Physiology 28 [5-11
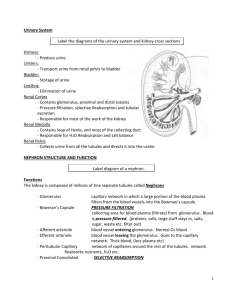
advertisement

Physiology 28 - - - - - - - Osmolarity = amount of solute/volume of ECF Total body water controlled by fluid intake, renal excretion of H2O Kidneys can excrete dilute or concentrated urine independent of solute excretion o ADH/vasopressin = primary effector of renal water excretion feedback When osmolarity increases (too concentrated), posterior pituitary secretes ADH -> increased permeability of distal and collecting tubules to water Mechanism for excreting dilute urine -> kidney reabsorbs solutes while failing to reabsorb water o Proximal tubule -> solute and H2O reabsorbed proportionally (isosmotic to plasma ~300 mOsm/L) o Descending loop of Henle -> H2O reabsorbed (osmosis) (hypertonic) o Ascending loop of Henle (thick) -> Na, K, Cl avidly reabsorbed, impermeable to H2O (hypotonic ~100 mOsm/L) Regardless of whether ADH is present or absent, fluid leaving early distal tubular segment is hypoosmotic o Distal tubule, cortical collecting duct, and collecting duct -> additional NaCl reabsorption, impermeable to H2O without ADH (further dilutes, ~50 mOsm/L) Water lost from body via lung evaporation, GI feces, skin evaporation and perspiration, urine Water deficit -> kidney concentrates urine (solute excretion > H2O excretion) o Maximum urine [] 1200-1400 mOsm/L Max concentrating ability dictates urine volume excreted o Ex. normal human excretes 600 mOsm/day and max urine concentrating ability is 1200 mOsm/L -> minimal volume to be excreted (obligatory urine volume) = 600/1200 = 0.5L/day Dehydration with ingestion of seawater because of high [] of solutes approaching max concentrating ability + excretion of regular metabolites (urea) -> net fluid loss Urine specific gravity = clinical estimate of urine solute concentration (more [], higher s.g. increasing linearly) -> measure with refractometer o Determined by number and size of solute molecules o Expressed in grams/ml and ranges 1.002-1.028 g/ml (↑ 0.001 for every 35-40 mOsm/L) Altered with high amounts of large molecules (glucose, radiocontrast, antibiotics) Requirements for concentrating urine = high level of ADH and high osmolarity of renal medullary interstitial fluid (osmotic gradient for H2O reabsorption) o Renal medullary interstitium normally hyperosmotic Countercurrent mechanism depends on special anatomical arrangement of the loops of Hele and the vasa recta (specialized peritubular capillaries of renal medulla) o 25% of nephrons = juxtamedullary nephrons Osmolarity of medullary interstitial fluid = 1200-1400 mOsm/L in pelvic tip of medulla o - - - - - - Buildup of solute [] -> active transport of Na w/ cotransport of K, Cl, and other ions (thick ascending limb); active ion transport from collecting ducts; facilitated diffusion of urea; low diffusion of water TAL active and cotransport establishes 200 mOsm [] gradient (impermeable to H2O) Steps to hyperosmotic renal medullary interstitium: o Loop of Henle fluid ~300 mOsm/L o TAL established 200 mOsm/L gradient (~400 mOsm/L in interstitium) o descending limb of loop of Henle and interstitial fluid reach equilibrium (osmosis) o additional fluid from proximal tubule added (hyperosmotic DL fluid to AL) o Ions pumped from AL into intersititum (200 mOsm/L gradient created again) o Repeat until interstitium concentrated Gradually traps solutes in medulla and multiplies [] gradient -> interstitial fluid osmolarity to 1200-1400 mOsm/L Repetitive reabsorption of NaCl by TAL and new NaCl from proximal tube = countercurrent multiplier Fluid is dilute at distal convoluted tubule (100 mOsm/L) -> further dilution in early distal tubule o ADH affects late distal tubule and cortical collecting tubule Large amounts of H2O absorbed in cortex preserves high medullary interstitial fluid osmolarity o Medullary collecting duct reabsorbs less water carried away by vasa recta into veins Urea contributes about 40-50% osmolarity of renal medullary interstitium (passively reabsorbed from tubule) o Ascending loop, distal and cortical collecting tubules -> impermeable to urea but with high ADH, water reabsorbed and urea concentrated o High [urea] in inner medullary collecting duct causes diffusion out (facilitated by urea transporters, UT-A1 and UT-A3) -> high urea [] in tubule maintained tho UT-A3 activated by ADH o High protein diet can concentrate urine much better Rate of urea excretion determined by [urea] in plasma and the GFR o Renal disease with reduced GFR -> plasma urea ↑ to return filtered urea load/excretion rate to normal Proximal tubule reabsorbed 40-50% of filtered urea o Urea [] increases through tubules from H2O reabsorption and secretion into think loop from medullary interstitium Secretion of urea into thin loop of Henle = urea transporter UA-A2 o TAL, distal and cortical collecting tubule impermeable to urea (may even ↑ urea [] if ADH present) -> passive diffusion in medullary collecting duct Recirculation of urea additional mechanism to form hyperosmotic renal medulla Excess water in body increases urine flow rate so [urea] in medullary collecting duct reduced Special features of renal medullary bloody flow (preserve high solute []) = medullary blood flow is low and vasa recta serve as countercurrent exchangers o - - - - - Vasa recta highly permeable to solutes except for plasma proteins -> concentrated descending into medulla and less concentrated back up as H2O moves in Little dilution because of U shape -> vasa recta do not create medullary hyperosmolarity by prevent it from dissipating Vasodilators and increased AP ↑ medullary BF “washing out” solutes and reducing concentrating ability Proximal tubule -> 65% electrolyte reabsorption with osmosis (no change in fluid osmolarity) Descending loop of henle -> H2O absorbed (osmolarity increases) Thin Ascending loop of Henle -> impermeable to H2O, some NaCl reabsorption and passive diffusion (osmolarity decreases), urea secretion (recycling) Thick Ascending Loop o Henle -> impermeable to water, high Na, Cl, K and ion active transport (osmolarity decreases) Early distal tubule -> solutes reabsorbed, H2O remains (further dilution) Late distal tubule and cortical collecting tubule -> dependent on ADH, urea not permeant (increased [urea]) Inner medullary collecting ducts -> dependent on ADH and medullary interstitium osmolarity, specific urea transporters o The kidney can, when needed, excrete highly concentrated urine that contains little NaCl (other solutes, urea, contribute to hyperosmolarity) Occurs in dehydration with low Na intake (stimulates renin-angiotensinaldosterone) o Large quantities of dilute urine can be excreted without increasing the excretion of Na (decreased ADH secretion) o Obligatory urine volume (dictated by urine [] ability) Total clearance of solutes from blood = osmolar clearance (Cosm) o Cosm= Uosm x V/Posm , (V is urine flow rate) Free water clearance (CH2O) = V – Cosm o Rate at which solute-free water is excreted by the kidneys -> positive = water>solute clearance, negative = solute>water clearance o Whenever urine osmolarity is greater than plasma osmolarity, CH2O is negative Disorders of urinary concentrating ability: o Inappropriate secretion of ADH o Impairment of countercurrent mechanism o Inability of distal tubule, collecting tubule, and collecting ducts to respond to ADH Central Diabetes Insipidus = inability to produce or release ADH from posterior pituitary o Large volume of dilute urine -> thirst mechanism activated so continue to drink H2O but severe dehydration can occur if insufficient H2O intake o Treatment -> desmopressin (synthetic ADH analog) selective for V2 receptors Nephrogenic Diabetes Insipidus = tubules don’t respond to ADH or failure of countercurrent mechanism o Large volume of dilute urine o - - - - - - Causes: renal diseases, impaired loop of Henle (diuretics like furosemide), drugs (lithium and tetracyclines impaire distal nephron response) o Distinguished from central by desmopressin administration (lack of effect) o Treatment -> underlying cause eliminated, low-Na diet, diuretic enhancing Na excretion (thiazide) Plasma Na [] regulated between 140-145 mEq/L o Posm estimated from plasma Na [] Posm = 2.1 x Plasma [Na] o For more accuracy, include glucose and urea [] o Na, HCO3 and Cl = 94% of extracellular osmoles Primary systems regulating [Na] and ECF osmolarity = osmoreceptor ADH-system and thirst mechanism Osmoreceptor-ADH feedback system: o High ECF osmolarity causes osmoreceptor cells in anterior hypothalamus to shrink -> sends signals in supraoptic nuclei relaying down to post pituitary -> release ADH (water reabsorption and excretion of concentrated urine) Hypothalamus contains magnocellular neurons that synthesize ADH in the supraoptic and paraventricular neuclei -> extend into posterior pituitary (ADH stored in secretory granules) Anteroventral region of the third ventricle (AV3V region): upper part = subfornical organ and inferior part = organum vasculosum of lamina terminalis; between is median preoptic nucleus o Lesions of AV3V region cause deficit in ADH secretion, thirst, Na appetite, and BP o Osmoreceptors are in vicinity o Lack BBB allowing solutes to cross and rapidly respond to change Arterial baroreceptor reflexes and cardiopulmonary reflexes control ADH, too (originate in aortic arch, carotid sinus and cardiac atria) -> signal through CN IX and X through tractus solitarus -> hypothalamic nuclei o ↓ arterial P and blood volume trigger ADH secretion (only when 10% decrease) ADH more sensitive to small osmolarity change Nausea = potent ADH stimulus Nicotine and morphine stimulate ADH, alcohol inhibit ADH (thus marked diuresis) AV3V region + preoptic nucleus = thirst center o Organum vasculosum of lamina terminalis involved in sensing CSF osmolarity Stimuli for thirst: o Increased ECF osmolarity causes o Angiotensin II intracellular dehydration of o Dryness of mouth/esophagus thirst centers o GI and pharyngeal stimuli o Decreased ECF volume and AP Na above 2 mEq/L of normal = threshold for drinking If either ADH or thirst mechanism fail, the other system can compensate reasonably but if both lost, poor control of Na [] and osmolarity Angiotensin II and aldosterone -> increase amount of Na in ECF and ECF volume via osmosis o have little effect on Na concentration except under extreme conditions o o - Even without functional aldosterone feedback system, plasma [Na] well regulated ADH-thirst mechanism overshadows angiotensin II-aldosterone system (even in primary aldosteronism [Na] increases only 3-5 mEq/L above normal) o In extreme conditions (adrenalectomy or Addison’s disease) loss of Na by kidneys can reduce plasma [Na] -> thirst mechanism triggered but only ↑ H2O reabsorption so more dilution Humans can survive with only 10-20 mEq/day of Na o Salt appetite = behavioral drive when Na deficiency (important in Addison’s disease) o Primary stimuli that increase salt appetite = association with Na deficits and ↓ blood volume/BP (circulatory insufficiency) o Neuronal mechanism analogous to that of thirst mechanism (AV3V region)