Candidiasis - UCLA Oral Medicine
advertisement
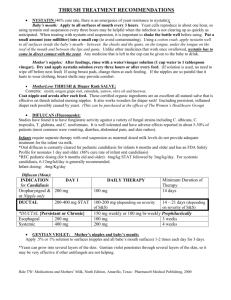
CANDIDIASIS By: Sanam Soroudi Michelle Duong Bryan Houlberg Colby Smith Candida is Present in Everyone Normally resides in the skin, mouth, GI tract, and vagina Overgrowth is prevented by other microorganisms Carriers experience few or no symptoms At least 75% of all women will experience Candidiasis at some point in their lives Clinical Features Acute Pseudomembranous Candidiasis (Thrush): – White, cheesy, creamy, loose patches that can be easily rubbed off. – Underlying mucosa is erythematous and easily bleeds. Clinical Features Chronic Hyperplastic Candidiasis – White plaque that does not rub off – Commonly found on buccal mucosa along occlusal line in V-shape and widening as it approaches commissure. Clinical Features Atrophic (Erythematous) Candidiasis – Smooth and flat, red and raw. Generalized red area of atrophic tissue. – Common on hard and soft palate due to ill fitting dentures; or dorsum of tongue. Diagnostic Testing Generally diagnosed by clinical appearance Culture – Usually swab lesion and grow on agar medium Superficial Smear w/ PAS Staining Diagnostic Testing Barium Swallow – Pt swallows thick Barium mixture, take radiograph – For visualizing esophageal candidiasis Newer Diagnostic Avenues PCR Monoclonal Antibody Rapid Latex Agglutination (RLA) Many Factors Can Cause Candidiasis Increased incidence with: – – – – Diabetes Mellitus Immuno-compromised Pregnancy Burn patients Other causes: – – – – Oral contraceptives Antibiotics Sexually transmitted Hormone replacement therapy Pathogenesis 1 Adhesion is an important determinant of Candida’s virulence – Candida produces a large number of adhesins that mediate adherence to host epithelial and endothelial cells – Strains with faulty adhesins are avirulent Pathogenesis 2 Candida produces many enzymes that contribute to its pathogenicity – Produces 9 proteinases involved in invasion of tissues by degredation of extracellular matrix proteins – Produces adenosine which blocks neutrophil degranulation, thus impairing phagocytosis Pathogenesis 3 Candida adapts rapidly to changes in host environment – Shifts between phenotypes in a reversible and random fashion – Produces genetically altered variants at a high rate – This adaptation makes it difficult for host defenses to attack and eliminate infection Histology ACUTE: -Neutrophils in the Stratum Corneum is characteristic -Diffuse inflammatory infiltrates -Fungal elements are sparse CHRONIC: -Hyperkeratosis and pseudoepitheliomatous hyperplasia -Compact orthokeratosis -Spores and hyphae are identifiable -Ill-defined granulomas Treatment ANTI-FUNGALS: -Topical- localized candidiasis in patients with normal immune function. -Systemic- disseminated disease or in patients that are immune-compromised Medications Nystatin (swish and swallow) Clotrimazole (troche) -Topical treatment for Pseudomembranous Candidiasis and Chronic Hyperplastic Candidiasis Ketoconazole Fluconazole Itraconazole -Systemic tablets for treatment of Pseudomembranous and Chronic Hyperplastic Candidiasis. Nystatin ointment Miconazole, Clotrimazole, Ketoconazole creams -Treatment of Chronic Atrophic Candidiasis Amphotercin B -Treatment of invasive Candidiasis Multiple Choice Questions Which of the following is NOT an appropriate treatment for Oral Candidiasis? a. Ketoconazole b. Nystatin c. Penicillin d. Clotrimazole Multiple Choice Question 2 A fungal infection characterized by white lesions that rub off is: a. b. c. d. Acute Pseudomembranous Candidiasis Histoplasmosis Chronic Hyperplastic Candidiasis Coccidiomycosis