receptor- binds IGF1 but not insulin. Found mostly in embryo and important for implantation, DNA synth/cell cycle, and embr and placental develp o o o o IGF-1 receptor found later in life- stim DNA synth/cell cycle and postnatal neuronal development GH and IGF-1 important for immune develp Both stim BMF production IGF production reduced and overridden by fasting, low energy, low protein intake, insulin deficiency despite ↑ in GH (lack of IGF is probably reason for elevated GH due to lack of FBI) When prot and energy intake are both ample, insulin and GH ↑ and stim prod of IGFs for overall anabolism Insulin antagonistic affect on GH is to prevent hypoglycemia When only carbs are taken in, insulin is stim and GH inhib- no prot anabolism necessary when no AA intake. When gluc levels fall, insulin decr, GH ↑ (↑ lipolysis) but deficit of calories and of insulin inhib IGF prod- this is good when prot anabolism is not advantageous and prot catab is necessary. Estrogen and cortisol decrease IGFs o Prolactin- stim breast develop and milk prod- influences reprod func and immune responses- from mammotrophs (aka lactotrophs) (10-25% of pit)- these cells ↑ in # during preg and lactation and in response to estrogen (somatomammotrophs can secrete GH and prolactin) Prolactin Synthesis- from prehorm. N-term signal cleavedNglycosylationto golgi deglycosylated and stored in granules (although some escapes before deglycosylation and supplies a basal level of less active prolactin) Prolactin Secretion- TRH ↑ transcription, dopamine decreases it ↑ steadily during pregnancy- prob due to ↑ estrogen which stimulates hyperplasia of prolactin cells and prolac transcrip Inhibition- uniquely prolactin is tonically inhibited by the hypothal o Dopamine- inhib prolac transcrip- prolactin-inhibiting factor (PIF)- binds to mammotrph to decr cAMP/Ca+ o Somatostatin o GABAo Prolactin- inhib its own synth/release- short-loop by incr dopamine Stimulationo Estrogen- stim transcrip of prolac (and its receptor) o Removal of hypothal inhibitiono TRH- stim transcrip, hyperplasia of mammotrphs o Gonadotrophs- responding to GnRH have paracrine stimulation via angiotensinII o Night- circadian rhythm night ↑ o Stress- surgery, insulin induced hypoglycemia, fear, etc o Oxytocin- short portal vein delivery- suckling o PrRP- prolactin releasing peptide- stronger w/estrogen Prolactin Action- breast develp in puberty and preg, lactogenesis With estrogens, progesterone, cortisol, GH stim branching of ducts in breast, develp of breast lobules of alveoli during preg, milk synth and with oxytocin maintains milk Binds to PM receptor like that of GH- 1 prolactin binds 2 receptorscyto tyrosine kinaseph STAT prots (upregs its recep) Stim cell uptake of AA and induces transcrip of genes for milk prot and lactose Stim synth of FA and phospholipids in breast Estrogen and progest inhibit prolactin affect of milk prodction Prolac has inhib and stim effects on reproduction (depends on cycle stage). Excess prolac inhib GnRH- prevents ovulation in females and sprm prod in males Stim protective parental behavior Stim produc of synlactin in liver- helps prolactin (like IGF for GH) Needed for immuno balance of fetus and mother Neurohypophysis Hormones- ADH (conserve body water/regulate osmolarity) and OTC (eject milk/uterine contractions)- both synth in cell bodies of hypothal. o ADH from supraoptic nuc and OTC from paraventricular nuc o genes on same chrom- gene products include the horm and other proteins called neurophysins- neurophysin I for OTC and II for ADH (role unknown) o ADH and OTC Synthesis- processing of preprohormones OTC and ADH bound to their Nphysin carrierspackaged in acidic neurosecretory granulesdown axons to post pit terminal swellings called Herring Bodiesreleased when depolariz from stim of cell body travels to Herring bodies↑ Ca+granules release horm dissociates from nphysin in neutral environmententers capillary via enoth cell endocyt o ADH Secretion- reg by osmotic and vol stimuli Hyperosmolarity induces loss of ICF from osmoreceptors in hypoth causes ADH release (and stim thirst) Solutes that don’t cross PM like Na+ can cause hyperosmo also, solutes like urea do not trigger ADH release ↑ of Na+ in CSF also stim ADH release Water ingestion suppresses osmoreceptor firingshuts off ADH release ADH initially suppressed by swallowing water Inhibition Blood infusion- or isotonic saline sol ↑ blood vol Pressure receptors- tonic inhibition of ADH ANP- released by heart and brain Ethanol Cortisol Thyroid horms Solute diuresis Water loading PGE- interferes with ADH activation of aden cyclase K+ deficiency Ca+ excess Lithium Stimulation ↑ in plasma osmolarity hypovolemia- sensed by pressure sensors in carotid and aorta, stretch receptors of atria and pulm veins, renal juxtaglom cells9/10th cranial nerves to medullaadrenergics to supraoptic nuc of hypoth (normally blocked by adrenerg tonic inhibition) o ADH release due to decr impulses from baros to brainstem o Hypovol also directly stim renin and angiotensin in brain (angiotensin II stim release of ADH and thirst) Decrease in CO or BP- ie hemorrhage, stand up, etc. response to hypotension stronger than to hyperosmolarity Pain/stress Heat o o o o o o Nausea/vomiting Inflammatory cytokines Old age Tetracycline antibiotic Circ unbound- binds to platelets HL 5min, MCR 600mL/min (urine clearance always 5% of MCRthus is valid index of secretion) ADH Action- main action on renal cells responsible for water reabsorp- cells lining distal convoluted tubule and collecting ducts of medulla- ↑ their perm to water. Class 1 PM G-prot receptor (V2) on capillary/basal sideCa+/cAMP and IP3activates luminal/apical prot kinaseph aquaporin-2 channelap-2 channels transported to luminal memb – back diffusion of water (urea also reabsorb) Also acts on ascending limb of loop of Henle- enhance Na+ transport into interstitium of medulla to ↑ osmolarity and help diffuse water out of filtrate Also acts directly on vascular smooth musc to constrict via V1 receptor, Ca+ and PLC generated 2nd messengers (V2 receptor causes vasodilation prevent over constriction) (also V1 vasoconstrict spermatic cord- ejaculat) Also acts as corticotropin-releasing factor via portal veins to AH Also neurotransmitter in brain- regulates memory, temp, BP, circadian rhythms, development OTC Secretion- circ unbound, HL 4min, degraded by kid/liver Inhibition Opioid/endorphinergic input Progesterone- inhib OTC-receptor binding Catecholamines Stimulation Suckling- afferent sensory receptors in nipple to CNS Crying baby Estrogens Female sex activityOTC Action- binds to PM receptors (affinity ↑ by Mg+ and cholesterol, inhib by progesterone)Ca+, IP3/DAGcontract myoepith cells of alv of mam glands or of uterus Ca+/calmodactivate myosinLCKcontract smooth musc uterus/myometrium Receptor in uterus- terminates corpus luteum at end of menst cycle Receptor in testis, epididimus, prostate- move sperm, add seminal fluid, ejac V. Thyroid Gland- reg metab, O2 utilization, growth and development. From endoderm from pharyngeal gut- descends ant neck. Innervated by thyrocervical arteries and autonomic NS. Endoth cells surround follicle lumen (follicular cells) where new hormone is stored as colloid material. Close to follicular cells are parafollicular cells or C cells- source of calcitonin. Thyroid Hormone Synthesis and Release- secretory products- iodothyronines- 90% thyroxine/T4, 10% triiodothyronine/T3. o Circulating pool of iodide of 250-700g- thyroid takes up 75g/day (total thyroid iodide= 7500g in form of hormone). o Iodide transported in against electrochem gradient by membrane Na+I- symport system (NIS)- iodide trap require energy (NIS gene inhib by iodide, stim byTSH) o Iodide transported into lumen of follicles by I-Cl- transporter (pendrin)iodide oxidized and incorporated into tyrosine tied to thyroglobulin (glycoprot) from RERCHO moieties addedgolgifollicle lumen, thyroglobulin iodinatedforms monoiodoryosine (MIT) and diiodotyrosine (DIT)2 DITs = T4, 1DIT + 1MIT= T3 All of these reactions catalyzed by thyroid peroxidase (TPO) on follicular memb H2O2 (made via O2 and NADPH) accepts electrons for iodideiodine rxn When iodide is low or when gland hyperstim by TSHT3 favored (more potent) o Iodinated thyroglobulin stored in lumen as colloid- release of T4 and T3 requires proteolysis of thyroglob and endocytosis retrieval by endoth cell. Megalin receptor- uptake of tg from follicle- receptor/cell memb form pseudopods- engulf pocket of colloid o Engulfed colloid moves through cyto toward basal memblysosomes fuse with colloid dropletproteases release free T4 and T3leave basal end of cell and enter blood o MIT and DIT engulfed with tg are deiodinated in cell by deiodinase and recycled Regulation of Thyroid Glando TSH binds to PM receptorG protaden cyclase/cAMP/IP3/DAGiodide uptake and all other actions, insulin/IGF (req for tg synth). TSH also gluc ox via HMPshunt for NADPH production (for peroxidase rxn). o Inhibition Free T4/T3- (free not bound T3/4) at pit TSH secretion- FBI High iodide levels- iodide too high NADPH prod and NIS/TPO genes (effect known as Wolff-Chaikoff) Thyroglobulin- inhib TSH-receptor binding and aden cycl response Ach- inhib via cGMP Fasting Aging- decrease in TSH Thiouracils- hyperthyroidism meds suppress peroxidase and hence T3/4 o Stimulation TSH- stim all steps, transcrip of genes for NIS, tg, TPO, megalin, hypertrophy/plasia of follicular cells, capillaries/blood flow Iodide available- activity proportional to amount of iodide at low levelsiodide and tg upreg pendrin levels. Night- TSHtg synth, iodide trapping, and all steps of T3/4 synth and release Epineph and VIP- stim T4 release via cAMP Prostaglandins Calorie ingestion- esp CHOs T3 and metab rate Leptin- stim TRH neurons directlyTSHT4 Cold- TSH response to TRH T3/T4 Hormone Action: metabolic rate, heat production, O2 use, energy expenditure T Hormone Metabolismo T4 dominant for secreted and circulated (T3 2-3x more bioactive, 10x the affinity for the receptor than T4) Major portion of T3 derived from circulating T4- T4 like a prohorm for T3 T4 much lower MCR Most T4T3 conversion occurs in tissues with high blood flow and rapid plasma exchange like liver and kidneys o T3/T4 circ entirely bound to prot- 70% bound to thyroxine binding globulin (TBG)- glycoprot from liver- TBG:T4=1:1 binding TBG maintains large circ reservoir of T4 which buffers changes in thyroid Serine protease cleaves bondaffinityTBG dumps T4 (i.e. happens on contact with activated leukocytes) o Other binding prots: 15% bound to transthyretin (TTR)-lower affinity than TBG but > capacity 15% bound to albumin- lower affinity than TBG, > binding capacity TTR and albumin deliver T3/4 to cells 3% bound to lipoproteins o degradation in liver, kidneys, skeletal muscle- rate of degradation depends on free [T4] in plasma. o Most T4 that is released from thyroid is deiodinated (T4T3) (first step in T4 metabolism and important for action), 15% excreted in bile Enzymes that diodinate T4T3T2T1 – they depend on selenium. T4T3 by D2 (in pit, sk muscle, brain, BAT) Inactive rT3T2 by D1 These enzymes regulate the circ concentrations of the different active and inactive forms of thyroid horm T Hormone IC Actions o T3/4 enter cell by energy dependent carrier- like AA transporter- transport of T4 is the rate limiting step of IC production of T3 Transport inhibited by AA, FFA, carnitine. T4T3bind to nuc receptor of steroid family acts as transcription factor and receptors- 1 in brain liver kidney, 2 in pituitary and hypothal (T3 downregs 2 receptor) receptor statically inhibits target gene production- inhibition lifted when T3 binds- target genes include GH, osteocalcin, myosin chains, lipogenesis enz, TSH, T3 receptor itself. Effects in nucleus include stim of RNA polymerase and phPKs. Also mito respiration, respiratory chain enz produc stimulated o temphypoth sympathetic activityBAT activity via norep – all of this including # of receptors for norep in BAT stimulated T3 stim promotor for UCP-1, 2, and 3 gene to uncouple oxphos o T horm activity of PM Na+K+ATPase o T3 stim adenine nucleotide translocasemito ATP/ADP exchange o Also tim AA uptake by cellsprot synth T Horm General Body Effects o METABOLISM: Ox consumption o gulc and FA uptake and oxidation o RQ (more increase in FA oxidation than gluc) o heat production, body temp- compensated by heat loss via blood flow, sweating, and ventilation. o glycolysis/glycogenolysis o gluc absorption from intestine and gluc turnover o lipolysis (via -adrenergic recep), o protein turnover/degredation (and to lesser extent protein synth), urea prod o effects of epineph, norep, glucagon, cortisol, GH on gluconeogenesis, lipolysis, ketogenesis, proteolysis o OVERALL- accelerates response to starvation, o RESPIRATORY: respiratory rate, min ventil, RBC count, erythropoietin production o CARDIO: CO (HR&SV), diastolic relaxation shortens(Ca+ sequestration), small systolic pressure, diastolic (reflects effect of SV but TPR), vasodilation (directly and partly due to CO2 and heat), myocardial Ca+ uptake and aden cycl activity, -adrenergic receptors in heart o total blood volume (activates renin/ang/ald axis), compensates by activating ANP (and ANP inhib T3/4 by TSH action in thyroid), o Hyperthyroidism- most common cause Graves disease (autoimmune antibodies against TSH receptor- mimic TSH action), next most common neoplasm (tumor) o BONE: endochondral ossification, linear growth, maturation of chondrocytes (mostly by local somatomedin production/action) o bone remodeling, IL-6 release and bone resorption, tooth development o growth of hair follicles, skin, nails o NERVOUS SYSTEM: CNS development in fetus (T4 not T3 taken up by developing brain tissue) o Enz/receptors for neurotransmitters, myelin, neurotropic factor, neuro cell adhesion molecules, prot for neuron migration o cerebral blood flow and gluc metab o energy, alertness, responsiveness, awareness of hunger, memory, learning, normal emotion o speed and amplitude of neural impulses o normal reproduct development, normal ovarian cycle, ovulation, spermatogen, maintenance of pregnancy, sex steroid bindin glob from liver, sertoli cell differn o ENDOCRINE- GH, prolactin, cortisol (and its MCR), estrogen:androgen ratio in men, PTH and vitD synth (compensate for TH effects of resorption) VI. Adrenal Glands outer zone- cortex- 85% of gland- from mesodermal- source of corticosteroid horms inner zone- medulla- 15% of gland- from neuroectodermal symp ganglia- source of catecholamine horms- cells called chromaffin cells (present in all three zones of cortex as well, and cortical cells present in medulla as single cells, rays, or islets) one of bodies highest rates of blood flow/g tissue- from aorta, renal arts, and phrenic art.blood enters cortex and drains into medullary veins (bathes medullary cells). o R. adrenal vein drains directly to inf. vena cava, L. drains to renal vein. Cortex: glucocorticoids- essential for life, CHO/prot metab, anti-inflam effects, req ketone at 3rd position, and hydroxyl groups at 11 and 21 o Cortisol o Corticosterone Mineralocorticoid- req oxygen at C18 o Aldosterone Sex steroid precursors- 2ndary sex characteristics, oxygen at C17 (C20-21 eliminated) o Androgens o Estrogens- aromatization of androgen A ring 3 zones: o Zona glomerulosa- thin outermost layer o Zona fasciculata- middle, widest zone, grows in response to ACTH o Zona reticularis- innermost zone, grows in response to ACTH Cortical Hormone Synthesis: precursor cholesterol, binds to adrenal PM receptors for LDL and HDLendocytosisesterified and storedcytochrome P-450 oxygenases catalize steroid hydoxylations for cholessteroids (NADPH transfers hydrogen to P-450 via adrenoxin reductase and adrenoxin) o Glucocorticoids- zona fasciculata Cortisol- dominant glucocorticoids (but corticosterone can compensate if cortisol prod is blocked) controlled by CRH-ACTH axis. Esterified cholesterol hydrolyzedtransported across outer mito memb (OMM) to IMM where adrenoxin awaitscholest hydroxylations and cleavage of side chainin ER to 11deoxycortisol (via 17-hydroxylase) transferred back to mitohydroxylated on C11 by 11-hydroxylase (most efficient step)cortisol diffuses out of cell (not stored) o Androgens/Estrogens- zona reticularis- ACTH regulation. Starts with 17-hydroxylated (via P-450) derivatives of pregnenolone and progesteroneremoval of C20-21 side chainvia P-450 yields DHEA and androstenedioneDHEA sulfatedDHEA-S (this and androstenedione are major precurs)converted to more active androgen testosterone and then some testosterone to active estrogen estradiol in peripheral tissues Important androgen precursors in women but little importance in men because testis produce large amounts of testost. Conversion of androgen precursors to estrogens in women not important till after ovaries stop working. Last common step in cortisol/androgen synth is 17-hydroxylation- if cortisol synth is inhib at any step after, androgens accumulate Androgens metabolized in liver to androsterone and etiocholanoloneexcreted in urine. Androsterone, etiochol, & DHEA-S leave in urine- called 17-ketosteroids o Mineralcorticoids- zona glomerulosa- aldosterone Cholestcorticosterone is same as in z. fasciculata. Corticosterone then hydroxylatealdosterone which is released ACTH regulates fasciculata and reticularis (not aldosterone from glomerulosa) o binds to PM receptor (req Ca+)Gprotaden cyc/cAMP/IP3/DAG/PKC&Aph prots o steroidogenesis activator frees cholest, sterol transfer prot moves choles to OMM, StAR (steroidogenic acute reg prot) transfers choles to IMM for P-450 action (rate lim step). All steps of corticosteroid horm synth stim by ACTH (cortisol & androgens) Cortisolo 80% circulates bound 1:1 to 2-globulin (CBG) called transcortin, other 15% to albumin, 5% free. Inflammation/leukocyte enz cleave transcortin-cortisol and increase free cortisol (HL 70min, MCR 200L/day) o cortisol equilib with cortisone its inactive analog, like a prohorm for cortisone. Interconversion via hydroxysteroid dehydrogenases (HSD)- type 1 in liver, bone, muscle, adipose, gonads. Type 2 in kidney. o Cortisol/cortisone- metabolized in liver- products excreted in urine- reliable index of cortisol secretion. Cortisol precursors progesterone and 17-hydroxyprogest. o Inhibition: Glucocorticoids- FBI on ACTH (cortisol) ANP- suppresses StAR gene o Stimulation: Night- peak just before morning (following ACTH peak), low level just before sleep- blunts CRH. Bright light lunch/OrexinA- (appetite stimulant) stim cortisol. Stress- burns, surgery, fever, exercise, etc TNF- stim ACTH/cortisol Estrogeno Cortisol Actions- catabolic, permissive- allows processes to happen (not initiate)actions req hours or days Maintains gluc production from proteins Fat metabolism CNS function Immune system Enters cell by diffusionbound to glucocort recep (GR, usually GRII except brain has GR I). (GR & GR both made but inactive- can bind to to inactivate it for control.) cortisol binds to receptorreceptor phmoves to nucGlucocortRegElements on DNAinteracts with histone acetylatorsinitiation or repression of a gene GH gene activated in AH Tyrosine aminotransferase activated in liver Represses expression of GR and induces GR for FBI MineralcortR (aka GR type I) also binds cortisol but less action Metabolic Effects- facilitate mobilization of fuels- esp mobilization and conversion of protglycogen- essential for survival of fast and starvationextends the hyperglycemia evoked by glucagon, epineph, and GH. mobilization of muscle prot for gluconeogen, inhib prot synth o plasma BCAA except alanine (directly converted to gluc) o availability of prot does synth but not as much defends against insulin hypoglycemia glucose-6-phosphatase– releases gluc from liver powerfully antagonizes insulin’s gluc storage effects o inhib insulin’s suppression of liver gluc production o inhib insulin-stimulated uptake of gluc by musc & adipose tissue responsiveness to insulin (req insulin for same effect) o eventually more insulin released due to resistance removes gluc transporters from PM to reduce gluc uptake permits lipolysis by epineph, GH, and others (RQ) o also stim lipogenisis in some areas (prolif of adipcytes) o also stim leptin- which appetite in hypoth NPY synth and its receptorsstim eating Muscle Effects: Reduces muscle mass via prot catabolism Ach, myocardial NaK+ATPase, and -adrenerg receptors which maintains contractility of muscle insulin sensitive slow oxidative type I fibers Bone Effects: bone resorption by mRNA of collagenase bone formation- via oblast and oclast GR collagen synth oblast differentiation, oblast and ocyte apoptosis (via IGFs) Ca+ absorption from intest by vitD (further bone resorp) CT Effects: collagen synth- thins skin and walls of capillaries Vascular Effects: Req to maintain BP- sustains myocard performance and allows arterioles to respond (constrict) to angiotensin II and catechols vasodilating PG maintain blood vol by perm of endothel Kidney Effects: GFR- via pre-glom resistance/glom blood flow Ca+/Pi reabsorption water excretion via inhib of ADH CNS Effects electrical activity- modulates excitability, behavior, moods o receptors in limbic system and hippocampus in excess can cause insomnia, over-elevate or depress moods, decrease memory, lower threshold for seizure. Fetal Effects Maturation of CNS Preparation of fetal lung for use at birth- alveoli develp & synth of surfractant Immune/Inflammatory Effects- net result to local immune response, but cytokines released in immune response cortisol (to control immune response so as to not over react and destroy healthy tissue) dilation of capillaries at site of injury, permeability for trapping of leukocytes at site of injury (inhibit natural immediate immune response at site of injury by inhibiting arachidonic acid production (via lipocortin which inhibits PLA2) and thus production of PGs, thromboxanes, leukotrienes, NO, platelet-activating factor) COX2 gene and NO gene (has same effect as above) tissue swelling mast cell differentiation and prolif activity of neutrophils (although it # of neutrophils) # eosinophils and Tcells (stim apoptosis) Aldosterone- sustains ECF vol by conserving Na+. daily secretion 50-250g o Juxtaglom cells sense renal blood flowsecrete reninacts on angiotensinogen from liverangiotensin IACE converts to angiotensin II (potent vasoconst)angII binds PM receptors in zona glomerulosaG-protCa+, IP3/DAG, PKCtransfer of choles to mito P-450 enzaldosterone release Release of renin by sympathetic activity via -adren receptors in kidney. PGsrenin (so COX inhibitors can inhibit aldost). FBI on juxta cells by angII Na+ and K+ also locally activate renin-ang system in adrenal gland o ANP- VolANP (all types, B from ventr and C from endoth)binds to receptors at zona glomer and inhibits aldost synth- via cAMP and cGMP (also ANP renin release) o Aldos clearance of K+ (K+ stim aldosterone secretion)- K+ depol adrenal cell membvoltage dependent Ca+ channels openIC Ca+ o ACTH acutely stim aldos secretion- but more importantly maintains a tonic role in keeping the zona glom sensitive to angII o Circulates in plasma bound to aldos-binding glob, transcortin, and albumin Binding weaker than for cortisol, HL 20min, MCR 1600L/day o Inhibit Low K+ Dopamine- via Gi cAMP o Stimulate- Low sodium- intake or plasma level- aldos response to ACTH, angio, K+ Ach VIP/PACAP- made in adrenomedullary cells Serotonin o Aldosterone Actions- binds to GR type 1 (mineralcort receptor)gene transcriptional changes (lag of 1-2hrs) Kidney is major site of action- stimulates active Na+ reabsorption from tubular urine back into peritubular caps via collecting duct cells and late distal convoluted tubule cells water passively follows (no change in [Na+]) expression of Na+ channel gene in principal cells of collect duct, # of channels in apical memb, # of thiazide sensitive Na-Cl cotransporters in apical memb of distal conv tubule cells, NaK-ATPase pumps in basal/capillary memb which pump Na+ back into plasma. K+ secretion out of tubular cell- because ATPase at cap memb brings in K+ when sending out Na+, and the tubular lumen becomes neg due to Na+ coming into cell, K+ just leaves for tubular lumen. Aldos necessary for normal small secretions of K+ even at normal Na+ levels. (aldos control of K+ slow compared to insuline & epineph stimulation of muscle K+ uptake Mg+ & H+ secretion- so aldos excess leads to alkalosis & hypertension Na+ colon absorption, K+ fecal excretion and cellular K+ uptake spironolactone- competitive inhibitor of aldos, used for hypertension Addison’s disease- distruction of adrenal cortex Adrenal Medulla- enlarged sympathetic ganglion- neuroecto cells from n crest invade glandmade of chromaffin cells innervated by symp preganglionic cholinergic nerves Chromaffin cells- granules containing catecholamine horms epineph and norep, ATP, prots, lipids, enkephalins, -endorphin, proopiomalanocortin, NPY, & chromagranin Chromaffin cell tumor- pheochromocytomaCatecholamine Synthesiso First rxn catalyzed by tyrosine hydroxylase (rate limiting step) occurs in cytoplasm. TyrosineDOPA (requires O2, cofactor, & NADPH)catecholamines inhibit this step. o DOPAdopamine (catalyzed by AA decarboxylase)dopamine taken up into granules to complete catecholamine synthesis o Dopaminenorepinepherine (catalyzed by dopamine -hydroxylase only found in granules)some norepinepherine stored in granules. o In the majority of granules, norep diffuses back into cytopl where it is methylated by a methyltrasferase and taked back into granules (req ATP & Mg+) and stored as epinephrine (the dominant adrenomedullary horm) o Inhibition Co-released chromogranin- FBI o Stimulation Symp stimulation releases catechols relieving inhib and activating tyro hydroxy ACTH- directly stim Cortisol- cortex blood bathes medulla cells- selectively stim methyltransferase, thus only epineph Danger- stress, harm, injury, fluid loss, hemorrhage, hypotention, temp extremes, hypoglycemia, exercise, etc Pregang fibers- in splanchnic nerverelease Achdepolarizes chromaffin cells by Na+ permCa+ influxgranule exocyt Catecholamine Metab- almost all the circulating epineph is from medulla, and almost all norep is from symp nerves and brain that excaped reuptake- norep does not act as endocrine but as neurotransmitter (very weak distant effects in circulation). o HL 2min. Liver/kidney MCR 2-6L/min- can increase by symp activity (FBI) o Key enzymes- chatecholamine O-methyltransferase and monamine oxidase/aldehyde oxidase Catecholamine Actionso Intracellular actions: 1, 2, 3, 1, and 2 receptors- epineph stronger on receptors, norep on (much overlap). receptors- aden cyc/cAMPPKA 2 – Gi cAMP and PKA 1- PI systemCa+, PKC downreg their receptors. Also refractoriness exists- desensitization to subsequent doses due to receptor phrenders recep inaccessible (FBI) o Metabolic actions: prevent hypoglycemia for CNS gluc production- glycogenolysis via receptors that activate same cascade as glucagon. (glycogen synthase restrained) gluconeogenesis via and in liver muscle glycogenolysis glucagon secretion insulin-mediated glucose uptake via epineph lipaseFFA and their oxidation via in exercise phosphorylasepromote glycogenolysislactate releaseliver uses lactate to make glucose BMR and thermogenesis in BAT (uncouple oxphos) o Cardiovascular effects: HR, CO via / selective arteriolar constrict- kidney, spleen, & skin- shunt blood to muscles systolic BP, diastolic stays same or decreases o Other effects GI and genitourinary activity 2 relaxation of bronchiolesimprove gas exchange 2 pupil dilation ADH release- , renin release via in kidney influx of K+ into muscle via 2 thyroid horm secretion and conversion of T4T3 via 2 Stress Response- adrenergic NS relationship with CRH-ACTH-cortisol axis o Stress activates CRH and ACTH neurons in paraventricular nuc and other adrenergic nerves in hypothalmutually reinforcing norep CRH release and CRH adrenergic discharge. o CRH and ADH stimulate ACTH plasma cortisol; adrenergic stimulationnorep and epin Together these glucose production, shift glucose utilization towards CNS. Epinephrine (with cortisol help) FFA to heart and muslces Both BP and CO Epi and CRH arousal, attention, vigilance, aggressiveness CRH in hypothal- awareness of pain, GH and gonadotropin, appetite and sexual activity- these occur because growth and reproduction are not useful during stress- reinforced by cortisol which suppresses growth and ovulation. Local immune responses to injury stimulated but if immune defense is too high and cytokines become too elevated they stimulate CRH releaseACTHcortisol which dampens immune resp. VII. The Reproductive Glands Gonads govern development, maturation, nutritional support of ind male & fmale germ cells & their successful union in reproduction; assist in early growth & development of the offspring within mother Paracrine signaling prominent Hypothal peptides that also prod within gonads and placenta. Sexual Differentiation- time btw indifferent gonadmature female/male- genotype, Gonadal sex, and genital sex (phenotype) differences Primordial germ cells generate oogonia/spermatogoniaova/sperm. 1st 5wks gestation- gonads are same, no genital tracts- Gonadal cells present: o spindle cells/coelomic epith- precurs of granulosa cell of ovarian follicle and Sertoli cells of seminef tubules- sustain germ cells to mature/guide their movement into genital duct system. o Interstitial/mesenchymal stromal cellsovarian theca cells/testicular Leydig cells- secrete androgenic horms- dev. male sex charcteristics/sperm production, female precursor for estrogen synth Genetic Sex- X-3000-4000 genes, Y-30 genes. PAR- pseudoautosomal region- tip of sex chroms short arm facilitate meiosis crossing over/xchange. o Y or its crossed over info req for testes & masculine genital pattern dev. SRY gene- on Y short arm- sex-determining region- just below PARo encodes testis-determining factor (TDF)-SOX transc factor family- Zn finger minor groove of DNA bind- bends DNA to exposeo TDF- at genital ridge initiate gonad diff to testis- relieve repression exerted by Sox-9 on programmed develpment of Sertoli/Leydigs. o X gene steroidogenic factor-1 (SF-1) necessary for adrenal steroid synth and gonadal development Induces enz of testost synth, aromatase (estradiol synth), LG gene, oxytocin, inhibin, GnRH, FSH, prolactin. Adrenocortical hypoplasia congenital (AHC) gene- on X- codes for transcrip factors for ovarian devlpment- double X (double AHC suppresses testicular dev) Gonadal Sex- 5 day blasocyst- primord germ cells differentiate- 23 days migrate from yolk sack to genital ridge to make indifferent gonad made of coelomic epithelium (precursor of granulose and Sertolis), mesenchymal stromal cells (theca/Leydig/germ cell precursor). o Primitive gonad- has cortex and medulla Male- semineferous tubules begin to form 6wks under Sox-9 influence Leydig cells appear 8wks- begins testost secretion SRY gene inhibts aromatase enz (thus inhib estrogen) Cortex regresses- medulla dominates Female- ovary appears 9wks (both X chroms active)- Germ cellsmitosisoogoniameiosis in some oogonia and they become surrounded by granulosa cells and stroma making them primary oocytesstroma gives rise to some interstitial cells Primary oocytes remain in diplotene (late prophase) unitl ovulation at puberty Cortex dominates, medulla regresses (opposite male) Estrogens block actions of available androgens Genital Sex- so far differentiation has not required hormone products o Diff of genital ducts req gonadal horms (in absence of gonadal horms, female genitals devel) o Fem- at 5wks/male- at 9wks- 2 genital ducts devel Male- mullerian ducts dissapear at 7wks when Sertoli cells arise and make Mullerian inhib factor (MIF or anti-mullerian horm AMH- activated by SF-1 and SOX-9)- AMH also organizes testis/initiates descent. Leydig cells develop and secrete testostthen the wolffian (aka mesonephric ducts) develwhich give rise to epidiymis, vas def, seminal vesicles, ejac duct (system respons for delivering sperm from testis to vag) Wolffian duct dev/diff does not req conversion of testost to dihydrotestost (DHT) Female- Mullerian ducts arise next to wolffians wolffian ducts dissapear at 10wks because no testost in absence of AMH Mullerian ducts develop- upper endsfallopian tubes, lower ends join to form uterus, cervix and upper vag (completed by 18wks- no horm/ovaries necessary) o Genitals- m and f devlp from: genital tubercle (glans/clit), genital swelling (scrotum/labia maj), genital folds (enclose urethra and corpora spongiosa/labia minora), urogenital sinus (prostate/lower vagina). Male devlpment req presence of testost converted to dihydrotestost (done by 5-reductase enz in target tissues- also converts testostandrostenediol) Female dev does not req horms(altho estradiol may oppose androgens presnt) Fetal Leydigs make testost under influence of chorionic gonadotropin (an LH) from placenta (no fetal GnRH) Last 6 mo. growth male & female genitalia does req fetal pit LH for estrogen and androgen synth (respectively) After birth constant pattern of gndtrpn release in males vs monthly cycle in females Testost suppresses breast develp Abnormalitieso Absence of testosterone/AMH leads to mullerian duct dec, female genitalia, wolffian duct regression, even in XY individuals. Testicular feminization syndrome- cannot respond to androgens due to receptor deficiency/mutation- presence of Y makes testes but no o o o o o masculinization of ext genitalia, no wolffian ducts, breasts formunopposed estrogen action (genitalia vary on degree of testost def) XY failure to convert testostDHT= ext genit variation from male to completely female (however AMH present so epididymis, vas deferns, sem ves normal. XX over produce adrenal androgens- have ovaries bc 2 XX present (with no Y), Mullerian normal (bc no AMH), variable ext genit. XXY- klinefelter’s XXX- shorter reprod life. Gene mutations- SF-1, SOX, AMH. Or duplication of AHC gene on X leads to ovaries (even in XY ind) Gonadal Function- common aspects. Both use cholesterol for precursor for steroids (same synth as adrenal glands, except more insitu cholest from acetyl-CoA used than uptake. SF-1 upregulat). Androgens precursors of estrogens- aromatization of A ring- by P-450 complex Estradiol and estrogen formed from testost and androstenedion respectively (can be interconverted) Other gonadal products: o Inhibins and activins- same growth-regulating fam as AMH. Inhibin- glycoprot- inhibits GnRH-stimulated secretion of FSH, locally inhibin stim testost prod in Leydigs Activin- opposite effect on GnRH- locally stim dev of embryonic tissues, testost o Follistatin- other FSH inhib by binding to/inactivating activin o IGF-1 (somatomedin C), and TGF and - made by Sertoli, Leydig, and granulosa cells- modulate cell growth o Proopiomelanocortin products- from Leydigs. o Oxytocin- from leydigs. o Also make ster binding prot, IGF-binding prots, proteases, PGs, cytokines, ECmatrix molec (laminin), integrins, collagens I & IV, proteoglycans Gonadotropin Actions in Gonads- LH/FSH reg gonad func, neg FB mech. Growth promoting effects, gluc oxidationvasodilation o LH- stim interstitials (Leydig/thecals) to secrete androgens (also acts on granulosas) PM receptor- G-prot/aden cyc/cAMP/Ca+/PGs and MAPKs. Continued stimulationdownreg receptor interstitial uptake of cholest and stim P-450 o FSH- acts on granulosa/Sertoli cells via PM receptcAMP aromatase transcrip (thus estr synth), inhibin synth # of granulosa cell LH receptors Age-Related Changes in Gn Secretion- GnRH present in hypoth at 4wks of gestation, pit LH/FSH at 11wks. Plasma inhibin correlates with Gn very low levels in childhood (nonreproductive state) (after infant GnRH peak, GABA, NPY, endorphins, melatonin inhib GnRH neurons). Puberty- transition to repro state. LH > FSH. Boys delayed onset. GABA inhib lifted by glutaminergic tone) o Obese pubesce earlymin fat mass necessary- leptin stim GnRH, inhib NPY o Gradual maturing of hypoth neuronsGnRHpulsatile secretion LH/FSH Month cycle in females where LH greatly exceed FSH o Nocturnal LH peak amplified (disappears in adult) o Cause testos in men and estradiol in women (FSHinhibin in both)causes 2-3x in GH pulse ampl (no change to freq)bone mass and male muscle mass Synergy of GH and testost (estradiol lack)greater musc mass GH/IGF-1 gonad growth, IGF GnRH release Aging- after 50gonad response to gonadotropins- gradual in males, females menopause (couple years) o Steroid and inhibin , so neg FBFSH >LH (rise in females) o GH/IGF-1 secretion bone/muscle, fat Germ Cell Develpo In embryo- male primordial germs- only mitosis to primitive spermatogonia, meiosis does not resume until puberty. o Female embryonic germs- mitosisoogoniameiosis1- stops in diplotene of prophaseresumes at pubertymeiosis2 stops again in metaphaseII with extrusion of 1 polar bodymeiosisII completed after fertilization and 2nd polar body extruded Testes- spermatic arteries. Semineferous tubules, CT with scattered Leydigs. Seminiferous tubules- coiled mass. Begins and ends at duct tubulus rectus which anastamose in rete testis and drain via ductuli efferentes epididymis which is storage and maturation site for spermatozoa. From epididvas deferensejac ductpenis o Semin tubules separated from Leydigs and peritubular (myeloids) by basement memb- beneath which are spermatogonia and Sertolis. Leydigs- secrete testost Spermatogonia dividespermatocytesspermatidsspermatozoa in column from b memb to lumen o Sertoli cytoplasm fuses into tight junc (blood testis barrier) that move spermatagonia/spermatocytes from basal compartmentadluminal compt (spermatids/spermatozoa) toward lumen as they dev BT barrier protects maturing sperm from substances Sertolis prolif in infancy and puberty (not after or b/w)- # of sertolis determines capacity of sperm prod. Sperm release TNF cytokine (Sert/Leydigs have recepts)- secrete inhibin in response to TNF FSH upreg androgen receptor on sertoli. FSH and testost act on sertoliandrogen binding prot (ABP- regs availability of free testost/DHT/estradiol in semin tubules) and inhibinB, activin, GFs. o Peritubular myeloid cells- secrete paracrine reg stuff, may contract tubules/vessels Spermatogenesis-200mil daily. Ea spermatagonium64 spermatozoa. No sperm without testost, low or none without FSH and LH. GH needed for timing o High testost must be present around semintubules- from LH action on Leydigscrosses basement memb to Sertolis. Prevents premature spermiation of sperm into lumen by stim cadherin prod (some testostestradiol in Leydigs and Sertolis). o Prolactin LH receptors, androgen prod. o FSH necessary (proper acrosome, motility, transcrip of CREMs, stim Sertolis) o GH- needed for timing- stim growth of wolffian duct, penis, prostate, Leydig LH response, w/IGF stim testost prod. o Stem cell renewal (mitosis)germ cell prolif (meiotic)spermiogenesis (maturation). Latter 2 phases in adluminal comptment. Last stage histones replaced with protamines (pkg DNA much smaller) o Interactive- cells in one stage can influence other stages o Extrinsic horm regulation. o Germ cell prolif- starts w/primary spermatocytessecondary spermatocytesspermatids (haploid, X or Y), lie near lumen attached to Sertolison to: o Spermiogenesis- head form, nuc condense, shrink cytop, middle piece/body (mitoch), acrosome forms, tail flagella (dynein/microtub- central pair/9surrounding pairs)emerge as spermatozoainto lumen via spermiation (most of cytoplasm rejected back into sertoli as residual body. o Spermatozoa in lumenepididymis (surrounded by contractile muscle) 3wks travel/maturation (prots in epid and semin enhance motility and stabilize sperm)vas deferens (stored up to months) Sexual Funco Erection- pudendal nerve & symp and ps nerves of pelvic n.blood fills venous sinuses of corpora cavernosa/spongiosa Pelvic symp n inihb erection- cavernosa kept closed, art constric Ps nerves art dilation, fills corpora NO and PGEcGMPrelax cavernosa o prostate secretions added (basic to neutralize vag)semin vesicle secretion added (fructose, PGs, FSH/LH, prolac, testos, estrad, inhibin, endorph, oxytoc, relaxin, etc)ejac from vas def (symp stim ishio-/bulbocavernosa musc contract o sperm need capacitation to fertilize (4-6hrs)- washed free of sem fluid, cholest removed from memb, FertPromotPeptide (from prostate)cAMPcapacitation, capacitation to keep acrosome reaction from starting early. Angiotensin/calcitonincapacit, Ca+/motility o acrosome rxn- proteolytic/hydrolytic penetration Androgen Secretion and Metabo testosDHT and androstenediol via type 1 and type 2 5-reductase & NADPH in peripheral tissues (type 2 in genital tissues- reg devlpment, downreg after puberty and type 1 takes over) androstenedione- testos precursor-also secreted from Leydigs- little activity testos high in fetus during masculinization- at birth falls (no Leydigs) puberty testos levels very high again, at 40 starts to decline every year due to reduction in GnRH and loss of Leydig responsiveness to LH 1% of testos is free, 65% bound to sex steroid-binding glob (SSBG), remaining bound to albumin- bound serves as circ resevoir. (only free and loosely albumin bound are bioactive). Thyroid horm and estrogens SSBG (akafree testos), androgens SSBG (level of free testos) o 2 estrogens- estradiol and estrone- in men almost all derived from circ testost converted in adipose and liver Androgen Action- 1)effects on reprod function and sex charactristcs 2)effects of stim growth and devlp nonreprod tissue. o Testos- diffuses freely into cellsusually converted to DHT (sometimes to androstenediol)androgen/receptor complx phosphorylated, dissociates from heatshock protsinteracts w/DNA (some assisted by transcrip factors)RNA polymerase, mRNA, prot synth Sometimes binding of androgen relieves inhib effects of receptor Receptor can also be activated by IGF-1MAPK ph Androgen downregs receptor synth in some tissues, upregs in others o Stim growth of accessory organs- hypertrophy/plasia o TGF- (repressor of prostate growth) downreg by DHT o DHT Req in fetus for diff of: genital tubercle, gen swellings, gen folds, urogen sunuspenis, scrotum, urethra, prostate (respectively) Req in puberty for: growth of scrotum & prostate (and secretions) o DHT or 5-androstenediol: Stim male pattern hair growth, beard, body hair, recession of head hair/baldness, sebaceous gland sebum secretion, acne o Testosterone: func that do not req conversion Diff of wolffian ductsepidid, vas def, seminal ves In puberty- enlargemnt of penis/seminal v, initiate linear growth and later closes epiph plates, enlrge muscle mass, oblast secretion of TGF (estradiol req for testos bone action) Enlargmnt larynx/vocal cords Initiation/maintenance of spermatogen N retention (prot anabolism) LH/FSH secretion (negFBI) circ LDL, HDL erythropoietin synth renal Na+ reabsorp sex drive/erection aggressiveness hepatic SSBG, cortisol and thyrox binding glob mammary gland growth o Estradio- mediates effects of testos (esp in hypoth, bone, reprod tract) FSH/LH (mediates testos neg fb on LH/FSH) reabsorp of reprod tract luminal fluid by efferent ductule cells to concentrate sperm o Puberty FSH Testes enlarge LHLeydigs appeartestost secretion stim GH pubic hair penis growth linear growth sperm production adult testos levels reachedclose epiphys plates, AMH (via inhib by testos) Ovaries- horm secretion to modulate dev and extrusion of ova 3 zones: o cortex- germinal epith and oocytes enclosed in follicles (stroma inbetween) o Medullao Hilum- (entry of blood vessels) and Leydig-like androgen producing cells Follicle- nutures oocyte, releases, prepares vag /falop tubes/uterus, horm support until placenta kicks in Oogenesis- primordial germ cells leave yolk sacgenital ridgeproduce 7mil oogoniasome start meiosis (primary oocytes) until after birth when all oogonia are primary oocytes (many apop to leave 2mil). o Follicles form (12wks gestation), many apop (atresia). By puberty 400,000 prim oocytes. o As a oocyte enters meiosisinduces single layer spindle cells (granulosa precurs)basal lamin forms around themprimordial follicle Primordial follicle growth ind of FSH/LH. Factors from oocyte stim granulosas which stim thecals (TGF, EGF) o 25wks- single layer cells become granulosa cells (w/gap junc) = primary follicle FSH augments prim follicle granulosa growth, and aromatase activity (progest synth) (FSH action reinforced by ing estradiol) They both stim LH receptors on granulosa cells (and theca’s)- for later stimulation of andro synth o multi layer follicle- granulosa cells secrete mucopolysaccs to form protective halo (zona pellucida)- granus have cyto processes to feed oocyte (they form sertoli like barrier) o another layer of spindle cells recruited around bas lamina to form theca interna and ganulosa cells start secreting fluid= secondary follicle (last step until puberty) o At puberty start: o Some 2ndary follicles coalesce into single antrum- full of a lot of stuff o Granulosa cells release ster horms and AMH/inhibindiffuse theca internato antrum (AMH/inhibin inhib meiosis) o Gran cells multiply to make cumulus oophorus, theca cells prolif, more spindle cells and blood vessels make theca externa (blood brings molec i.e.FSH/LH)entire new complex called graafian follicle (aka antral follicle) GH- hyperplasia of granulosas and steroid prod, growth of oocyte (these actions done by IGF-1 and 2, no follicle GH receptors) o At menses: o Single graafian selecteddominant folliclemore growthantral fluid Dominant follicle estradiol, inhibin which inhibit the other sister follicles (atresia)only 1 makes it. Dom follicle estradiol prod stim ovulatory surge of FSH/LH o Basal lamina to ovary surface rupture to release oocyte with cumulus (meiosis 1 complete)drawn into fallopian tube (1st polar body discarded)sperm fertilization completes meiosis 2 and second polar body o After ovulation: o Ruptured folliclecorpus luteum- made of granulosas, theca’s, capillaries, fibroblasts- provides gonadal steroids necessary for inplantation and maintenance until plaenta takes over (leutinization- is LH dependent- granulosas prep for horm produc/release by ER, mito, etc) o Basal lamina disappears- thecas and capillaries communicate directly with granulosascholest intake Vasc endoth GF-capillaries Prolactin LH receptors o If fert did not occur- corpus luteum regresses (luteolysis)- apoptosis, necrosis, invaded by immune cells for degradation- scar is corpus albicans If declining LH not replaced by its equivalent- HCG from placenta Menstrual Cycle: 3 phases o Follicular: onset of menst bleed. At end of luteal FSH/LH are their lowest Begins follicular- they begin to rise- cause gradual estradiol/estrone (andros low) InhibinB (from dominant follicle), inhibinA (from corpus luteum) B + estradiol FBI on pit to reduce FSH B + IGF= androgen production by theca cells (as does insulin) Follistatin inhib activin & stim progest synth Second half follicular- FSH falls, LH rises more (est levels rise sharply just before ovulation) estradiol released by dom follicle, estrone prod peripherally Progest (from adrenal cortex) low until ovulation when slow o Ovulatory: ovulation Spike in gn levels (LH more than FSH)-from dominant follicle estradiol production and action on pit/hypo (inhib of dopa/endorphinergic nerves on GnRH neurons)- then FSH/LH decline over 20hrs spike triggers ovulation (releases inhib of meiosis from AMH) also triggers PGs, TXs, leukotrinesinflam rxnrupture (plasminbreakdown of follicle wall) Estradiol plummets due to LH spike-caused downreg of LH receptorssensitivity to LHestradiol and andro Andros decrease o Luteal: ends with bleed LH/FSH still declining progest from corpus luteum estrogens to peak in middle of luteal andros continue to decline inhibinB , inhibin A A+estradiol and progest FBI on pit FSH/LH A inhib androgen synth, but offset by its stim FSH/LH receptors Gonadal Horm Effects- estradiol, estrone, other estrogens, progesteroneenter cell freely bind to estrogen receptor (ER and ER)o Ligand bindsReceptor phosphorylation occurstransfer to nucDNA RE o Also PM/MAPK-linked receptors for estrogens exist for fast nongenomic effects (ie vasodilation) o PR- progesterone receptorPRE (prog reg elemnts) on DNA o Estradiol productin of PRs and ERs (amplifies own effects on follicle growth, endometrium, and prepares tissues for progest action) o Progest ER synth i.e. inhib endometrial proliferation Uterus- house fetus- muscle lining, mucus memb endometrium- (shed at follic phase) o glands sparse/straightendo shed. estradiolendo thickness just before ovulation, glands become coiled, arteries elongate- this is proliferative phase of endometrium: telomeres repaired (inhib apop) cervix mucus more watery (not as thick-allows spermies to swim) o secretory phase: after ovulation- progestprolif, thins endomet, telomerase suppressed (apop). Luteal phase progresses Glands more torturoussecretion,arteries spiral & elongate more o Menstrual period: If no implantationcorpus luteum regressimmediateestradiol and progestcontractions of arteries and muscles, PGs, leukotrines, inflammatory rxnischemia, necrosis, shedding Menopause: o folliclesestrogens, inhibins o FSH/LH due to no FBI by inhibins and estrogens/estradiol o estrogen deficiencybreast mass, emotional lability Pregnancy: o Blastocyst implantation= adhesionpenetrationinvasion o cell surface receptors (Integrins on zygote/osteopontin from uterus) are required. zona pellucida broken down. o Trophpblasts invade between memb of endometrial cells use laminin and fibronectin (adhesion)- form decidua for source of nutrients until blood connection made. (decidua also releases prolactin, relaxin, PGs, etc). tropho and decidua directed by IGFs, TGF, EGF, cytokines. o Chorion/amnion forming Placentao Fetal lung o Fetal kidney o Fetal gut o Endocrine gland Cytotrophoblasts- like hypothal- secrete stimulatory and inhibitory hypothal-like peptides that act on: Syncytiotrophoblasts- like pit- release pituitary-like horms and synth steroid horms from precursors Horms of Pregnancy o HCG- first horm of preg- secreted by syncytiotrophos- like GnRH (reg by inhibin/activin) o Estrogens-augmented prodution in pregnancy- stim growth of uterine myometrium, breast, and along with relaxin relazes mother’s pelvic muslces and ligaments to fit fetus better o Human chorionic somatomammotropin- (aka HCS, HPL)- from syncytiotrophosregulated by GHRH and somatostain (from neighbor cytotrophoblasts)- promote anabolism- somatomedins produced in placenta in response to HCS o Prolactin- essential for mammotrophic effects of estrogen/progest- although continued progest/estrogen inhibit lactation. Prolactin depresses immune responses to fetus o Relaxin- decidual cells and corpus luteum synth this- resembles proinsulinproduction stimulated by HCG- suppresses myometrial contractions by inhib myosin LCK- softens pelvic region o Inhibins- A from fetal trophoblasts, some from corpus luteum in response to HCG- A steady in preg to inhibit mothers GSH secretion and unneeded ovarian follicle formation- A falls after delivery, B is low during preg and after delivery o Activin- stimulates HCG and progest synth by placenta, follistatin inhibits this. o Other changes insulin high- peak coincides with HCG peak- it is also high throughout pregnancy because tissue insulin sensitivity diminished aldosterone- in preg (renin, angiotensin)ECF for fetus cortisol- estrogen induced increased in CBG, but free levels rise tooleads to more fat, breast devel Thyroid horm - estrogen induced increase in TBG- free T3/4 also , (HCG induced) Maternal GH - not needed because HCG present. LH/FSH- estrogen, progest, and inhibin (first from corpus luteum, later from placenta) inhibits these Ca+ absorption - due to vitD. (PTH supressed) Lactation- drop in progest and estrog allow lactation. Acutely elevated due to suckling o Mediated by prolactin- which also suppresses reproductive function in new mother. o Prolactin LH/FSH- no menstrual cycle/reproduction needed o Dopamine neurons normally are inhibiting prolactin- inhibition lifted after pregnancy o Acts in brain to stim motherly/protective behavior, appetite o Colostrum comes first- fluid not quite milk o Milk- Ca/Ph, lactoferrin, IgA, oligosaccsprotect infant. All pituitary horms and their hypothal releasing horms, IGF, vitD, thyroid/steroid horms, PTH, PGs. o Cortisol, insulin, prolactin necessary to make milk Fetal Endocrine: o Prolactin high o HCS serves for GH o IGFs o Thyroid horm from fetal thyroid necessary after birth for normal CNS developmnt o Fetal PTH (and placental) transports Ca from mother across placental barrier to fetus o Calcitonin promotes bone formation