Introduction of current development and concept
advertisement

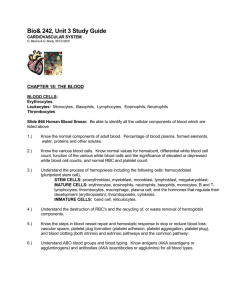
Introduction of current development and concept cardiovascular physiology and pharmacology Mohammad Saifur Rohman, MD. PhD. FIHA Lab. Cardiology and Vascular Medicine Faculty of Medical, Brawijaya University Outline • Physiology of CV • Pathogenesis of CV • Current development and concepts of CV drugs Blood Flow Through Heart Blood Flow Through and Pump Action of the Heart Coronary Arteries • Originates from the aorta just beyond the aortic valve • Coronary blood flow to the myocardium occurs primarily during diastole * To maintain adequate blood flow through the coronaries, mean arterial pressure (MAP) must be at least 60 mmHg Intrinsic Cardiac Conduction System Approximately 1% of cardiac muscle cells are autorhythmic rather than contractile 70-80/min 40-60/min 20-40/min Type of Cells in The Heart • Pacemaker cells • – 5 – 10 um in length; • Sinoatrial and atrioventricular nodes • – Spontaneous depolarization • – Action Potential • Electrical conducting cells • – Long thin cells • Atrial conducting system • Ventricular conducting system • Myocardial cells • – Contractile units in the heart, most are myocardial cells • – Calcium is responsible for contractile process after initiation of action potential Physiology of the Heart • Electrophysiologic properties (regulates heart rate & rhythm) - Automaticity – ability of all cardiac cells to initiate an impulse spontaneously & repetitively - Excitability – ability of cardiac cells to respond to stimulus by initiating an impulse (depolarization) - Conductivity – cardiac cells transmit the electrical impulses they receive - Contractility – cardiac cells contract in response to an impulse - Refractoriness – cardiac cells are unable to respond to a stimulus until they’ve recovered (repolarized) Ion movement and channels • The movement of specific ions across the cell membrane serve as action potentials depends on : • 1. Energetic favorability; concentration gradient and transmembrane potential • 2. Permeability of the membrane for the ion: channels which is selective and gated • Selective: manifestation of size and structure of its pore • Gated: pass through it specific channels only at certain times; voltage sensitive gating (fast sodium channel) Action potential in autorhythmic cells Action Potential in contractile cells Different pattern of Membrane potential at different cells Action Potential in contractile cells and ECG Heart Excitation Related to ECG P wave: atrial depolarization START P The end R PQ or PR segment: conduction through AV node and A-V bundle T P P QS Atria contract. T wave: ventricular Repolarization Repolarization R T P ELECTRICAL EVENTS OF THE CARDIAC CYCLE QS P Q wave Q ST segment R R wave R P QS P R Ventricles contract. Q P S wave QS Cardiac Cycle - Filling of Heart Chambers • Heart is two pumps that work together, right and left half • Repetitive contraction (systole) and relaxation (diastole) of heart chambers • Blood moves through circulatory system from areas of higher to lower pressure. – Contraction of heart produces the pressure Cardiac Cycle - Mechanical Events 1 START 5 4 Isovolumic ventricular relaxation: as ventricles relax, pressure in ventricles falls, blood flows back into cups of semilunar valves and snaps them closed. Ventricular ejection: as ventricular pressure rises and exceeds pressure in the arteries, the semilunar valves open and blood is ejected. Late diastole: both sets of chambers are relaxed and ventricles fill passively. Atrial systole: atrial contraction forces a small amount of additional blood into ventricles. 2 3 Isovolumic ventricular contraction: first phase of ventricular contraction pushes AV valves closed but does not create enough pressure to open semilunar valves. Figure 14-25: Mechanical events of the cardiac cycle Wiggers Diagram 0 100 200 Time (msec) 300 400 QRS complex Electrocardiogram (ECG) P 500 600 700 800 QRS complex Cardiac cycle T P 120 90 Dicrotic notch Pressure (mm Hg) Left ventricular pressure 60 30 Left atrial pressure S1 Heart sounds S2 EDV 135 Left ventricular volume (mL) Atrial systole ESV 65 Atrial systole Isovolumic ventricular contraction Ventricular systole Ventricular systole Ventricular diastole Early ventricular diastole Atrial systole Late ventricular diastole Atrial systole Modulation of Cardiac Contractions Regulation of Cardiac Output Figure 18.23 Normal Endothelial Function Endothelial Dysfunction : Atherogenesis Atorvastatin calcium Extensively Studied in Large Trials Atorvastatin effectively reduces LDL-C Across a Broad Range of Patients 10 mg 10,305 patients without CHD in ASCOT-LLA LDL-C level at randomisation Follow-up LDL-C level Outcomes 133 mg/dL 90 mg/dL • 36% RRR of nonfatal MI and fatal CHD • 27% RRR of stroke 80 mg* 2838 patients 10,001 patients 654 patients 4162 patients in CARDS in TNT in REVERSAL in PROVE IT <130 mg/dL 150 mg/dL 106 mg/dL with diabetes 116 mg/dL 77 mg/dL • 37% RRR of death and major CV events • 48% RR of stroke with CHD 77 mg/dL • 22% RR of major CV events • 25% RR of stroke with CHD with CHD 79 mg/dL 62 mg/dL Significantly impacted atherosclerotic disease progression; pravastatin was associated with further disease progression • 16% RR of major CV events versus pravastatin *80 mg is not a starting dose. RR=risk reduction. Nissen et al. JAMA. 2004;291:1071-1080; Cannon et al. N Engl J Med. 2004;350:1495-1504; LaRosa et al. N Engl J Med. 2005;352:1425-1435; Sever et al, for the ASCOT Investigators. Lancet. 2003;361:1149-1158; Colhoun et al. Lancet. 2004;364:685-696. Atherosclerosis ACS STEACS vs. NSTACS Occluded artery ECG featured of Ischemic cell Arrhythmias Detected on ECG continued • In third-degree or complete AV node block, no atrial activity passes to ventricles – Ventricles are driven slowly by bundle of His or Purkinjes Therapeutic Options in Acute Coronary Syndromes • • • • • Anti-ischemic treatment Antiplatelet agents Anticoagulants Revascularization/Reperfusion/Thrombolysis Long term treatment/secondary prevention Targets for anti thrombotics Tissue factor Collagen Aspirin Plasma clotting ADP cascade Thromboxane A2 Direct Xa inhib LMWH Heparin Prothrombin AT Factor Xa Bivalirudin Hirudin Dabigatran Clopidogrel Prasugrel AZD 6140 Conformational activation of GPIIb/IIIa Thrombin Fibrinogen GPIIb/IIIa inhibitors Platelet aggregation Fibrin Thrombus NSTE-ACS : Antiplatelets What, when and How? What? Invasive 1,2 Conservative 2 Aspirin Ticagrelor* / Clopidogrel‡ Aspirin Ticagrelor* / Clopidogrel‡ When ? How ? Loading dose ASAP Aspirin: started at a dose of 150–300 mg and at a maintenance dose of 75–100 mg, plus Ticagrelor: 180 mg LD, 90 mg twice daily, or Clopidogrel: 300 or 600 mg LD, 75 mg daily Upstream GPIIbIIIa are not recommended in patients with high ischaemic risk ‡All patient received clopidogrel LD before PCI in CURRENT * Ticagrelor has limited experience for prePCI loading 1. Wijns W et al Eur Heart J 2010;31:2501-55 2. Hamm CW et al ESC NSTE-ACS Guidelines EHJ 2011; doi:10.1093/eurheartj/ehr236 3. Anderson JL et al Circulation 2007;116:148-304 Aspirin: started at 150–300 mg and at a maintenance dose of 75–100 mg, plus Ticagrelor 180 mg LD, 90 mg twice daily, or Clopidogrel: an immediate 300 mg LD, 75 mg daily dose ST-ACS: Oral antiplatelet What, when and how ? What ? Primary PCI1 Thrombolysis2 Aspirin Clopidogrel / Prasugrel* / Ticagrelor* Aspirin Clopidogrel When ? How? ASAP Aspirin: mulai 150–300mg per oral or 250–500mg bolus iv dilanjutkan dengan 75-100mg/hari Prasugrel: 60mg Loading dilanjutkan 10mg /hari atau Ticagrelor: 180mg Loading dilanjutkan 2x90mg/ hari atau Clopidogrel: 600mg Loadingdilanjutkan 75mg /hari 1. Wijns W et al Eur Heart J 2010;31:2501-55 2. Van de Werf F et al Eur Heart J 2008;29:2909-45 Aspirin: 150-325mg per oral or i.v. 250mg iika tidak mungkin per oral. Clopidogrel: loading 300mg jika usia ≤75 tahun; 75mg jika usia >75 tahun ESC Guidelines Doses of antiplatelet and antithrombin co-therapies ESC Guidelines for the management of AMI in patients presenting with ST-segment elevation, 2012 Contractile Dysfunction in IHD Myocardial ischaemia Oxygen Supply and Demand Are Mismatched During Leading to Impaired Diastolic Relaxation Vasospasm X Thrombus Atherosclerosis Diltiazem, Amlodipine, Nicorandil, Nitrates β-Blockers, Verapamil/Diltiazem, Ivabradine Microvascular Flow O2 Supply Ischaemia , Afterload X Heart X rate Contractility X Preload O2 Demand β-Blockers, Verapamil/Diltiazem Ischaemia β-Blockers, Calcium Antagoni - Induced Sodium Calcium Overload Relaxation Impaired Diastolic Adapted from Chaitman BR. Circulation 2006;113:2462 -72. Adapted from Belardinelli L et al. Eur Heart J 2004;6(Suppl I):I3 -7. Diastolic Wall Tension New Approach of Ischemic Heart Disease Traditionally, ischemic heart disease is treated by pharmacological or mechanical means that act primarily either to increase oxygen supply to the heart or to decrease oxygen demand of the heart muscle Recently, an additional approach to treating ischemic heart disease is by means of metabolic modulation, whereby optimizing energetics in the myocardium can improve cardiac efficiency of the heart muscle 1. Ussher JR. et al. Basic Res Cardiol. 2009;104:203–10. 2. Stanley WC et al. Physiol Rev. 2005;85:1093–129. 3. Lam A et al. Curr Opin Pharmacol. 2007;7:179–85. New mechanistic approaches to chronic stable angina Rho kinase inhibition (fasudil) Metabolic modulation (trimetazidine) N SO2 N CH3 CH3 NH O N O H O CH3 N CH3 N O CH3 H N O CH3 H O NO2 N O Late INa inhibition (ranolazine) CH3 H Preconditioning (nicorandil) H3 C O H3 C O O N Sinus node inhibition (ivabradine) N CH3 O OH N N OCH3 O NEW CONCEPT IN CARDIAC METABOLISM Former concept (in past decades): Chronic heart failure associated with chronic coronary artery disease (CAD) is irreversible It should be treated with hemodynamic agents New concept (progress in cardiac imaging techniques): CHF associated with chronic CAD is reversible Cause of reversible left ventricle dysfunction is Hibernation and Stunning It highlights the impact of metabolic changes Energy Utilization in Ischemia Classification of Blood Pressure ESC-ESH 2007 JNC-VII Optimal : <120 and < 80 Normal : 120-129 and/or 80 - 84 High Normal : 130-139 and/or 85-89 Grade 1 : 140-159 and/or 90-99 Grade 2 : 160-179 and/or 100-109 Grade 3 : > 180 and/or > 110 Normal Pre-hypertension Stage 1 Stage 2 H Y P E R T E N S I O N JNC VII committee, JAMA 2003: 289;2560-2572 History of Hypertension Management • Hypertension: entered the language of medicine in the 19th and early 20th centuries. • The history of hypertension can be divided into two eras: 1. Pre-treatment Era (before 1967) 2. Treatment era (established the benefit of drug therapy for hypertension) Krakoff LR. Et al. Boca Raton; Taylor & Francis Group, 2005: 3-14. Pretreatment During the first 120 years of hypertension research (from the 1840s to 1965) basic and clinical research defined the following (1): 1. The mechanisms of increased BP 2. The natural history of untreated HTN to CVD 3. Causes of secondary HTN 4. Set the stage for recognizing potential therapy through drug treatment Non farmacological treatments: Phlebotomy, purgatives Loss of Water and sodium (2) 1. Krakoff LR. Et al. Boca Raton; Taylor & Francis Group, 2005: 3-14. 2. Hoobler SW. Hoeber-Harper Book, N York 1959 Diet for HTN Krakoff LR. Et al. Boca Raton; Taylor & Francis Group, 2005: 3-14. Surgical (Sympathectomy) for HTN Krakoff LR. Et al. Boca Raton; Taylor & Francis Group, 2005: 3-14. Farmacotherapy for HTN Krakoff LR. Et al. Boca Raton; Taylor & Francis Group, 2005: 3-14. Regulation of BP Excess sodium intake Renal Sodium retention Reduced Nephron number Stress Decreased Sympathetic Filtration nervous overactivity surface Fluid Volume Preload Venous Constriction Contractility Genetic Alteration Endothelium derived factors Renin Angiotensin Excess Hyperinsulinemia Cell membrane alteration Functional Constriction Structural Hypertrophy Blood Pressure = Cardiac Output (CO) X Peripheral Resistance (PR) Hypertension Increased CO and/or Increased PR Autoregulation Kaplan NM, Clinical Hypertension 7th ed. 2002; 63 Obesity Krakoff LR. Et al. Boca Raton; Taylor & Francis Group, 2005: 3-14. LIFESTYLE MODIFICATIONS Not Goal BP INITIAL DRUG CHOICES Without Compelling Indications Stage 1 Stage 2 Thiazide-Type diuretics for most. May consider ACEI, ARB, BB, CCB, or combination Two –Drug combination for most (usually thiazide-type diuretic and ACEI, or ARB, or BB, or CCB With Compelling Indications Drug(s) for the compelling indications. Other antiHT Drugs (Diuretics, ACEI, ARB, , CCB) as needed US-JNC VII Report Clinical Trial and Guideline Basis for Compelling Indications (JNC VII 2003) Aldo Ant CCB ARB ACEI BB Compelling Indication* Diuretic Recommended Drugs Clinical trial basis Heart Failure ACC/AHA Heart Failure Guideline, MERITHF, COPERNICUS, CIBIS, SOLVD, AIRE, TRACE, ValHEFT, RALES, CHARM Postmyocardial Infarction ACC/AHA Post-MI Guideline, BHAT, SAVE, Capricorn, EPHESUS High Coronary Disease Risk ALLHAT, HOPE, ANBP2, LIFE, CONVINCE, EUROPA, INVEST Diabetes NKF-ADA Guideline, UKPDS, ALLHAT Chronic Kidney Disease NKF Guideline, Captopril Trial, RENAAL, IDNT, REIN, AASK Recurrent Stroke Prevention PROGRESS Amlodipine besylate Extensively Studied in Large Trials ALLHAT ASCOT-BPLA VALUE CAMELOT/ NORMALISE Patients studied High-risk hypertensive (N=33,357) High-risk hypertensive (N=15,245) CHD patients (n=1991) Comparators Amlodipine besylate, lisinopril, chlorthalidone Amlodipine besylate, valsartan Amlodipine besylate, enalapril, placebo Trial duration 6 years Moderate-risk hypertensive (N=19,342) Amlodipine besylate perindopril, atenolol thiazide Trial stopped early 6 years 2 years End point: cardiac morbidity and mortality End point: CV events and plaque progression End points: CHD death and nonfatal MI ALLHAT Collaborative Research Group. JAMA. 2002;288:2981-2997; Julius et al, for the VALUE trial group. Lancet. 2004;363:2022-2031; Sever et al, for the ASCOT Investigators. J Hypertens. 2001;19:1139-1147; Nissen et al, for the CAMELOT Investigators. JAMA. 2004;292:2217-2226. Emerging Role of Gene in HTN Gene Polymorphism : • Aldosteron synthase • Angiotensin • Epithelial sodium transport (Liddle’s syndrome) • Amiloride sensitive sodium channel • WNK kinase system Krakoff LR. Et al. Boca Raton; Taylor & Francis Group, 2005: 3-14. Single Nucleotide Polymorphism Consequence of Gene Polymorphism • Gene polymorphism A large, prospective study published on July 2009 in JACC : Differences in beta-blocker effectiveness and variability in beta-blocker responses among African Americans attributed to polymorphisms that affect beta receptors • Pharmacogenomic • Different response to drug may be correspond to ethnic/race and familial Krakoff LR. Et al. Boca Raton; Taylor & Francis Group, 2005: 3-14. Different Combination of Treatment ? • Race base therapy, raise from a difference response of HTN treatment between white and black • Indonesian are White or Black? • Specific race researches are warranted to achieve blood pressure target worldwide. Krakoff LR. Et al. Boca Raton; Taylor & Francis Group, 2005: 3-14. Respond to the same antihypertensive drug ? The Progression from Hypertension to Heart Failure LVH Diastolic dysfunction CHF Hypertension Systolic dysfunction MI LV Normal LV Structure & Function remodeling Time (decades) Death Subclinical Overt LV dysfunction Heart Failure Time (months) Vasan RS, Levy D. 1996. Arch Intern Med 156 : 1759-1796 The Cardiovascular Continuum Coronary thrombosis Myocardial infarction Myocardial ischaemia CAD Atherosclerosis LVH Risk factors Hypertension, smoking, cholesterol, diabetes Sudden Death Arrhythmia & loss of muscle Remodelling Ventricular dilatation Congestive heart failure Death Dzau V. Braunwald E, Am Heart J. 1991 THE DONKEY ANALOGY Ventricular dysfunction limits a patient's ability to perform the routine activities of daily living… HEART FAILURE ERAS OF HEART FAILURE MANAGEMENT Non-pharmacological • Bed rest Pharmacological • Gene therapies • Digitalis • Inactivity • Fluid restriction • (Digitalis, diuretics) pre -1980’s Cellular/genetic 1980’s • Diuretics • Cell implantation/ regeneration • Neurohormonal interventions • Xenotransplantation 1990’s 2000’s 2020’s ⇒ Pharmacological Device • Digitalis • CRT • Diuretics • ICDs • Vasodilators • LVADs • Inotropes • Others? Heart Failure Updates, 2003 TREATMENT OPTION FOR HF INOTROPIC Like the carrot placed in front of the donkey ACEI AND DIURETICS Reduce the number of sacks on the wagon Nowtreatment previously Preferred Heart Failure Myocardial Infarction ACE-I B Blocker ß-BLOKERS Limit the donkey’s speed, thus saving energy ACTIVATION OF NEUROHORMONAL PATHWAYS IN HF Coronary Disease Cardiomyopathy Cardiac Overload Left Ventricular Dysfunction Vasoconstriction Neurohormonal Activation • Cathecholamines • RAAS • AVP • Endothelin Peripheral organ blood flow Cardiac remodelling Skeletal muscle flow Exercise intolerance Na+ RBF retention Edema, congestion LV dilatation Sudden death LV hypertrophy Pump failure Ruffolo, J.Cardiovasc Pharmacol,1998 Renin-Angiotensin-System Blockers Liver Kidney Angiotensinogen X Renin Bradykinin ACE inhibitors X Angiotensin I X ACE Inactive kinins Direct Renin Inhibitor Angiotensin II X Retention of salt and water Vasoconstriction Blood pressure increases Kaplan NM, Clinical Hypertension 7th ed. 2002; 63 ACE inhibitors (ACEi) Angiotensin II Receptor Blokers (ARB) Inhibition of the RAAS by ACE inhibitors Angiotensinogen (-) ACE inhibitor Renin Bradykinin Angiotensin I Nonrenin Angiotensinconverting enzyme NonACE Inactive kinins Angiotensin II ARB BP AT1 • Vasoconstriction • Aldosterone secretion • Catecholamine release • Proliferation • Hypertrophy Ellis ML, et al. Pharmacotherapy 1996;16:849-860; Carey RM, et al. Hypertension 2000;35:155-163 AT2 • • • • • Vasodilation Inhibition of cell growth Cell differentiation Injury response Apoptosis ACEI Reduced Mortality and Morbidity Trials Mortality Reduction Sample Size Follow up SAVE 2.231 AMI 24-60 months SOLVD 4.228 without, 2568 with overt HF > 3 years 8-16 % AIRE 2.006 AMI with HF 15 months 18-30% TRACE 1.h749 AMI with LV dysfunction 24-50 months ATLAS 3.164 CHF 39-58 months GISSI3 18.895 AMI 6 weeks Morbidity Reduction 19-32% Recurent MI 25% Overt HF 29%, Remodeling Prevented progression to severe heart 7.60% failure 8% Hospitalization 16-14% 6.70% Whats what 2006 ADRENERGIC ACTIVATION IN MYOCARDIAL DYSFUNCTION Myocardial Insult Myocardial Dysfunction Increased Load Reduced Systemic Perfusion Cardiac Adrenergic Activation Altered Gene Expression Growth and Remodeling Toxicity, Ischemia, or Energy Depletion Necrosis Apoptosis Cell Death Bristow MR. Am J Cardiol 1997;80(11A):26L-40L 1.0 100 CIBIS-II COPERNICUS Bisoprolol Survival (%) 0.8 Placebo Risk reduction = 34% 80 Carvedilol (n=1156) 70 Placebo (n=1133) 35% risk reduction p < 0.0001 p 0.001 0.6 60 0 0 0 200 400 600 0 800 Days after inclusion 3 CIBIS-II Investigators (1999) Placebo Metoprolol CR/XL Cumulative mortality (%) 6 9 12 15 Months of follow up 20 15 MERIT-HF 10 5 Risk reduction = 34% p = 0.0062 0 0 3 6 9 12 Follow up (months) 16 18 21 MERIT-HF Study Group.(1999) Survival 90 18 21 Packer et al. 2001 -Blockers in Heart Failure All-Cause Mortality -BLOCKER THERAPY ON SURVIVAL IN CHF NYHA II CIBIS II MERIT-HF US Carvedilol program NYHA III NYHA IV Ischemic Level of Evidence A Non ischemic 0 0.5 1 Relative Risk 1.5 95% CI 2 Compliance at 1 year with antihypertensive treatment Compliance at 1 year (%) 70 60 64 * * p<0.007 vs ACE inhibitors 58 50 50 40 43 38 30 20 10 0 Diuretics Beta-blockers CCBs ACE, angiotensin-converting enzyme; CCB, calcium-channel blocker; ARB, angiotensin II receptor blocker ACE inhibitors ARBs Bloom BS, et al. Clin Ther 1998;20:671-681 IC50 (nM) Olmesartan has greater binding affinity for the AT1 receptor than losartan 100 90 80 70 60 50 40 30 20 10 0 92 16 8 Olmesartan Losartan EXP3174 12 Candesartan Koike H, et al. J Hypertens 2001;19(suppl 1):S3-S14 IC50: the lower the IC50, the greater the binding affinity These results were found in a rat study and may not be reflected in humans Change from predose to 24 hours in mean PRA (ng/mL/h) Olmesartan may give more prolonged AT1 blockade than irbesartan or valsartan 5 p vs placebo 4 <0.0001 p vs olmesartan 0.005 0.058 (NS) 0.004 0.028 0.002 0.036 3.16 n=20 3 1.84 1.78 2 1.19 1 0 0 Placebo Olmesartan Irbesartan 40 mg 300 mg PRA, plasma renin activity Performed in healthy volunteers in 1-dose study; PRA response may not predict those in hypertensive patients Valsartan 160 mg Valsartan 320 mg Jones M, et al. Presented at ASH 2006; Abstract P-195 Lower pill burden: better adherence As the number of pre-existing Rx meds increased, the likelihood of adequately refilling AHT and LLT decreased Likelihood of achieving adherence Number of pre-existing Rx medications 0.0 0.5 1.0 1.5 2.0 2.5 Adjusted odds ratio for adherence to both AHT and LLT* (PDC ≥80%) (95% confidence interval) 1.00 (reference group) ≥6 3-5 1.23 (1.10-1.38) 2 1.30 (1.14-1.49) 1 1.61 (1.40-1.84) 0 1.96 (1.72-2.25) Lesser Greater *P<0.001 for all groups versus reference group. Retrospective cohort study of a managed care population. N=8406 patients with hypertension who added AHT and LLT to existing Rx meds within a 90-day period. Adherence to concomitant therapy: sufficient AHT and LLT Rx meds to cover ≥80% of days per 91-day period. Chapman RH, et al. Arch Intern Med. 2005;165:1147-1152. Fixed Dose Combination Patients fully compliant (%) Cohort study of general practice research data (N=755) 100 Fixed-dose combination therapy 80 Co-administration of two pills 60 40 20 0 17% 21% 0 3 6 9 12 15 18 21 24 27 Months since start of therapy Patients on free combination had a higher odds ratio (OR) of being non-compliant than patients on FDC: OR 2.09 (95% CI: 1.69, 2.59) Summary • Rapid acceleration of current concepts and drug development in CV = Molecular Cardiovascular research • 1 drug = certain target (pleotropic effect) • Complex disease= multi drug=poly pill • Fixed dose combination technology • 3x1x, Pharmacokinetic/ Pharmacodynamic