The Player, The Doctor, The Business
advertisement

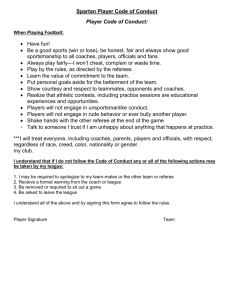
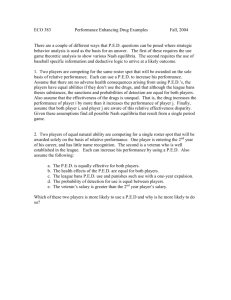
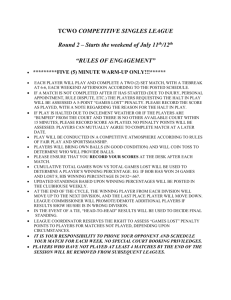
THE PLAYER, THE DOCTOR, THE BUSINESS: MEDICAL ETHICS IN PROFESSIONAL FOOTBALL MAJ Ryan Labio, Capt Marc Orcutt, MAJ Bob Plotts Faculty: Dr. Karin Zucker, Dr. Scott Kruse Army - Baylor Graduate Program in Health and Business Administration Bryan Christie Design; Purdue University “The same ethical principles that apply to the practice of medicine shall apply to sport medicine...Never impose your authority in a way that impinges on the individual right of the athlete to make his/her own decision.” The International Federation of Sports Medicine's (FIMS) code of ethics (1994). “It is the responsibility of the sports medicine physician to determine whether the injured athletes should continue training or participate in competition” (FIMS 2009). BACKGROUND 2009 Team Physician Considerations Professional football, a billion dollar industry, is widely recognized as the most popular and successful sport in America. Recent traumatic brain injury (TBI) research has prompted increased scrutiny of the health risks of football. Advances in neuro-imaging capabilities have raised new ethical considerations involving return-toplay decisions. The athlete, physician, team, and league all face complex and conflicting choices which affect ethical behavior, player health, and financial viability. ETHICAL ISSUES http://ergooccmed.com/uncategorized/419/ Should continued employment depend on the success of the team? Conflicts of interest exist between shortterm success and long-term health risks of the player. How do physicians balance the responsibility to disclose information to coaches and management? How do team physicians earn the trust of both the players and management? the year the NFL adopted a more stringent concussion policy, including provisions to remove players from games and to require medical clearance by both the team physician and an independent physician 6.4 number of missed days after a concussion in 2009 16 number of missed days after a concussion in 2012 6 number of years of an average player’s career $118,750 average player’s salary per game How much autonomy should a player have in deciding if he can play, especially if his cognition is impaired? 52 percentage of NFL players who would try to conceal Will improved imaging technologies aid treatment or inhibit provider discretion and player autonomy? $286,000,000 average NFL team’s revenue per year Does a lack of evidence based clinical guidelines for treating concussions create an ethical dilemma when considering new treatment options in a win-at-allcosts professional sport environment? a concussion rather than risk being pulled from the game 4 former NFL players have a 4 times higher chance of being diagnosed with Alzheimer Disease or ALS than a member of the general population 4,500+ Player Considerations http://nesn.com/2009/12/biggest-challenge-for-nfls-concussion-policy-is-changing-attitudes/ Are strict return-to-play protocols paternalistic? Do they limit the autonomy of the athlete to refuse treatment? Will athletes mask TBI symptoms in order to return to play? To what degree does loyalty and concern for one’s personal reputation and job security influence a player’s decision making? is the number of former players claiming the NFL withheld information about the effects of head trauma Owners of Teams and League Considerations theadvocate.com Owners of teams run a business. To what degree do explicit and implicit coercion influence team physicians, coaches, and athletes to win at all costs? How do owners mitigate conflicts of interest between protecting assets (players) and providing a quality product by ensuring the best players are on the field? Will players intentionally establish lower baselines in the preseason to game neuropsychological testing? How does the cost of injury prevention vs. the cost of long-term morbidities influence league decisions? As imaging technology advances and athletes are sidelined more frequently, will self-reporting decline? How will the TBI litigation by former players affect the future of the league? ($765-$914 million) Will more studies linking TBI to neurodegenerative processes influence the decisions of players? Should the league or owners be liable when the players choose to engage in a dangerous sport? CONCLUSION Interest in players’ safety will continue to drive scrutiny and ethical debate in professional football. Advances in neuro-imaging have the potential to alter current concussion protocols and return-to-play decisions. Players, physicians, and owners have much at stake. DISCLAIMER AND REFERENCES This poster was approved for general release by the Operations Security Officer and the Public Affairs Officer of the AMEDD Center and School, Ft. Sam Houston, TX. The views expressed hereon are those of the authors only and do not reflect policy of the Army Baylor Graduate Program in Health and Business Administration, the Department of the Army, the Department of the Air Force, or the Department of Defense. References are available on request.