Oropharyngeal Candidiasis In Persons Living with HIV/AIDS
advertisement

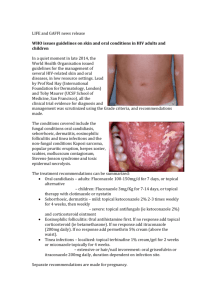
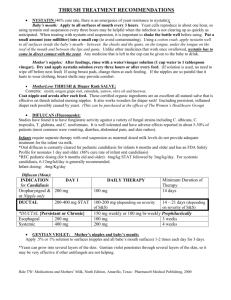
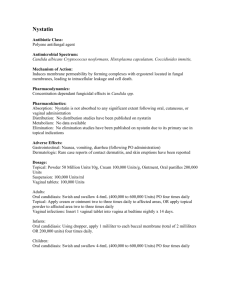
Module 6 Oropharyngeal Candidiasis in Persons Living with HIV/AIDS Oropharyngeal Candidiasis in Persons Living with HIV/AIDS David A. Reznik, D.D.S. Chief, Dental Service Grady Health System Atlanta, Georgia Angular Cheilitis • The clinical presentation of Angular cheilitis (AC) is erythema and/or fissuring of the corners of the mouth. • AC can occur with or without the presence of erythematous and/or pseudomembranous candidiasis. • Treatment involves the use of a topical antifungal cream directly applied to the affected areas four times a day for the two-week treatment period. Angular Cheilitis Angular Cheilitis • Erythematous candidiasis (EC) • EC presents as a red, flat, subtle lesion either on the dorsal surface of the tongue and/or the hard/soft palates. • EC tends to be symptomatic with patients complaining of oral burning, most frequently while eating salty or spicy foods or drinking acidic beverages. Erythematous candidiasis (EC) • Clinical diagnosis is based on appearance, taking into consideration the person’s medical history and virologic status. • The presence of fungal hyphae or blastospores can be confirmed by performing a potassium hydroxide preparation. Erythematous candidiasis (EC) Erythematous candidiasis (EC) Erythematous candidiasis (EC) • Erythematous candidiasis (EC) Pseudomembranous candidiasis (PC) • PC appears as creamy white curd-like plaques on the buccal mucosa, tongue and other oral mucosal surfaces that will wipe away, leaving a red or bleeding underlying surface. • The most common organism involved with the presentation of candidiasis is Candida albicans, however there are increasing reports of the increased incidence of non-albicans species. 1 – 1. Powderly WG, Mayer KH, Perfect JR. Diagnosis and treatment of oropharyngeal candidiasis in patients infected with HIV: a critical reassessment. AIDS Res Hum Retroviruses 1999 Nov 1;15(16):1405-12. Clinical Diagnosis of PC • The diagnosis of PC is based on clinical appearance taking into consideration the person’s medical history. • Potassium hydroxide preparation, fungal culture or biopsy, may be useful in obtaining an accurate diagnosis. Mild to Moderate Pseudomembranous Candidiasis Mild to Moderate Pseudomembranous Candidiasis Moderate to Severe Pseudomembranous Candidiasis Moderate to Severe Pseudomembranous Candidiasis Azole Resistant Pseudomembranous Candidiasis (C. albicans) Azole Resistant Pseudomembranous Candidiasis (C. glabrata) Trends in Candidiasis in the HAART-Era • There has been a decline in the occurrence of PC in patients who are on successful highly active retroviral regimens containing protease inhibitors 2 • A review of the literature suggests that immune reconstruction alone does not account for this reduction, but rather the added effect of protease inhibitors on candidal virulence factors such as aspartyl protease.3 2 Patton LL, McKaig R, Straauss R, Rogers D, Enron JJ Jr. Changing prevalence of oral manifestations of human immunodeficiency virus in the era of protease inhibitor therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:299-304. 3 Cauda, R, Tacconelli E, Tumbarello M, Morace G, De Bernardis F, Torosantucci A, Cassone A. Role of protease inhibitors in preventing recurrent oral candidosis in patients with HIV infection: a prospective case-control study. J Acquir Defic Syndr Hum Retrovirl, Vol 21(1), May 99. Treatment of Candidiasis • Treatment should be based on the extent of the infection with topical therapies (nystatin, clotrimazole) utilized for mild to moderate cases and systemic therapies (fluconazole) used for moderate to severe presentations. • Antifungal therapy should last for two weeks to reduce the colony forming units to the lowest level possible to prevent recurrence. Azole Resistance • As HIV disease progresses and immunosuppression becomes more severe, the incidence and severity of oropharyngeal candidiasis increase. The introduction of oral azoles, most notably fluconazole, has led to the increased incidence of azole resistant Candida albicans as well as the emergence of nonalbicans species such as Candida glabrata, which are inherently resistant to this class of drug1 Azole Resistance • Factors that increase the probability of azole resistant strains of Candida presenting in the oral cavity include previous exposure to azoles, low CD4 count and the presence of nonalbicans species.4,5 • To minimize the risk of resistance, topical therapies should be considered for first-line treatment of initial or recurrent cases of mild to moderate oropharyngeal candidiasis.1 4. Maenza JR, Keruly JC, Moore RD, Chaisson RE, Merz WG, Gallant JE. Risk factors for fluconazole-resistant candidiasis in human immunodeficiency virus-infected patients. J Infect Dis 1996 Jan;173(1):219-25 5. Cartledge JD, Midgley J, Gazzard BG. Non-albicans oral candidosis in HIV-positive patients. J Antimicrob Chemother 1999 Mar;43(3):419-22. Available Medications Used in the Management of OPC • Topical agents Clotrimazole troches 10 mg: Dispense 70, dissolve one troche in mouth 5 times a day for 14 days Nystatin oral suspension 500,000 units: Swish 5 mls in mouth as long as possible then swallow, 4 times a day for 14 days Nystatin pastilles 100,000 units: dispense 56, dissolve 1 in mouth 4 times a day for 14 days Available Medications Used in the Management of OPC • Systemic agents Fluconazole 100mg: dispense 15 tablets, take 2 tablets on day 1 followed by 1 tablet a day for the remainder of the 14 day treatment period Itraconazole oral suspension 10mg/10ml: dispense 140ml, swish and swallow 10ml per day for 7 to 14 days. Take medication without food. Efficacy of antifungal drugs used in the treatment of OPC in HIV+ Patients • Limitations in published literature HIV disease status (CD4 count, viral load ) not reported in ~ 1/2 of the studies Antiretroviral therapy reported in only 2 studies, none involving HAART or protease inhibitors Compliance with prescribed drug therapy not universally assessed Speciation of candidal organisms in treatment failures was rare; drug susceptibility testing not performed Cost-effectiveness analysis not performed Efficacy of topical antifungal therapies • Clinical trials have not been undertaken which compare the efficacy of the two most frequently prescribed topical antifungal medications used in the management of OPC in HIV+ individuals nystatin oral suspension clotrimazole troches • The only comparison which can be referenced include two studies which were designed to look at the efficacy of two different formulations of fluconazole. Selected studies involving topical antifungal therapies • Pons et al, 1993, Fluconazole (100 mg) once daily for 14 days vs Clotrimazole 10 mg troche 5 X daily for 14 days 98% C. albicans at baseline 334 enrolled, 288 evaluated for efficacy Fluconazole arm: 91% complete clinical response: 7% clinical improvement Clotrimazole arm: 85% complete clinical response: 9% clinical improvement Difference in clinical response: Group 1 vs 2 p= ns Selected studies involving topical antifungal therapies • Pons et al, 1997, Fluconazole liquid suspension 100 mg 1X daily for 14 days vs nystatin oral suspension 500,000 Units 4 X daily for 14 days 95% C. albicans at baseline 167 enrolled, 138 evaluated for efficacy Fluconazole suspension arm: 87% complete cure, 12% improvement Nystatin liquid arm: 52% complete cure, 16% improvement Difference in clinical response: P < .001 Conclusions • Oropharyngeal candidiasis is still a common oral opportunistic infection 2 • Judicious use of systemic antifungal therapies is warranted. 1 2.Patton LL, McKaig R, Straauss R, Rogers D, Enron JJ Jr. Changing prevalence of oral manifestations of human immunodeficiency virus in the era of protease inhibitor therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:299-304 1.Powderly WG, Mayer KH, Perfect JR. Diagnosis and treatment of oropharyngeal candidiasis in patients infected with HIV: a critical reassessment. AIDS Res Hum Retroviruses 1999 Nov 1;15(16):1405-12. Conclusions • There is an increased incidence in fluconazole refractory oropharyngeal candidiasis 4,5 • Factors which lead to resistance include previous exposure to systemic azoles and low CD4 counts 4 4.Maenza JR, Keruly JC, Moore RD, Chaisson RE, Merz WG, Gallant JE. Risk factors for fluconazole-resistant candidiasis in human immunodeficiency virus-infected patients. J Infect Dis 1996 Jan;173(1):219-25 5.Cartledge JD, Midgley J, Gazzard BG. Non-albicans oral candidosis in HIV-positive patients. J Antimicrob Chemother 1999 Mar;43(3):419-22