Metabolism of Xenobiotics Xiao Li Xenobiotics
advertisement

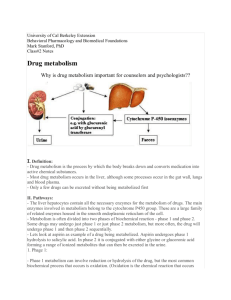
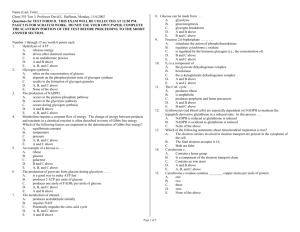
Metabolism of Xenobiotics Xiao Li Introduction ※Xenobiotics: is a compound that is foreign to the body ; is a chemical which is found in an organism but which is not normally produced or expected to be present in body. ※Endogenous: Pigments , hormone ※nonendogenous : Such as drugs , food additives, pollutants, toxin, etc Most of these compounds are subject to metabolism (biotransformation) in human body. Definition of the biotransformation Conversion of lipophilic xenobiotics to water-soluble chemicals by a process catalyzed by enzymes in the liver and other tissues. In most cases, biotransformation lessens the toxicity of xenobiotics, but many must undergo the process to exert their toxic effects. Purpose of biotransformation 1. facilitates excretion: Converts lipophilic to hydrophilic compounds 2. Detoxification/inactivation: converts chemicals to less toxic forms Chronic hepatitis and cirrhosis of liver Hepatic palm Spider lentigo Increase of estrogen, aldosterone and antidiuretin 3. Metabolic activation: converts chemicals to more toxic active forms Detoxification ≠ biotransformation benzpyrene 3,4-Benzypyrene Sites of biotransformation Liver – Primary site! Rich in enzymes – Acts on endogenous and exogenous compounds Extrahepatic metabolism sites – Intestinal wall Sulfate conjugation Esterase and lipases - important in prodrug metabolism – Lungs, kidney, placenta, brain, skin, adrenal glands Knowledge of the metabolism of xenobiotics: rational understanding of pharmacology and therapeutics , pharmacy, toxicology, cancer research , and drug addiction . General Metabolic Pathways Approximately 30 different enzymes catalyze reactions involved in xenobiotic metabolism; however, this note will only cover a selected group of them. It is convenient to consider the metabolism of xenobiotics in two phases – phase Ⅰand phase Ⅱ Phase I reactions ♣♣ Functionalization – Oxidation – Reduction – Hydrolytic reactions Purpose Introduction of polar functional groups in a molecules ♣ Increase a molecule’s polarity ♣ Does provide a site for phase II metabolism Phase II reactions ♣♣ Conjugation ★ Purpose – Introduce highly polar conjugates: ☻☻Glucuronic acid ☻☻ Sulfate – Detoxification Glycine or other Amino Acids (some solubility), Acetyl , Methylations , Glutathione ★ Site of attachment often introduced in Phase I Hydroxyl , Carboxylate , Amino Comparing Phase I & Phase II Enzyme Phase I Phase II Types of reactions Hydrolysis Oxidation Reduction Small Conjugations Exposes functional group Polar compound added to functional group May result in metabolic activation Facilitates excretion Increase in hydrophilicity General mechanism Consquences Large Phase Ⅰ: Oxidation 1. Hydroxylation RH + O2 + NADPH + H+ R-OH + H2O + NADP+ Addition of an oxygen atom or bond Require NADH or NADPH and O2 as cofactors RH: drugs, cacinogens, pesticides, petroleum products, pollutants, steroids, eicosanoids, fatty acids, retinoids, etc. Enzyme: Cytochrome P450s-dependent monooxygenase Hydroxylation:O2 * It has been shown by the use of O2 that one atom of oxygen enters R-OH and one atom enters H2O. * This dual fate of the oxygen accounts for the former naming of monooxygenases as “mixedfunction oxidases”. RH + O2 + NADPH + H+ R-OH + H2O + NADP+ Cytochrome P450s-dependent monooxygenase -----the most versatile biocatalyst ----Works on a large number of diverse compounds ★ Microsomal drug oxidations require cytochrome P450, cytochrome P450 reductase, NADPH , & O2 The actual reaction mechanism is as follows: Cytochrome P450s-dependent monooxygenase CYP or Cytochrome P-450 ★ Heme proteins ★ Iron containing porphyrin - binds O2 What is a Heme Protein? Cytochrome P-450, Hemoglobin, & Myoglobin ALL Heme Proteins! ★ The name cytochrome P450 is derived from the spectral properties of this hemoprotein in its reduced (ferrous, Fe2+) form, it binds CO to give a complex that absorbs light maximally at 450 nm Cytochrome P-450 Enzymes isolated by disruption of the liver cells – Endoplasmic reticulum - microsomes when disrupted – Enzymes are membrane bound – Explains why lipophilic drugs are processed – Catalytic process heme binds O2 Cytochrome P450: Isozymes ★ Isozymes - multiple forms of an enzyme ★ Supergene family - More than 8,000 P450 genes as of November/2007 - More than 368 gene families, 814 subfamilies - Human: 18 families, 43 subfamilies, 57 sequenced genes ★ Nomenclature CYP1A2 family subfamily individual member of that subfamily Cytochrome P450 This enzyme is very important. approximately 50% of the drugs that humans ingest are metabolized by isoforms of cytochrome P450. These enzymes also act on various carcinogens and pollutants. Substrates CH Allyl H2 C Vinyl Aromatic Benzyl Aliphatic Alicyclic 2. Monoamine oxidase, MAO RCH2NH2+O2+H2O2 RCHO+NH3+H2O ★ MAO catalyze the oxidative deamination of monoamines. ★ Oxygen is used to remove an amine group from a molecule, resulting in the corresponding aldehyde and ammonia. ★ MAO are found bound to the outer membrane of mitochondria in most cell types in the body. They belong to protein family of flavin containing amine oxidoreductases. 3. ADH and ALDH ADH alcohol dehydrogenase ALDH aldehyde dehydrogenase Alcohol Dehydrogenase belongs to the oxidoreductase family of enzymes. high concentrations within the liver and kidney. Function The primary and most common role of ADH in humans is to detoxify incoming ethanol by converting it into aldehyde. The resulting aldehyde, a more toxic molecule than ethanol, is quickly converted into acetate by aldehyde dehydrogenase (ALDH) and other molecules easily utilized by the cell. ALDH ADH NAD+ R CH2OH NADH NAD+ R CHO NADH R CO2H ADH NAD+ R CH2OH ALDH NADH NAD+ R CHO NADH R CO2H During this reaction, hydrogen is removed from the alcohol and transferred to a molecule called nicotinamide adenine dinucleotide (NAD), converting it to reduced NAD (NADH). NADH participates in numerous other metabolic reactions, passing on the hydrogen to other compounds or electron transfer chain. Absorption 20% Soluble in water Small size - penetrates everywhere, easily crosses all bio membranes 80% Rapidly absorbed from GI In people who consume alcohol at moderate levels and/or only occasionally, most of the alcohol is broken down by ADH and ALDH. after higher alcohol consumption, The MEOS plays a role in alcohol metabolism. CH3CH2OH + NADPH + O2 + + NADP+ + 2H2O CH3CHO ALDH H+ MEOS CH3CHO CH3COOH MEOS: Microsomal Ethanol-Oxidizing System , is also called Cytochrome P450-dependent Microsomal Ethanol Oxidizing System. converts alcohol to acetaldehyde CH3CH2OH + NADPH + O2 + + NADP+ + 2H2O H+ MEOS CH3CHO This reaction also relies on oxygen and NADPH, and results in the formation of NADP and water. ◆consume oxygens of liver and NADPH ◆ As byproducts of these reactions, oxygen radicals or reactive oxygen species (ROS) are generated. These ROS can contribute to liver damage through a variety of mechanisms. Although the rate at which ADH breaks down alcohol generally stays the same, the activity of the MEOS can be increased (induced) by alcohol consumption. Because the MEOS metabolizes not only alcohol but also other compounds (certain medications), enhanced MEOS activity resulting from high alcohol consumption also can alter the metabolism of those medications. This may contribute to harmful interactions between alcohol and those medications or otherwise influence the activity of those medications. Alcoholism leads to fat accumulation in the liver, hyperlipidemia, and ultimately cirrhosis. Phase Ⅰ: Reduction 4. Nitro and Azo Reduction • NADPH dependent microsomal and nitro-reductase enzymes. • Bacterial reductases play a role in enterohepatic recirculation of nitro or azo containing drugs. + O Ar N O Ar N N Ar' Ar N O Ar N N Ar' H H Ar NHOH H2N Ar Ar NH2 + H2N Ar' 2005 , sudan red incident chili patse sudan red nitroreductase chloromycetin Phase Ⅰ: Reduction 5. Hydrolysis Substrates: esters , amide , glycoside, etc. Catalyzed by widely distributed hydrolytic enzymes Hydrolysis of esters major metabolic pathway for ester drugs ☻Non-specific esterases (liver, kidney, and intestine) ☻Plasma pseudocholinesterases also participate Acetylsalicylic Acid, ASA CO2H O esterase CH3 CO2H OH CH3 O O salicylic acid ASA HO Phase II: Conjugation In phase Ⅰ reactions, xenobiotics are generally converted to more polar, hydroxylated derivatives. In phase Ⅱ reactions, these derivatives are conjugated with molecules such as glucuronic acid, sulfate, or glutathione. This renders them even more water-soluble, and they are eventually excreted in the urine or bile. xenobiotic Phase I Phase II Protection Elimination excrection Reactive metabolite Cell injury Antibody product Cell injury nontoxic metabolite mutation cancer Five types of phase II reactions A. B. C. D. E. Glucuronidation Sulfation Conjugation with glutathione Acetylation Methylation 1. Glucuronidation the most frequent conjugation reaction. UDP-glucuronic acid (UDPGA) is the glucuronyl donor UDP-glucuronyl transferases (UGT), present in both the endoplasmic reticulum(ER) and cytosol, are the catalysts. – Liver, lung, kidney, skin, brain and intestine Attachment sites are hydroxyls – Alcohols, phenols, enols, N-hydroxyls, acids Oxygen site often from Phase I Oxygen glucuronides cont… Alcohol hydroxyl example OH OH Cl H N O 2N O 2N Cl HO HO Chloramphenicol - Chloromycetin® - O HO HO H Phenol hydroxyl example CH3 CH3 O O NH NH HO2C OH Acetaminophen APAP N-acetyl-p-aminophenol HO HO Cl O HO 2C O Cl H N O HO H O O 2. Sulfate Conjugation Some alcohols, arylamines, and phenols are sulfated. Catalyzed by sulfotransferases – liver, kidney and intestine Sulfate donor: adenosine 3’-phosphate-5’-phosphosulfate (PAPS); this compound is called “active sulfate.” Leads to inactive water-soluble metabolites Glucuronate conjugation often more competitive process HX Drug sulfotransferase PAPS O O -O S O P O O OH H2O3PO O Adenine OH O -O S O X Drug Sulfate Conjugation O O +PAPS +PAP HO 3SO HO estrone sulfate estrone CH3 HO HO H2N CO2H alpha-Methyldopa Aldomet® - Merck Antihypertensive O -O S O O HO CH3 H2N CO2H 3. Conjugation with glutathione glutamic acid, cysteine, R + GSH GST glycine R-S-G where R= an electrophilic xenobiotics R: epoxides and halogenides GST: Glutathione S-Transferases (Liver and kidney) Glutathione (GSH) Conjugation DETOXIFICATION of electrophiles! Electrophilic chemicals cause: – Tissue necrosis – Carcinogenicity – Mutagenicity – Teratogenicity The thiol (SH group) ties up potent electrophiles Glutathione S-transferase (+)benzo[a]pyrene7,8-dihydrodiol9-10-epoxide HO GST HO OH DNA reactive; + glutathione HO Inactive lung and skin tumors DETOXIFICATION Glutathione (GSH) Conjugation Epoxide or an Arene Oxide oxidation Benzene O H+ aflatoxin b-1 epoxide SG HSG OH 4. Acetylation X + Acetyl-CoA - - - - >Acetyl-X + CoS where X represents a xenobiotics. (for: aromatic amines) • Enzyme: acetyltransferases • present in the cytosol of various tissues, particularly in liver. isoniazid sulfanilamide Important for drugs with primary amino groups Generally, metabolites are nontoxic and inactive Acetylation does NOT increase water solubility Detoxification or termination of drug activity Methylation A few xenobiotics are subject to methylation by methyltransferase, emplyoing S-adenosylmethione(SAM) as the methyl donor. SAM catechol Metabolism via Methylation Key for biosynthesis of many compounds Important in the inactivation of physiologically active biogenic amines neurotransmitters – norepinephrine, dopamine, serotonin, histamine Minor pathway in the metabolism of drugs Methylation does NOT increase water solubility Most methylated products are inactive Factors that influence metabolism Age – older people less efficient at metabolism Sex – Linked to hormonal differences Heredity – Genetic differences can influence amounts and efficiency of metabolic enzymes Disease states – Liver, cardiac, kidney disease Summary Xenobiotic, Biotransformation Phase I reactions: – Purpose: – Functionalization: Enhances elimination Converts chemical to less toxic forms (detoxification) Converts chemicals to more toxic active forms (activation) Oxidation: monooxygenase, CYP450 Reduction: ADH, ALDH Hydrolytic reactions: esterase Phase II: Conjugation Rx – – Purpose: more water-soluble, excreted in the urine or bile Functionalization: Glucuronidation, Sulfation, Conjugation with glutathione, Acetylation, Methylation ALCOHOL Mechanism of Fatty Liver The likelihood of hypoglycemia is also increased in alcoholics when they fast, as they often have low hepatic stores of glycogen because of poor nutrition. The shift in the NADH/NAD+ ratio also inhibits β-oxidation of fatty acids and promotes triglyceride synthesis; this increases hepatic synthesis of VLDL, and the remaining excess triglyceride is deposited in the liver.