oral microbiology - fungal diseases

ORAL FUNGAL INFECTION
Dr. Saleem Shaikh
COMMON FUNGAL INFECTIONS
• Candidiasis
• Histoplasmosis [Darlings disease] – Common lung
• Blastomycosis [Gilchrists disease; north american blastomycosis]
• Paracoccidioidomycosis [Lutz disease; south american blastomycosis]
• Coccidioidomycosis
• Cryptococcosis
• Zygomycosis [Mucormycosis]
• Infection with the yeast like fungal organism Candida albicans is termed as candidiasis
• A thin-walled dimorphic fungus
• Morphogenesis
• Unicellular yeast (harmless)
• Filamentous/hyphal (pathogenic)
• Strict aerobe, favors moist surfaces
• Commensally found in gut, genitals, and lungs
• Older name for this disease is “moniliasis”; derived from the archaic designation
Monilia albicans
• Other members of the Candida genus, found intraorally
• C. Tropicalis
• C. Krusei
• C. Parapsilosis
• C. Stellatoidea
• C. Glabrata
VIRULENCE FACTORS:
Adherence: change in morphology from yeast form to filamentous form promotes its adherence;
Evasion of Host defenses: exposure to various environments makes the candida to change its gene expression which in turn effects its surface antigenicity, drug susceptibility, resistance to phagocytosis etc.
Invasion and destruction of host tissue: it causes the release of hydrolytic enzymes into the local environment which promotes its invasion.
• The most common oral fungal infection in humans and has a variety of clinical manifestations
• Component of the normal oral microflora
• Factors affecting clinical outcome of infection are:
• The immune status of the host
• The oral mucosal environment
• The strain of C. albicans
• Was considered to be only an opportunistic infection
• May also develop in people who are otherwise healthy.
• May range from mild, superficial mucosal involvement seen in most patients to fatal, disseminated disease in severely immuno-compromised patients
Classification of Oral Candidiasis
Acute
Acute pseudomembranous candidiasis
Acute atrophic candidiasis
Chronic
Chronic hyperplastic candidiasis (candidal leakoplakia).
Chronic atrophic candidiasis
Central Papillary Atrophy Of The Tongue
Angular Cheilitis
Denture stomatitis
Chronic mucocutaneous candidiasis
Chronic familial mucocutaneous candidiasis
Chronic localized mucocutaneous candidiasis
Candidiasis endocrinopathy syndrome
Chronic diffuse mucocutaneous candidiasis
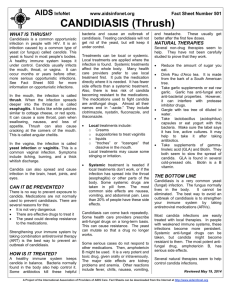
Acute Pseudomembranous Candidiasis
• Best recognized form
• Also known as “ Thrush ”
• Characterized by the presence of adherent white plaques that resemble cottage cheese or curdled milk on the oral mucosa which are composed of tangled masses of hyphae, yeasts, desquamated epithelial cells, and debris.
• Easily Scraped off with a dry gauze sponge.
• The underlying mucosa may appear normal or erythematous.
• May be initiated by exposure of the patient to broad-spectrum antibiotics (thus eliminating competing bacteria) or by impairment of the patient's immune system.
• Symptoms are relatively mild
• Burning sensation , Unpleasant taste (salty or bitter), blisters (elevated plaques rather than true vesicles).
• The plaques are characteristically distributed on the buccal mucosa, palate, and dorsal tongue.
Acute atrophic candidiasis / Antibiotic Sore Mouth
• Typically follows a course of broad-spectrum antibiotics.
• Patients often complain that their mouth feels as if a hot beverage had scalded it.
• Burning sensation is usually accompanied by a diffuse loss of the filiform papillae of the dorsal tongue, resulting in a reddened, “bald” appearance of the tongue
• Other forms of erythematous candidiasis are usually asymptomatic and chronic.
Chronic Atrophic Candidiasis / Central Papillary Atrophy Of The
Tongue
• Thought to be a developmental defect of the tongue
• Consistent relationship between the lesion and C. albicans
• Some patients with central papillary atrophy may also exhibit signs of oral mucosal candidal infection at other sites. This presentation of erythematous candidiasis has been termed Chronic Multifocal Candidiasis
• In addition to the dorsal tongue, the sites that show involvement include the junction of the hard and soft palate and the angles of the mouth. The palatal lesion appears as an erythematous area that, when the tongue is at rest, contacts the dorsal tongue lesion, resulting in what is called a “ kissing lesion ” because of the intimate proximity of the involved areas
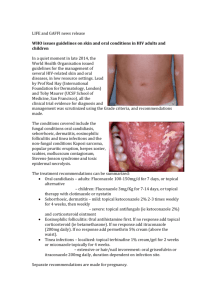
ANGULAR CHEILITIS [PERLECHE]
• Candidal involvement of the angles of the mouth
• Characterized by erythema, fissuring, and scaling.
• Often occurs alone/ as a component of chronic multifocal candidiasis
• Typically seen in an older person with reduced vertical dimension of occlusion and accentuated folds at the corners of the mouth.
• Saliva tends to pool in these areas, keeping them moist and thus favoring a yeast infection.
• Severity of the lesions waxes and wanes.
• Cases are caused C. albicans alone, combined infection Staphylococcus aureus
or S. aureus alone
• Cheilocandidiasis : Candidal infection which more extensively involves the perioral skin, usually secondary to actions that keep the skin moist (e.g., chronic lip licking, thumb sucking)
Denture stomatitis / chronic atrophic candidiasis
It is a form of erythematous candidiasis, localized to the denture-bearing areas of a maxillary removable dental prosthesis.
Characterized by varying degrees of erythema, sometimes accompanied by petechial hemorrhage.
Rarely symptomatic.
Seen in persons who wears the denture continuously.
Should rule out the allergy to denture base material
DIAGNOSIS AND TREATMENT
• Diagnosis is often made on the basis of clinical findings but sometimes microbial specimens may be obtained to identify and quantify the candida species – culture from whole saliva, swab, smear, imprint culture, biopsy.
• Mangement – Correction of predisposing host factors
Antifungal intervention: Nystatin, Amphotercin, fluconazole etc.