I. Blood and Blood Cells

Chapter 14
1
I. Blood and Blood Cells
1. Blood is three to four times more viscous than water.
2. Most blood cells form in red bone marrow.
3. Types of blood cells are red blood cells and white blood cells.
4. Cellular fragments of blood are platelets.
5. Formed elements of blood are the cells and platelets
2
•
What type of tissue is blood?
•
Cells are suspended in what type of matrix?
•
What are “formed elements” of blood?
Answers: connective tissue with a liquid extracellular matrix and containing suspended formed elements of white cells, erythrocytes, and platelets.
3
Blood Volume
• varies with
• body size
• changes in fluid concentration
• changes in electrolyte concentration
• amount of adipose tissue
• about 8% of body weight
• about 5 liters
4
B. Blood Volume and Composition
1. Blood volume varies with body size, changes in fluid and electrolyte concentrations, and the amount of adipose tissue.
2. Blood volume is about 8% of body weight.
3. An average-size adult has 5 liters of blood.
5
B. Blood Volume and Composition
4. Hematocrit is the percentage of blood cells in a blood sample.
5. A blood sample is usually 45 % red blood cells and 55 % plasma.
6. Plasma is a mixture of water, amino acids, proteins, carbohydrates, lipids, vitamins, hormone, electrolytes, and cellular wastes.
7. Less than 1% of formed elements of blood are white blood cells and platelets and 99% are red blood cells.
6
• What is the composition of the buffy coat?
• How can one separate blood components?
• Answers:
• white blood cells and platelets
• centrifugation and settling
7
Blood Composition
8
•
What is the hematocrit?
•
What is a typical value for a hematocrit?
•
What is another name for hematocrit?
•
Answers:
•
% of packed RBC volume in relation to overall total volume of all components.
•
45%
• packed cell volume
9
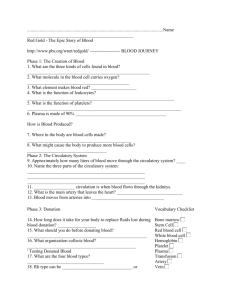
Figure 14.02
10
• What percentage of blood is composed of plasma?
• What percentage of plasma is made of water?
• What gases are present in plasma?
• What proteins are found in plasma and what percentage of plasma do the constitute?
11
Blood Plasma
• straw colored
• liquid portion of blood
• 55% of blood
• 92% water
12
C. The Origin of Blood Cells
1. Blood cells originate in red bone marrow from hemocytoblasts or hemopoietic stem cells.
2. A stem cell can differentiate into any number of specialized cell types.
3. Colony-stimulating factors are growth factors that stimulate stem cells to produce certain cell types.
4. Thrombopoietin stimulates the production of megakaryocytes.
13
Origin of Blood Cells
14
• What is another name for an hemocytoblast?
• What marrow cell is the precursor for platelets?
• What is another name for platelets?
• Answers
• Hematopoietic stem cell
• Megakaryocytes
• Thrombocytes
15
Figure 14.03aa
16
Figure 14.03
17
Characteristics of Red Blood Cells
• erythrocytes
• biconcave discs
• one-third hemoglobin
• oxyhemoglobin
• deoxyhemoglobin
• can readily squeeze through capillaries
• lack nuclei and mitochondria
18
D. Characteristics of Red Blood
Cells
• Red blood cells are also called erythrocytes.
• Red blood cells are biconcave in shape.
• The shape of red blood cells allow them to have an increased surface area for the transport of gases.
• Hemoglobin is an oxygen carrying protein in red blood cells.
• Each red blood cell is about one-third hemoglobin by volume.
19
D. Characteristics of Red Blood
Cells
• Oxyhemoblobin is hemoglobin combined with oxygen.
• Deoxyhemoglobin is hemoglobin that has released oxygen.
• Red blood cells extrude their nuclei as they mature.
• Because red blood cells lack mitochondria they must produce ATP through glycolysis.
• As red blood cells age, they become rigid and are more likely to be damaged and removed by enzymes in the liver and spleen.
20
Figure 14.04a
21
• Normal blood smear with:
– RBC’s
– Platelets (6 o'clock)
– Lymphocyte (center)
22
Normal Blood Elements
23
Cellular Blood Components
24
Red Blood Cell Counts
• number of RBCs in a cubic millimeter of blood
•
4,600,000 – 6,200,000 in males
•
4,200,000 – 5,400,000 in adult females
•
4,500,000 – 5,100,000 in children
• reflects blood’s oxygen carrying capacity
25
Red Blood Cell Production
• low blood oxygen causes kidneys and liver to release erythropoietin which stimulates RBC production
• vitamin B
12
, folic acid and iron necessary
26
F. Red Blood Cell Production and
Its Control
• Erythropoiesis is red blood cell production.
• Initially, red blood cell formation occurs in the yolk sac, liver and spleen.
• After an infant is born, red blood cells are produced almost exclusively in the red bone marrow.
• Hemocytoblasts in red bone marrow give rise to erythroblasts that give rise to erythrocytes.
27
F. Red Blood Cell Production and
Its Control
• Reticulocytes are immature red blood cells that still contain endoplasmic reticulum.
• The average life span of a red blood cell is 120 days.
• Erythropoietin controls red blood cell production and is released primarily from the kidneys.
• When the availability of oxygen decreases, erythropoietin is released and red blood cell production increases.
28
Life Cycle of Red Blood Cell
• circulate for about 120 days
• macrophages in spleen and liver destroy worn out RBCs
• hemoglobin is broken down into heme and globin
• iron from heme returns to red bone marrow
• bilirubin and biliverdin excreted in bile
Figure 14.06
29
Figure 14.08
30
Dietary Factors Affecting Red Blood
Cell Production
• Two vitamins needed for red blood cell production are vitamin B12 and folic acid.
• Intrinsic factor is needed for the absorption of vitamin B12.
• Iron is required for hemoglobin production.
• Anemia is a reduction in the oxygencarrying capacity of the blood.
31
Dietary Factors Affecting Red
Blood Cell Production
32
Types of Anemia
33
Normal RBCs
RBCs of person with hypochromic anemia
Anemia
34
• What is the amino acid substitution that results in sickle cell anemia?
• What hemoglobin subunit is affected?
35
Sickle Cell
• Single DNA base change causes addition of a single different amino acid in hemoglobin
• Hgb crystallizes in low oxygen
• Sickle cells cause blockages in small vessels
• Causes excruciating joint pain and organ damage
36
Sickle Cell
• Consequences of hemolysis include chronic anemia, jaundice, predisposition to aplastic crisis, cholelithiasis , and delayed growth and sexual maturation.
• Vascular occlusion and tissue ischemia can result in acute and chronic injury to virtually every organ of the body, most significantly the spleen, brain, lungs, and kidneys.
37
Sickle Cell
• Though in early childhood the spleen may be enlarged with sickle cell anemia, continual stasis and trapping of abnormal
RBC's leads to infarctions that eventually reduce the size of the spleen tremendously by adolescence. This is sometimes called "autosplenectomy". Seen here is the small remnant of spleen in a patient with sickle cell anemia.
38
Sickle Cell
•
Molecular Genetic Pathogenesis
• Hemoglobin
S results from the substitution of valine for glutamic acid in the second nucleotide of the sixth codon of the β-globin chain.
39
Sickle Cell
•
Diagnosis/testing.
• The term sickle cell disease encompasses a group of symptomatic disorders associated with mutations in the HBB gene and defined by the presence of hemoglobin S
(Hb S).
40
Sickle Cell
• Newborn screening.
• Because of the high morbidity and mortality of sickle cell disease in undiagnosed toddlers, all 50 states, the District of Columbia, Puerto Rico, and the Virgin Islands currently provide universal screening for sickle cell disease. The vast majority of new cases are diagnosed at birth.
41
Sickle Cell
42
Destruction of Red Blood Cells
43
Destruction of Red Blood Cells
• Damaged red blood cells rupture as they pass through the spleen or liver.
• In the liver and spleen, macrophages destroy worn out red blood cells.
• Hemoglobin molecules are broken down into globin and heme groups.
• Heme decomposes into iron and biliverdin.
44
Destruction of Red Blood Cells
• Ferritin is an iron-protein complex that stores iron in the liver.
• Biliverdin is converted to bilirubin.
• Bilirubin and biliverdin are excreted in bile.
• The polypeptide globin chains breakdown into amino acids.
45
White Blood Cells
• leukocytes
• protect against disease
• interleukins and colony-stimulating factors stimulate development
• granulocytes
• neutrophils
• eosinophils
• basophils
• agranulocytes
• lymphocytes
• monocytes
46
47
Neutrophils
• light purple granules in acidbase stain
• lobed nucleus
• other names
• segs
• polymorphonuclear leukocyte
• bands (young neutrophils)
• first to arrive at infections
• phagocytic
• 50% - 70% of leukocytes
• elevated in bacterial infections 48
Eosinophils
• deep red granules in acid stain
• bilobed nucleus
• moderate allergic reactions
• defend against parasitic worm infestations
• 2% - 4% of leukocytes
• elevated in parasitic worm infestations and allergic reactions
49
Basophils
• deep blue granules in basic stain
• release histamine
• release heparin
• less than 1% of leukocytes
• similar to eosinophils in size and shape of nuclei
50
Monocytes
• largest blood cell
• spherical, kidney-shaped, oval or lobed nuclei
• leave bloodstream to become macrophages
• 2% - 8% of leukocytes
• phagocytize bacteria, dead cells, and other debris
51
Lymphocytes
• slightly larger than RBC
• large spherical nucleus surrounded by thin rim of cytoplasm
• T cells and B cells
• important in immunity
• B cells produce antibodies
• 20% - 40% of leukocytes
52
Figure 14.09
53
Figure 14.10
54
Figure 14.11
55
Figure 14.12
56
Figure 14.13
57
Diapadesis
• leukocytes squeeze between the cells of a capillary wall and enter the tissue space outside the blood vessel
58
Cell Adhesion Molecules
• guide cells on the move
• selectin – allows white blood cells to “anchor”
• integrin – guides white blood cells through capillary walls
• important for growth of embryonic tissue
• important for growth of nerve cells
59
3-7
Positive Chemotaxis
• movement of leukocytes toward the damaged tissue region because of the chemicals that were released by damaged cells
60
White Blood Cell Counts
• procedure used to count number of WBCs per cubic millimeter of blood
• 5,000 – 10,000 per cubic millimeter of blood
• leukopenia
• low WBC count (below 5,000)
• typhoid fever, flu, measles, mumps, chicken pox, AIDS
• leukocytosis
• high WBC count (above 10,000)
• acute infections, vigorous exercise, great loss of body fluids
• differential WBC count
• lists percentages of types of leukocytes
• may change in particular diseases
61
White Blood Cell Counts
62
Atypical Lymphocytes
63
The RBCs in the background appear normal. The important finding here is the presence of many PMN's. An elevated WBC count with mainly neutrophils suggests inflammation or infection. A very high
WBC count (>50,000) that is not a leukemia is known as a
"leukemoid reaction". This reaction can be distinguished from malignant WBC's by the presence of large amounts of leukocyte alkaline phosphatase (LAP) in the normal neutrophils.
64
Blood Platelets
• thrombocytes
• cell fragments of megakaryocytes
• 150,000 – 350,000 (approximate) per cubic millimeter of blood
• helps control blood loss from broken vessels
65
Blood Plasma
• straw colored
• liquid portion of blood
• 55% of blood
• 92% water
66
Plasma Proteins
67
Gases and Nutrients
Gases
• oxygen
• carbon dioxide
Nutrients
• amino acids
• simple sugars
• nucleotides
• lipids
68
Nonprotein Nitrogenous
Substances
• molecules containing nitrogen but are not proteins
• urea – product of protein catabolism; about 50% of
NPN substances
• uric acid – product of nucleic acid catabolism
• amino acids – product of protein catabolism
• creatine – stores phosphates
• creatinine
– product of creatine metabolism
•
BUN
– blood urea nitrogen; indicate health of kidney
69
Plasma Electrolytes
• absorbed from the intestine or released as by-products of cellular metabolism
• sodium
• potassium
• calcium
• magnesium
• chloride
• bicarbonate
• phosphate
• sulfate
• sodium and chloride are most abundant
70
Hemostasis
• stoppage of bleeding
Blood Vessel Spasm
• triggered by pain receptors, platelet release, or serotonin
• smooth muscle in vessel contracts
Platelet Plug
Formation
• triggered by exposure of platelets to collagen
• platelets adhere to rough surface to form a plug
Blood Coagulation
• triggered by cellular damage and blood contact with foreign surfaces
• blood clot forms
71
Platelet Plug Formation
72
73
Blood Coagulation
Coagulation
• hemostatic mechanism
• causes the formation of a blot clot via a series of reactions which activates the next in a cascade
• occurs extrinsically or intrinsically
74
Blood Coagulation
Extrinsic Clotting Mechanism
• chemical outside of blood triggers blood coagulation
• triggered by thromboplastin (not found in blood)
• triggered when blood contacts damaged tissue
Intrinsic Clotting Mechanism
• chemical inside blood triggers blood coagulation
• triggered by Hageman factor (found inside blood)
• triggered when blood contacts a foreign surface
75
Blood Coagulation
76
Table 14.09
77
Blood Coagulation
78
79
Figure 14.19b
80
Fate of Blood Clots
•
After forming, a blood clot retracts and pulls the edges of a broken vessel together while squeezing the fluid serum from the clot
•
Platelet-derived growth factor stimulates smooth muscle cells and fibroblasts to repair damaged blood vessel walls
•
Plasmin
– digests blood clots
• thrombus
– abnormal blood clot
• embolus – blood clot moving through blood
81
Prevention of Coagulation
•
The smooth lining of blood vessels discourages the accumulation of platelets and clotting factors
•
As a clot forms, fibrin adsorbs thrombin and prevents the clotting reaction from spreading
•
Antithrombin inactivates additional thrombin by binding to it and blocking its action on fibrinogen
•
Some cells, such as basophils and mast cells secrete heparin (an anticoagulant)
82
Prevention of Coagulation
83
Figure 14.20
84
Antigens and Antibodies
Agglutination – clumping of red blood cells in response to a reaction between an antibody and an antigen
Antigens
– a chemical that stimulates cells to produce antibodies
Antibodies
– a protein that reacts against a specific antigen
85
Antigens and Antibodies
86
Agglutination
87
Agglutination
88
Figure 14.22c
89
Figure 14.22d
90
ABO Blood Group
Based on the presence or absence of two major antigens on red blood cell membranes
• antigen A
• antigen B
91
Questions
• What is the main concern when blood is transfused?
• Why is type AB a universal recipient?
• Why is type O a universal donor?
92
ABO Blood Group
93
Blood Types for Transfusion
94
Questions
• What is the Rh blood group?
• What are ways that Rh incompatibility arise?
95
Rh Blood Group
Rh positive
– presence of antigen D and/or other Rh antigens on the red blood cell membranes
Rh negative
– lack of these antigens
96
Question
• What is erythroblastosis fetalis?
• How is it prevented?
97
Rh Blood Group
98
Clinical Application
Myeloid Leukemia
• bone marrow produces too many immature granulocytes
• leukemia cells crowd out other blood cells
• anemia
• bleeding
• susceptible to infections
Leukemia
Lymphoid Leukemia
• lymphocytes are cancerous
• symptoms similar to myeloid leukemia
Treatments
•
•
• drugs marrow and umbilical cord transplants chemotherapy regimens
99
In contrast to aplastic anemia, leukemia results in a highly cellular marrow. The marrow between the pink bone trabeculae seen here is nearly 100% cellular, and it consists of leukemic cells of acute lymphocytic leukemia (ALL) that have virtually replaced or suppressed normal hematopoiesis. Thus, though the marrow is quite cellular, there can be peripheral cytopenias. This explains the complications of infection (lack of normal leukocytes), hemorrhage (lack of platelets), and anemia (lack of red blood cells) that often appear with leukemia.
100
Figure 14.aa
101
Figure 14.ab
102
Figure 14.a
103
There are numerous granulocytic forms seen here, including immature myeloid cells and bands. This condition is one of the myeloproliferative states and is known as chronic myelogenous leukemia (CML) that is most prevalent in middle-aged adults. A useful test to help distinguish this disease is the leukocyte alkaline phosphatase (LAP) score, which should be low with CML and high with a leukemoid reaction.
104
Here is another view of a peripheral blood smear in a patient with CML. Often, the numbers of basophils and eosinophils, as well as bands and more immature myeloid cells (metamyelocytes and myelocytes) are increased.
Unlike AML, there are not many blasts with CML.
105
Myeloid cells of CML are also characterized by the
Philadelphia chromosome (Ph1) on karyotyping. This is a translocation of a portion of the q arm of chromosome 22 to the q arm of chromosome 9, designated t(9:22).
106
Here are very large, immature myeloblasts with many nucleoli. A distincitve feature of these blasts is a linear red
"Auer rod" composed of crystallized granules. These findings are typical for acute myelogenous leukemia (AML) that is most prevalent in young adults.
107
Leukemias typically fill up the marrow with abnormal cells, displacing normal hematopoiesis. The marrow here is essentially 100% cellular, but composed almost exclusively of leukemic cells. Normal hematopoiesis is reduced via replacement (a "myelophthisic" process) or by suppressed stem cell division. Thus, leukemic patients are prone to anemia, thrombocytopenia, and granulocytopenia and all of the complications that ensue, particularly complications of bleeding and infection.
108
At high power, the bone marrow of a patient with acute myelogenous leukemia is seen here. There is one lone megakaryocyte at the right center.
109
The WBC's seen here are lymphocytes, but they are blasts-very immature cells with larger nuclei that contain nucleoli.
Such lymphocytes are indicative of acute lymphocytic leukemia (ALL). ALL is more common in children than adults. Many cases of ALL in children respond well to treatment, and many are curable.
110
These mature lymphocytes are increased markedly in number. They are indicative of chronic lymphocytic leukemia, a disease most often seen in older adults. This disease responds poorly to treatment, but it is indolent.
111