Chapter 19 - WordPress.com
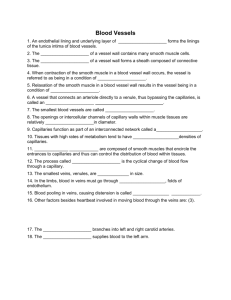
advertisement

Lecture – 9 (19) Sept. 21, 2011 [42:00] PG.695-671 Lumen = a central blood-containing space of a vessel Tunica Intima = the innermost tunic of a vessel, containing endothelium (simple squamous) Tunica Media = the middle tunic composed of mostly circular smooth muscle/sheets of elastin; this layer is responsible for vasoconstriction and vasodilation – small changes in vessel diameter can greatly affect blood flow and blood pressure. Tunica Externa = the outermost layer of the vessel – composed of mostly collagen fibers that protect and reinforce the vessel, anchoring it to surrounding structures Blood Flow: Heart Aorta Arteries Arterioles Capillaries Venules Veins Vena Cava Elastic (Conducting) Arteries Elastic arteries are the thick-walled arteries near the heart – the aorta and its major branches. Elastic arteries are sometimes called conduction arteries. Arterioles = the smallest arteries Capillaries = microscopic, the smallest blood vessels, consisting of exceedingly thin walls of just a thin tunica intima. At strategic locations along the outer surface of some capillaries are spider-shaped pericytes, smooth muscle-like cells that stabilize the capillary wall & help control capillary permeability. Capillary Structure: Basement membrane is incomplete only in the Sinusoidal capillaries and that pericytes most often occur on Continuous capillaries. [see page 699] Continuous Capillary – Least permeable, and most common (e.g., skin, muscle) Fenestrated Capillary – Large fenestrations (pores) increase permeability, occurs in special locations (e.g., kidney, small intestine) Sinusoidal Capillary – Most permeable, occurs in special locations (e.g., liver, bone marrow, spleen) Lecture – 10 (19) Sept. 26, 2011 BP 120/80 = Pulse Pressure of 40 BP 150/130 = PP of 20 [20 less efficient than 40] Mean Arterial Pressure (MAP) = Average of the arterial pressure and because the heart spends more time in relaxation than in contraction, the MAP is less than the actual median. Example: BP 120/80 has a MAP of less than 100; approximately 93 [ MAP = diastolic + PP/3] 1 Venous System - Systemic veins are called capacitance vessels because they are distensible and contain a large portion (60-65%) of the blood volume at any given time. Varicose Veins – veins that have become tortuous and dilated because of incompetent (leaky) valves; usually in the lower limbs. Several factors contribute, including heredity and conditions that hinder venous return: prolong standing in one position, obesity, pregnancy, and sitting on long flights. Varicosities in the anal veins are called hemorrhoids. Physiology of Circulation 1. Blood Flow – the volume of blood flowing through a vessel, an organ, or the entire circulatory system in a given period (ml/min.) Blood flow through the entire system = Cardiac Output 2. Blood Pressure (BP) – the force per unit area exerted on a vessel wall by the contained blood, is expressed in millimeters of mercury (mm Hg). It is the pressure gradient – the differences in blood pressure within the vascular system – that provides the driving force that keeps blood moving, always from an area of higher pressure to an area of lower pressure, through the body. 3. Resistance – is opposition to flow and is a measure of the amount of friction blood encounters as it passes through the vessels; aka Peripheral resistance. Three important sources of resistance are: blood viscosity, vessel length, and vessel diameter. a. Blood Viscosity – the internal resistance to flow that exists in all fluids and is related to the thickness or stickiness of a fluid. Distilled water has a viscosity of 1. The greater the viscosity the greater the resistance. b. Total Blood Vessel Length – the longer the vessel the greater the resistance. [Think of the longer a water hose the greater the resistance. c. Blood Vessel Diameter – changes in blood vessel diameter are frequent and significantly alter peripheral resistance. Fluid close to the wall of a tube or channel is slowed by friction as it passes along the wall, whereas fluid in the center of the tube flows more freely and faster. Smaller diameter has greater resistance. (Think of a 1” pipe connecting to a ½” pipe, a greater resistance) Resistance varies inversely with the fourth power of the vessel radius (1/2 the diameter). Relationship Between Flow, Pressure, and Resistance Flow = Change Pressure (PP) / Resistance F = ∆P/R Note: Blood flow (F) is directly proportional to the difference in blood pressure (∆P) between two points in circulation, that is, the blood pressure, or hydrostatic pressure, gradient. ↑ ∆P = ↑ Flow ↓ ∆P = ↓ Flow Anything ↑ R (resistance) = ↓ Flow Of these two factors influencing blood flow, Resistance (R) is far more important than PP (∆P). 2 Systemic Blood Pressure Arterial Blood Pressure – reflects two factors: 1. How much the elastic arteries close to the heart can be stretched 2. The volume of blood forced into them at any time Systolic Pressure – the peak pressure (at contraction) Diastolic Pressure – the lowest pressure (during relaxation) Pulse Pressure – the difference between the Systolic and Diastolic pressures Mean Arterial Pressure (MAP) – the pressure that propels the blood to the tissues MAP = Diastolic pressure + 1/3 of the Pulse Pressure Example: BP 120/80 has a MAP of 93 [MAP = diastolic + PP/3] [MAP = 80 + 40/3] Greatest drop in pressure occurs in the Arterioles – preventing capillary from rupturing Venous Blood Pressure Despite the structural modifications of veins (large lumens and valves), venous pressure is normally too low to promote adequate venous return. For this reason, three functional adaptations are critically important to venous return. 1. Respiratory Pump – pressure changes occurring in the ventral body cavity during breathing create the respiratory pump that moves blood up toward the heart. On inhalation, abdominal pressure increases, squeezing the local veins forcing blood toward the heart. 2. Muscular Pump – consisting of skeletal muscle activity; these muscles surrounding the deep veins contract and relax, they ‘milk’ blood toward the heart, and once blood passes each successive valve, it cannot flow back. 3. Smooth Muscle Layer – around the veins constrict under sympathetic control, increasing venous return. This is yet another way in which the sympathetic nervous systems increases cardiac output. Maintaining Blood Pressure Homeostatic mechanisms that regulate cardiovascular dynamics are those that maintain blood pressure, principally cardiac output, peripheral resistance, and blood volume. F = ∆P/R or CO = ∆P/R or ∆P = CO x R 3 ↑ CO & ↑ BP Clearly, blood pressure varies directly with CO and R. Additionally, blood pressure varies directly with blood volume because CO depends on blood volume (the heart can’t pump out what doesn’t enter its chambers). So in theory, a change (↑ or ↓) in any of these variables would cause a corresponding change in blood pressure. Short-Term Mechanisms: Neural Controls The short-term controls of BP, mediated by the nervous system and blood borne chemicals, counteract moment-to-moment fluctuations in BP by altering peripheral resistance (and CO). Neural controls of peripheral resistance are directed at two main goals: 1. Maintaining adequate MAP by altering blood vessel diameter. (small changes in blood vessel diameter cause substantial changes in peripheral resistance, and hence in systemic BP). 2. Alerting blood distribution to respond to specific demands of various organs. Most neural controls operate via reflex arcs involving baroreceptors and associated afferent fibers, the vasomotor center of the medulla, vasomotor fibers, and vascular smooth muscle. Occasionally, inputs from chemoreceptors and higher brain centers also influence neural control mechanism. Note: Baroreceptors and Chemoreceptors are located in the Aorta and Carotid Arteries. Role of the Vasomotor Center Vasomotor Center – a cluster of neurons in the medulla that oversees changes in the diameter of blood vessels. Cardiovascular Center – integrates blood pressure control by altering cardiac output and blood vessel diameter. Vasomotor activity is modified by inputs from: 1. Baroreceptors – pressure sensitive mechanoreceptors that respond to changes in arterial pressure and stretch 2. Chemoreceptors – receptors that respond to changes in blood levels of carbon dioxide, H+, and oxygen 3. Higher brain centers Baroreceptor-initiated Reflexes As arterial pressure rises, it stretches baroreceptors, neural receptors located in the carotid sinuses and in the aortic arch, and in the walls of nearly every large artery of the neck and thorax. When stretched, baroreceptors send a rapid stream of impulses to the vasomotor center. This input inhibits the vasomotor center, resulting in vasodilation of not only arterioles but also veins, and a decline BP. 4 Chemoreceptor-Initiate Reflexes When CO2 levels rise, or the pH falls, or O2 content of the blood drops sharply, chemoreceptors in the aortic arch and large arteries of the neck transmit impulses to the cardioacceleratory center, which then increases cardiac output, and to the vasomotor center, which cause reflex vasoconstriction. The rise in BP that follows speeds the return of blood to the heart and lungs. The most prominent chemoreceptors are the carotid and aortic bodies located close by the baroreceptors in the carotid sinuses and aortic arch. Chemoreceptors are more important in regulating respiratory rate than BP. Influences of Higher Brain Centers Hypothalamus Medulla influences BP … these higher brain centers can modify arterial pressure via relays to the medullary centers. Fight/Flight response is mediated by the hypothalamus. The hypothalamus also mediates the redistribution of blood flow and other cardiovascular responses that occur during exercise and changes in body temperature. [via sympathetic responses] Short-Term Mechanisms: Hormonal Controls 1. Adrenal Medulla Hormones – during periods of stress, the adrenal gland releases norepinephrine (NE) and epinephrine to the blood, and both hormones enhance the sympathetic fight/flight response. NE has a vasoconstriction action. Epinephrine increases CO and promotes generalized vasoconstriction [EXCEPT: Cardiac and Skeletal Muscles –> Dilation] 2. Angiotensin II / Renin – when BP or blood volume are low, the kidneys release the hormone renin. Renin acts as an enzyme, ultimately generating angiotensin II, which stimulates intense vasoconstriction, promoting a rapid rise in systemic blood pressure. It also stimulates release of aldosterone and ADH (vasopressin), which act in long-term regulation of BP by enhancing blood volume. 3. Atrial Natriuretic Peptide (ANP) – the atria of the heart produce the hormone ANP, which causes blood volume and BP to decline. ANP antagonizes aldosterone and prods the kidneys to excrete more sodium and water from the body, causing blood volume to drop. It also causes generalized vasodilation. 4. Antidiuretic Hormone (ADH) – produced by the hypothalamus, ADH/vasopressin stimulates the kidneys to conserve water. 5 Long-Term Mechanisms: Renal Regulation The long-term controls of BP, mediated by renal mechanisms, counteract fluctuations in blood pressure not by altering peripheral resistance (as in short-term controls) but rather by altering blood volume. Indirect Renal Mechanisms – is the renin-angiotensin mechanism. As arterial BP declines the kidneys release renin (enzymatic hormone) into the blood. Renin triggers a series of reactions that produce angiotensin II. Angiotensin II increases blood pressure in three main ways: 1. It is a potent vasoconstrictor, ↑ BP by ↑ peripheral resistance 2. It stimulates the adrenal cortex to secret aldosterone, a hormone that enhances renal reabsorption of sodium; as sodium moves into the bloodstream, water follows. 3. It prods the posterior pituitary to release ADH, which promotes more water reabsorption. Monitoring circulatory Efficiency Vital Signs = Pulse & BP Alterations in Blood Pressure Hypotension – Systolic Pressure < 100mm Hg Orthostatic Hypotension – temporary low BP and dizziness when the elderly rise suddenly from a reclining or sitting position. The aging sympathetic nervous system does not respond as quickly as it once did to postural changes, so blood pools briefly in the lower limbs. Chronic Hypotension – may hint at poor nutrition, anemia and inadequate levels of blood proteins, both of which reduce blood viscosity. Acute Hypotension – is one of the most important signs of circulatory shock (threat to pts undergoing surgery and those in ICU. Hypertension – (> 140/90) high blood pressure may be transient or persistent. Transient elevations in systolic pressure occur as normal adaptations during fever, physical exertion, and emotional upset. Persistent hypertension is common in obese people for variety of reasons that are not completely understood. Prolonged hypertension is the major cause of heart failure, vascular disease, renal failure, and stroke. Hypertension also raveages the blood vessels, accelerating the progress of atherosclerosis. 6 Primary or Essential Hypertension – (90%) in which no underlying cause has been identified & cannot be cured, only controlled by reducing environmental factors and/or medication (diuretics, betablockers, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin II receptor blockers. Primary Hypertension is due to a rich interplay between hereditary predispositions and a variety of environmental factors: 1. 2. 3. 4. 5. 6. 7. Heredity – Hypertension run in families. Diet – high intakes of salt, saturated fat, and cholesterol & deficiencies in K+, Ca++, Mg++ Obesity Age – usually appear after age of 40 Diabetes mellitus Stress Smoking – nicotine enhances the sympathetic nervous systems vasoconstrictor effects Secondary Hypertension – (10%) is due to identifiable disorders, such as obstruction of the renal arteries, kidney disease, and endocrine disorders such as hyperthyroidism and Cushing’s syndrome. Blood Flow Through Body Tissues: Tissue Perfusion Tissue Perfusion – blood flow through body tissues is involved in 1. 2. 3. 4. Delivery of oxygen and nutrients to, and removal of wastes from, tissue cells Gas exchange in the lungs Absorption of nutrients from the digestive tract Urine formation in the kidneys Velocity of Blood Flow The speed/velocity of blood flow changes as blood travels through the systemic circulation. It is fastest in the aorta and other large arteries, slowest in the capillaries, & then picks up speed again in the veins. The velocity of the blood flow declines in the capillaries due to the fact that there is more volume in capillaries than in the arteries/arterioles. Slow capillary flow is beneficial because it allows adequate time for exchanges between the blood and tissues cells. Autoregulation: Local Regulation of Blood Flow Autoregulation – the automatic adjustment of blood flow to each tissue in proportion to the tissue’s requirements at any instant. This process is regulated by local conditions and is largely independent of systemic factors. 7 Summary of Intrinsic and Extrinsic Control of Arteriloar Smooth Muscle in the Systemic Circulation Dilation of Vessels Constriction of Vessels Intrinsic Mechanisms (Autoregulation) Extrinsic Mechanisms (MAP/Exercise) Metabolic Controls Nervous Controls ↓ Amounts of: pH Sympathetic Hormones O2 ↑ Amounts of: CO2 α Receptors Epinephrine β Receptors Norepinephrine Angiotensin II Nitrous Oxide ↑ CO2 = ↓ pH = greater acidity or acidosis Blood Flow in Special Areas pg. 715-717 Autoregulation in the brain, heart, and kidneys is extraordinarily efficient. In those organs, adequate perfusion is maintained even when MAP is fluctuating. Skeletal Muscles – Generally speaking, capillary d3ensity and blood flow are greater in red (slow oxidative) fibers than in white (fast glycolytic) fibers. When muscle become active, blood flow increases (hyperemia) in direct proportion to their greater metabolic activity, a phenomenon called active or exercise hyperemia. Ultimately, the major factor determining how long muscles can continue to contract vigorously is the ability of the cardiovascular system to deliver adequate oxygen and nutrients and remove waste products. The Brain – Constant cerebral blood flow is necessary because neurons are totally intolerant of ischemia (lack of blood). Although the brain is the most metabolically active organ in the body, it is the least able to store essential nutrients. Brain tissue is exceptionally sensitive to declining pH (acidosis), and increased blood carbon dioxide levels, resulting in acidic conditions in brain tissue and causes marked vasodilation. Oxygen deficit is a much less potent stimulus for autoregulation. 8 When MAP declines, cerebral vessels dilate to ensure adequate brain perfusion. When MAP rises, cerebral vessels constrict, protecting the small, more fragile vessels farther along the pathway from rupture due to excessive pressure (aneurysm or stroke). Fainting, or syncope occurs when MAP falls below 60 mm Hg. The Skin – Blood flow through the skin: 1. Supplies nutrients to the cells [served by autoregulation, responding to the need for oxygen] 2. Aid in body temperature regulation [neural intervention] 3. Provides a blood reservoir [neural intervention] The primary function of the cutaneous circulation is to help maintain body temperature. Below the skin surface are extensive venous plexuses. The capacity of these plexuses enables neural adjustments of blood flow through arterioles and through unique coiled arteriovenous anastomoses. These tiny A-V shunts are located mainly in the fingertips, palms, toes, soles, ears, nose, and lips. Vasodilation of the arterioles is enhanced even more when we sweat, because an enzyme in perspiration acts on a protein present in tissue fluid to produce bradykinin, which stimulates the vessel’s endothelial cells to release the potent vasodilator NO (nitric oxide). Paradoxically, (when cold) the skin may stay quite rosy because some blood gets ‘trapped’ in the superficial capillary loops as the shunts swing into operation. The trapped blood remains red because the chilled skin cells take up less oxygen, leaving the blood oxygen saturation elevated. The Lungs – The pulmonary circuit is relatively short, and pulmonary arteries and arterioles are structurally like veins and venules; they have thin walls and large lumens. Because resistance to blood flow is low in the pulmonary arterial system, less pressure is needed to propel blood though those vessels.Autoregulatory mechanism in pulmonary circulation is opposite of what is seen in most tissues: low pulmonary oxygen levels cause vasoconstriction, and high levels promote vasodilation. When air sacs of the lungs are flooded with oxygen-rich air, the pulmonary capillaries become flushed with blood and ready to receive the oxygen load. If the air sacs are collapsed or blocked with mucus, the oxygen content in those areas is low, and blood largely bypasses those nonfunctional areas. The Heart – When the ventricles contract and compress the coronary vessels, blood flow through the myocardium stops. As the heart relaxes, the high aortic pressure forces blood through the coronary circulation. An abnormally rapid heartbeat seriously reduces the ability of the myocardium to receive adequate oxygen and nutrients during diastole, time for filling of coronary arteries is reduced. During strenuous exercise, the coronary vessels dilate in response to local accumulation of vasodilators (particularly adenosine), and blood flow may increase three to four times. Additionally, any event that decreases the oxygen content of the blood releases vasodilators that adjust the O2 supply to the O2 demand. 9 Blood Flow Through Capillaries and Capillary Dynamics Blood flow through capillary networks is slow and intermittent. This phenomenon, called vasomotion, reflects the on/off opening and closing of pre-capillary sphincters in response to local Autoregulatory controls. Oxygen, carbon dioxide, most nutrients, and metabolic wasters pass between the blood and interstitial fluid by diffusion -> movement always occurs along a concentration gradient -> each substance moving from an area of its higher concentration to an area of its lower concentration. There are four different routes across capillaries for different types of molecules: 1. Lipid-soluble molecules, such as respiratory gasses, diffuse through the lipid bilayer of the endothelial cell plasma membranes. Small water-soluble solutes, such as amino acids and sugars, also pass through. 2. Fluid filled intercellular capillary clefts 3. Fenestrations (small openings) 4. Some larger molecules, such as proteins, are actively transported in pinocytotic vesicles (pinching off – transport vessicles) or caveolae. FLUID FLOWS AT CAPILLARIES 1. Leaks 2. IFP 3. BOP 4. IFOP CAPILLARY 1 – Blood Pressure (Heart the greatest) creating a leaky vessel 2 – Interstitial Fluid Pressure – pushing fluids back into capillary 3 – Blood Osmotic Pressure – draws in fluids due to ↑ diluents (hypertonic solution – water follows) 4 – Interstitial Fluid Osmotic Pressure – draws out fluids to balance water/diluents ratios/gradients Note: Albumin is responsible for osmotic pressure / ↓ albumin and edema occurs 10 Circulatory Shock pg.719/20 Circulatory Shock – any condition in which blood vessels are inadequately filled and blood cannot circulate normally. This results in inadequate blood flow to meet tissue needs. If the condition persists, cells die and organ damage follows. Hypovolemic Shock – results from large-scale loss of blood, as might follow acute hemorrhage, severe vomiting or diarrhea, or extensive burns. If blood volume drops rapidly, heart rate increases in an attempt to correct the problem. Thus, a week, thready pulse is often the first sign of hypovolemic shock. A sharp drop in BP is a serious, and late, sign of hypovolemic shock. The key to managing hypovolemic shock is to replace fluid volume as quickly as possible. Vascular Shock – blood volume is normal, but circulation is poor as a result of an abnormal expansion of the vascular bed caused by extreme vasodilation. A common cause is loss of vasomotor tone due to anaphylaxis (anaphylactic shock), a systemic allergic reaction in which body-wide vasodilation is triggered by the massive release of histamine. Two other common causes are failure of autonomic nervous system regulation – neurogenic shock, and septic shock, septicemia, a sever systemic bacterial infection (bacterial toxins are notorious vasodilators. Cardiogenic Shock – or pump failure, occurs when the heart is so inefficient that it cannot sustain adequate circulation. Its usual cause is myocardial damage, as might follow numerous myocardial infarcts, heart attacks. Lecture – 11 (19) Sept. 28, 2011 Osmotic Pressure – Water chases Solutes The side with the higher levels of solutes has the higher osmotic pressure [8:00] pg.721 – 742 Circulatory System is divided into Pulmonary Circuit and the Systemic Circuit Circle of Willis – is an example of anastomosis, collateral vessels feeding the same area. Hepatic Portal (pg.742) filters blood to the liver (from all digestive organs) in order to screen (filter out toxicities) and for delivery of nutrients. This is an interruption of blood flow to the heart. Once filtered, the liver drains into the Hepatic Veins and then joins the Inferior Vena Cava and onto the heart. 11