increasing water loss in urine
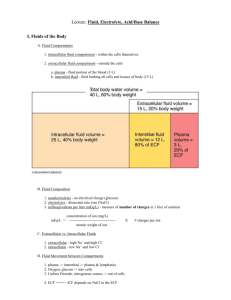
advertisement

HUMAN RENAL SYSTEM PHYSIOLOGY Lecture 7,8 BY: LECT. DR. ZAINAB AL -AMILY objectives Describe urea handling in the nephron Describe Ca handling in the nephron Describe regulation of body fluid osmolarity Describe pathophysiology of ADH secretion Describe renal mechanisms for excreting concentrated or diluted Urine: The Countercurrent Mechanism: Regulation of body sodium content by the kidney Because Na ion is the most abundant cation in the ECF, and that Na+ salts accounts for over 90% of the osmotically active solutes in the plasma and ISF. So, the amount of Na ions is the prime determinant of the ECF volume. Na+ is filtered in large amount, but normally(96%99%) of the filtered Na is reabsorbed. Through the effect of regulatory mechanisms the amount of Na excreted is adjusted to equal the amount of ingested over a wide range of dietary intake and the individual stays in Na+ balance. An increase in Na+ ingestion in the diet will result in an increase in body fluid osmolarity, which will act through the thirst mechanism to increase the water intake. The action of ADH will result in increased reabsorption of water by the kidneys that will bring back the body fluid osmolarity towards normal. These changes causing increased body fluid volume , hence increased venous return, cardiac output and BP. These changes are sensed by the baroreceptors causing increased discharge that will result in generalized vasodilatation. The afferent arteriolar vasodilatation will result in increased hydrostatic pressure within the glomerular capillaries leading to raised GFR and increased loss of Na+ and water. Other regulatory mechanism by the kidneys is by regulation of Na+ excretion through a decrease in the level circulating aldosterone. Increased BP will inhibit renin secretion by juxtaglomerular cells in the walls of afferent arterioles resulting in a fall in the circulating level of angiotensin II causing a decline in the circulating aldosterone level, then a decreased reabsorption of Na+ and water by the tubules Urea is freely filtered across the glomerular capillaries, and the concentration in the initial filtrate is identical to that in blood (i.e., initially, there is no concentration difference or driving force for urea reabsorption). as water is reabsorbed along the nephron, the urea concentration in tubular fluid increases, creating a driving force for passive urea reabsorption. Therefore, urea reabsorption generally follows the same pattern as water reabsorption— the greater the water reabsorption, the greater the urea reabsorption and the lower the urea excretion. In the proximal tubule, 50% of the filtered urea is reabsorbed by simple diffusion. As water is reabsorbed in the proximal tubule, urea lags slightly behind, causing the urea concentration in the tubular lumen to become slightly higher than the urea concentration in blood; this concentration difference then drives passive urea reabsorption, thus 50% remains in the lumen In the thin descending limb of Henle’s loop, urea is secreted there is a high concentration of urea in the interstitial fluid of the inner medulla. The thin descending limb of Henle’s loop passes through the inner medulla, and urea diffuses from high concentration in the interstitial fluid into the lumen of the nephron. More urea is secreted into the thin descending limbs than was reabsorbed in the proximal tubule; thus, at the bend of the loop of Henle, 110% of the filtered load of urea is present. The thick ascending limb of Henle, distal tubule, and cortical and outer medullary collecting ducts are impermeable to urea, thus no urea transport occurs in these segments. in the presence of antidiuretic hormone (ADH), water is reabsorbed in the late distal tubule and the cortical and outer medullary collecting ducts— consequently ,in these segments, urea is “left behind,” and the urea concentration of the tubular fluid becomes quite high. In the inner medullary collecting ducts, there is a specific transporter for the facilitated diffusion of urea (urea transporter 1, UT1), which is activated by ADH. Thus, in the presence of ADH, urea is reabsorbed by UT1, moving down its concentration gradient from the lumen into the interstitial fluid of the inner medulla. In the presence of ADH, approximately 70% of the filtered urea is reabsorbed by UT1, leaving 40% of the filtered urea to be excreted in the urine. The urea that is reabsorbed into the inner medulla contributes to the corticopapillary osmotic gradient in a process called urea recycling Calcium (Ca2) most of the body’s calcium (Ca2) is contained in bone (99%). The remaining 1% is present in ICF (mostly in bound form) and in ECF. The total Ca2 concentration in plasma is 5 mEq/L or 10 mg/ dL. Of the total plasma Ca2 , 40% is bound to plasma proteins, 10% is bound to other anions such as phosphate and citrate, and 50% is in the free, ionized form. The plasma Ca2 concentration is regulated by PTH Filtration of Ca2 differs from Na at the filtration step. Any Ca2 bound to plasma proteins (i.e., 40% of the total Ca2) cannot be filtered across glomerular capillaries; therefore, only 60% is ultrafilterable The pattern of Ca2 reabsorption along the nephron is quite similar to the pattern for Na reabsorption Like Na, over 99% of the filtered Ca2 is reabsorbed, leaving less than 1% to be excreted. Ca2 reabsorption is tightly coupled to Na reabsorption in the proximal tubule and loop of Henle, and only in the distal tubule is the reabsorption of the two ions dissociated. the distal tubule is the site of regulation of Ca2 reabsorption. The following three points concerning regulation in the distal tubule are : (1) The distal tubule is the only nephron segment in which Ca2 reabsorption is not coupled directly to Na reabsorption. (2) In the distal tubule, PTH(parathyroid hormone)secreted from parathyroid gland increases Ca2 reabsorption via a basolateral receptor, activation of adenylyl cyclase, This action of PTH on the distal tubules called its hypocalciuric action. Thus, PTH has two effects on the nephron, both of which are mediated by cAMP: a phosphaturic action in the proximal tubule, and a hypocalciuric action in the distal tubule. (3) Because of the uncoupling of distal Ca2 and Na reabsorption, the effect of thiazide diuretics on Ca2 reabsorption differs entirely from the effects of diuretics that act in the proximal tubule or thick ascending limb. Thiazide diuretics increase Ca2 reabsorption, while the other classes of diuretics decrease it. Mg2+ competes with Ca2+ for reabsorption in the thick ascending limb, hypermagnesemia will cause hypercalciuric action Which of the following would produce an increase in the reabsorption of isosmotic fluid in the proximal tubule? (A) Increased filtration fraction (B) Extracellular fluid (ECF) volume expansion (C) Decreased peritubular capillary protein concentration (D) Increased peritubular capillary hydrostatic pressure (E) Oxygen deprivation REGULATION OF BODY FLUID OSMOLARITY The regulation of body fluid osmolarity is best illustrated by two commonplace examples. The first example is the body’s response to water deprivation; The second is the body’s response to drinking water. Response to Water Deprivation 1. Water is continuously lost from the body in sweat and in water vapor from the mouth and nose (called insensible water loss). If this water is not replaced by drinking water, then plasma osmolarity increases 2.The increase in osmolarity stimulates osmoreceptors in the anterior hypothalamus, which are exquisitely sensitive and are stimulated by increases in osmolarity of less than 1 mOsm/L. 3. Stimulation of the hypothalamic osmoreceptors has two effects. It stimulates thirst, which drives drinking behavior. It also stimulates secretion of ADH from the posterior pituitary gland. 4. The posterior pituitary gland secretes ADH. ADH circulates in the blood to the kidneys, where it produces an increase in water permeability of the principal cells of the late distal tubule and collecting duct. 5. The increase in water permeability results in increased water reabsorption (5a) in the late distal tubule and collecting ducts. As more water is reabsorbed by these segments, urine osmolarity increases and urine volume decreases (5b). 6. Increased water reabsorption means that more water is returned to the body fluids. Coupled with increased thirst and drinking behavior, plasma osmolarity is decreased, back toward the normal value. Response to Water Drinking When a person drinks water, the ingested water is distributed throughout the body fluids. Since the amount of solute in the body is unchanged, the added water will dilute the body fluids and cause a decrease in plasma osmolarity. 2. The decrease in plasma osmolarity inhibits osmoreceptors in the anterior hypothalamus. 3. Inhibition of the osmoreceptors has two effects. It decreases thirst and suppresses water drinking behavior. It also inhibits secretion of ADH from the posterior pituitary gland. 4.When ADH secretion is inhibited, circulating levels of ADH are reduced, and less ADH is delivered to the kidneys. As a result of the lower ADH levels, there is a decrease in water permeability of the principal cells of the late distal tubule and collecting ducts. 5. The decrease in water permeability results in decreased water reabsorption by the late distal tubule and collecting ducts (5a). The water that is not reabsorbed by these segments is excreted, decreasing urine osmolarity and increasing urine volume (5b). 6. Since less water is reabsorbed, less water is returned to the circulation. Coupled with the inhibition of thirst and the suppression of water drinking, plasma osmolarity increases back toward the normal value. Decreased plasma osmolality and hypovolaemia. Would you see: (T or F) A. Decreased urine output B. Increased urine output C. Decreased ADH secretion D. Increased Renin –Angiotensin- Aldosterone secretion E. No change in urine output Diabetes insipidus (DI) Caused by a deficiency of or a decreased response to ADH. Two types of DI Central “neurogenic” DI Defect in the synthesis or release of ADH Nephrogenic DI Kidneys do not respond to ADH. SIADH (syndrome inapproperiate antidiuretic hormone secretion): the body secretes ADH when it shouldn't. Thus, water is retained when it should be excreted. This often leads to electrolyte disturbances (such as sodium levels). Causes: include head injury/trauma, meningitis, cancer (especially lung cancer), some infections and some drugs. Choose the appropriate nephron site in the diagram In a patient with severe central diabetes insipidus caused by a lack of antidiuretic hormone secretion, which part of the tubule would have the lowest tubular fluid osmolarity? In a person on a very low potassium diet, which part of the nephron would be expected to reabsorb the most potassium? Which part of the nephron normally reabsorbs the most water? In a normally functioning kidney, which part of the tubule has the lowest permeability to water during antidiuresis? Hyponatremia Na+ concentration below 135 mEq/L (135 mmol/L). 1) 1) Hypertonic (translocational): i. results from an osmotic shift of water from ICF to ECF, such as occurs with hyperglycemia Na+ becomes diluted. 2) Hypotonic (dilutional): I. most common form II. caused by water retention and characterized by a decrease in serum osmolality. Hypernatremia Serum Na+ level above 145 mEq/L Serum osmolality greater than 295 mOsm/kg. Na+ is functionally an impermeable solute contributes to the tonicity and movement of water across cell membranes. Hypernatremia is characterized by hypertonicity of the ECF and almost always causes cellular dehydration. Hypernatremia represents a deficit of water in relation to the body’s Na+ levels. Hypokalemia Refers to a serum K+ level below 3.5 mEq/L. Causes: i. ii. iii. iv. v. vi. vii. viii. ix. Shift of K+ from ECF into ICF (insulin & β-adrenergic agonist drugs). Metabolic alkalosis Mg2+ depletion (ICF ) Trauma and stress Hyperaldosteronism Vomiting Heavy perspiration Diuretics like thiazide and loop diuretics. Burns Extracellular-Intracellular Shifts Movement of K+ between the ECF and ICF K+ to move into body cells when serum levels are high and move out when serum levels are low. Factors that alter K+ distribution between the ECF and ICF are: A.Insulin increases cellular uptake of K+ after a meal. B. β-adrenergic (e.g., epinephrine) stimulation facilitate K+ movement into muscle tissue during periods of physiologic stress. Extracellular-Intracellular Shifts C. Serum osmolality: When increased because of the presence of impermeable solutes such as glucose (without insulin), water leaves the cell produces an increase in intracellular K+, causing it to move out of the cell into the ECF. D. Acid-base disorders. In metabolic acidosis, H+ move into body cells for buffering causes K+ to leave the cells and move into the ECF. Metabolic alkalosis has the opposite effect. Extracellular-Intracellular Shifts Exercise can also produce compartmental shifts in K+. Repeated muscle contraction releases K+ into the ECF. Although the increase usually is small with modest exercise, it can be considerable during exhaustive exercise. Hyperkalemia An increase in serum levels of K+ > 5.0 mEq/L. Causes: i. Hypoaldosteronism ii. Renal failure & hyperkalemia iii. Excessive IV fluid administration iv. Excessive hemolysis large amount of K+ release from the RBCs v. Drugs like K+ -sparing diuretics and ACEI At which nephron site is the tubular fluid/plasma (TF/P) osmolarity lowest in a person who has been deprived of water? (A) Site A (B) Site B (C) Site C (D) Site D (E) Site E At which nephron site is the tubular fluid inulin concentration highest during antidiures is? (A) Site A (B) Site B (C) Site C (D) Site D (E) Site E Renal Mechanisms for Excreting Concentrated or Diluted Urine: The Countercurrent Mechanism: The ability of the kidneys to excrete concentrated urine (than plasma) is essential for survival of mammals living on land. It depends upon the maintenance of a gradient of increasing osmolarity along the medullary pyramids. This gradient is produced by the operation of the loops of Henle as “countercurrent multipliers” and is maintained by the operation of vasa recta as “countercurrent exchangers”. There are important facts about the countercurrent system within the kidneys: 1. A countercurrent system is a system, in which the inflow runs parallel to, in close proximity to and in opposite direction to the outflow; which is the case for both the loop of Henle and vasa recta in the renal medulla. 2. There is an osmotic pressure gradient from the cortico-medullary junction to the tips of the medullary pyramids (which is made up of Na+, Cl¯ and urea), The longer the medullary depth, the greater the length of the loops of Henle, the higher the osmotic pressure gradient that can be reached at the tip of the pyramid; which means more chances to excrete a concentrated urine. . 3..a high level of ADH is another basic requirement for forming concentrated urine. The operation of each loop of Henle as a countercurrent multiplier depends on the active transport of Na+ and, Cl¯ out of its thick ascending limb, due to the presence of (Na+–K+–2Cl¯) exchanger proteins. This creates an osmotic pressure gradient between the fluid in the ascending limb and the medullary interstitium. Urea Recycling Urea recycling from the inner medullary collecting ducts is the second process that contributes to the establishment of the corticopapillary osmotic gradient. 1. In the cortical and outer medullary collecting ducts, ADH increases water permeability, but it does not increase urea permeability. As a result, water is reabsorbed from the cortical and outer medullary collecting ducts, but urea remains behind in the tubular fluid. 2. This differential effect of ADH on water and urea permeability in cortical and outer medullary collecting ducts causes the urea concentration of tubular fluid to increase. 3. In the inner medullary collecting ducts, ADH increases water permeability and it increases the transporter for facilitated diffusion of urea, UT1 (in contrast to its effect on only water permeability in cortical and outer medullary collecting ducts). 4. Since the urea concentration of tubular fluid has been elevated by reabsorption of water in the cortical and outer medullary collecting ducts, a large concentration gradient has been created for urea. In the presence of ADH, the inner medullary collecting ducts can transport urea, and urea diffuses down its concentration gradient into the interstitial fluid. Urea that would have otherwise been excreted is recycled into the inner medulla, where it is added to the corticopapillary osmotic gradient. Two factors allows the movement of water out into the osmotically high medullary interstitium by osmosis: The high permeability to water of the thin descending limb of the loop of Henle, 2. The continuous inflow of tubular fluid from the proximal tubule 1. CORTICOPAPILLARY OSMOTIC GRADIENT it is a gradient of osmolarity in the interstitial fluid of the kidney from the cortex to the papilla The osmolarity of the cortex is approximately 300 mOsm/L, similar to the osmolarity of other body fluids. Moving from the cortex to the outer medulla, inner medulla, and papilla, the interstitial fluid osmolarity progressively increases. At the tip of the papilla, the osmolarity can be as high as 1200 mOsm/L. countercurrent multipliers The process is best understood hypothetically for a cortical nephron as follows (see the diagram below): Assuming that the osmolality throughout the descending and ascending limbs and the medullary interstitium is (300 mosm/kg H2O) (1). Assuming, also, that the pumps in the thick ascending limb can pump 100 mosm/kg of Na+ and Cl¯ from the tubular fluid to the interstitium, increasing the interstitial osmolality to (400 mosm/kg H2O) (2). Water then moves out of the thin descending limb, and its content equilibrates with the interstitium (3). However, fluid continuing (300 mosm/kg H2O) is continuously entering this limb from the proximal tubule, which again equilibrates with the interstitium (4), so the gradient against which Na+ and Cl¯ are pumped is reduced; and more enter the interstitium (5). Meanwhile, hypotonic fluid flows into the distal tubule and isotonic and subsequently hypertonic fluid flows into the thick ascending limb (6) and (7). The process keeps repeating (4) – (6) and the fluid is progressively concentrated as it flows down the descending limb and progressively diluted as it flows up the ascending limb. The final result is a gradient of osmolarity from the top to the bottom of the loop that is even greater at the tip of juxtamedullary nephrons with longer loops of Henle, causing additional passive countercurrent multiplication Vasa Recta The vasa recta are capillaries that serve the medulla and papilla of the kidney. The vasa recta follow the same course as the loops of Henle and have the same hairpin (U) shape. Only 5% of the renal blood flow serves the medulla, and blood flow through the vasa recta is especially low. The vasa recta participate in countercurrent exchange, which differs from countercurrent multiplication as follows: Countercurrent multiplication is an active process that establishes the corticopapillary osmotic gradient Countercurrent exchange is a purely passive process that helps maintain the gradient. The passive properties of the vasa recta are the same as for other capillaries: They are freely permeable to small solutes and water. Blood flow through the vasa recta is slow, and solutes and water can move in and out, allowing for efficient countercurrent exchange. Countercurrent exchange is illustrated schematically The figure shows a single vasa recta, with its descending limb and ascending limb. Blood entering the descending limb has an osmolarity of 300 mOsm/L. As this blood flows down the descending limb, it is exposed to interstitial fluid with increasingly higher osmolarity (the corticopapillary osmotic gradient). Since the vasa recta are capillaries, small solutes, such as NaCl and urea, diffuse into the descending limb and water diffuses out, allowing blood in the descending limb of the vasa recta to equilibrate osmotically with the surrounding interstitial fluid. At the bend of the vasa recta, the blood has an osmolarity equal to that of interstitial fluid at the tip of the papilla, 1200 mOsm/L. In the ascending limb, the opposite events occur. As blood flows up the ascending limb, it is exposed to interstitial fluid with decreasing osmolarity. Small solutes diffuse out of the ascending limb and water diffuses in, and the blood in the ascending limb of the vasa recta equilibrates with the surrounding interstitial fluid. The blood leaving the vasa recta has an osmolarity of 325 mOsm/L, which is slightly higher than the osmolarity of the original blood that entered it. Some of the solute from the corticopapillary osmotic gradient was picked up and will be carried back to the systemic circulation. With time, this process could dissipate the corticopapillary osmotic gradient. The gradient normally does not dissipate, however, because the mechanisms of countercurrent multiplication and urea recycling continuously replace any solute that is carried away by blood flow. In the presence of ADH, the hypotonic tubular fluid which passes through the distal tubule will cause water to pass out of the tubule into the hypertonic interstitium driven by the osmotic pressure gradient. Even more water would be reabsorbed into the more hypertonic medullary interstitium, as the fluid passes down the collecting ducts. This hormone makes the tubular epithelium highly permeable to water, by: causing the insertion of “aquaporin 2” water channels into the apical membrane of the principal cells. It would facilitate the movement of urea into the medullary interstitium. As a result, concentrated urine would be excreted. in the absence of ADH, membranes of the distal tubule and the collecting duct would become relatively impermeable to water. Therefore, tubular fluid remains hypotonic, causing larger amounts to flow into the renal pelvis, increasing water loss in urine. In the absence of ADH, urea would move from the interstitium into the hypotonic tubular fluid in the inner collecting duct and the osmotic gradient of the pyramids is reduced; thereby aiding in the excretion of diluted urine.