Maternal Newborn (JO)
advertisement

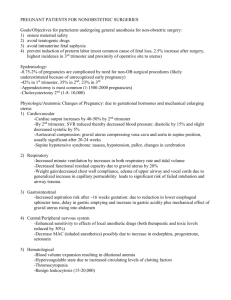
Maternity Introduction to Maternity & Pediatric Nsg; Leifer, 7th ed., Ch. (1, 2, 3 review), 4, 6, 7, 8 1. Discuss stages of fetal development. 2. Discuss major functions of each reproductive structure. 3. Explain expected Δ’s in the major body systems during pregnancy. 4. Describe diagnostic tests & estimating due dates. 5. Describe the 4 components of the birth process. 6. Explain the normal processes of childbirth: premonitory signs, mechanisms of birth & stages & phases of labor. The Present: Maternity https://www.youtube.com/watch?v=q0NRngqwqEg • Family involvement during pregnancy & birth • Necessary for bonding & support Hospitals • 3 separate sections of the maternity unit • Labor-delivery • Postpartum • Newborn nursery • Some facilities have merged all 3 areas into 1 Birthing Centers • Provide comprehensive care • Antepartum • Labor-delivery • Postpartum • Mothers’ classes • Lactation classes • Follow-up family planning Midwives • First school of nurse-midwifery • Opened in NYC, 1932 • Certified Nurse-Midwife (CNM) • RN • Graduate from an accredited midwife program • National certification • Provides comprehensive prenatal & postnatal care • Attends uncomplicated deliveries Advanced-Practice Roles in Maternity & Pediatric Nursing • Certified Nurse Midwife (CNM) • Clinical Nurse Specialist (CNS) • Neonatal Nurse Practitioner (NNP) • Pediatric Nurse Practitioner (PNP) • School Nurse Practitioner • Family Nurse Practitioner (FNP) Female Reproductive System Uterus • Pear-shaped organ in pelvis btw. bladder & rectum • Receives & nourishes fertilized egg • 3 muscular layers Endometrium – inner (decidua basalis during pregnancy) Perimetrium - outer Myometrium - middle Uterus • Fundus - Upper rounded part • Corpus - Middle - body • Cervix - Lower part • Internal Orifice (OS) opens into uterus • Canal • External OS opens into vagina Vagina • Muscular tube that extends from cervix to the vaginal opening in the perineum • Known as the birth canal • Passageway for menstrual blood flow, penis intercourse, & the fetus • • Ovaries Form the expel ova Primary source of estrogen & progesterone Fallopian Tubes • Attached to each side of uterus • Passageways for ovum to travel to uterus • Fertilization occurs in middle or outer part of tubes & then fertilized egg travels to uterus to implant itself • ~ 5 – 7 days for ovum to travel Fertilization & Implantation Fertilization • Occurs in the ampulla of the fallopian (uterine) tube when sperm & ova unite • When fertilized, the membrane of the ovum undergoes changes that prevent entry of other sperm • 23 chromosomes per reproductive cell • Sperm carry X or Y chromosome, XY, male; XX, female Implantation • The zygote implants in the uterus 6 to 8 days after ovulation. • The blastocyst secretes chorionic gonadotropic, so the luteum remains viable & secretes estrogen & progesterone for the first 2 - 3 months of gestation. https://www.youtube.com/watch?v=UDpTaUtgf0g Pelvis • Ilium forms hip bones • 2 pubic bones fuse at symphysis pubis • Sit-down bones or ischial tuberosities • ischial spines: bony projections on ischium • Pelvic joints lined w/cartilage which soften (d/t relaxin) during pregnancy & allows greater mobility of pelvic bones Prenatal Development Embryo at 3 weeks, 4 weeks, 8 weeks Growth of Embryo - Fetus • 1 month – heart begins to beat • 2 months – calcification of bones • 3 months – facial features are distinct • 1-3 months - internal organ development • 4 - 9 months refinement of development http://www.youtube.com/watch?v=gfgq7WiHbh4 Placenta Organ that sustains & nourishes the growing pregnancy 3 main functions • Provide for the transfer & exchange of substances • To act as a barrier to certain substances • To function as an endocrine gland by producing hormones Placental Hormones • When pregnancy occurs the fertilized egg implants in uterine lining & secretes hCG human chorionic gonadotropin • hPL: promotes lactation • Estrogen & progesterone: prepare uterus for pregnancy, & breast for lactation Trophoblast develops into the placenta Placenta has 2 membranes: chorion & amnion https://www.youtube.com/watch?v=MzkIE8zn3b4 Amniotic fluid Fills the amniotic cavity Serves 4 main functions • Physical protection • Temperature regulation • Provision of unrestricted movement • Symmetrical growth Yolk sac: small structure attached to embryo – produces blood cells for ~ 6 weeks Umbilical cord • Fetus is attached to placenta by umbilical cord • Umbilical cord: contains 2 arteries & 1 vein (“AVA”) • Surrounded by gel-like substance: Wharton’s jelly • Protects blood vessels & prevents kinking of cord Fetal Circulation • Fetal HR: 160 to 170 beats/min during first trimester, slowing to 110 to 160 beats/min near or at term Fetal circulation bypass • Ductus arteriosus connects pulmonary artery to aorta, bypassing lungs • Ductus venosus connects umbilical vein & inferior vena cava, bypassing liver • Foramen ovale is opening between right & left atria of heart, bypassing lungs http://www.youtube.com/watch?v=-IRkisEtzsk Δ’s in Circulation After Birth http://www.youtube.com/watch?v=jFn0dyU5wUw • Foramen ovale closes within 2 hrs after birth (permanently by age 3 mons) • Ductus arteriosus closes within 15 hrs (permanently ~3 wks) • Ductus venosus closes functionally when cord is cut (permanently in about 1 wk) • After permanent closure, the ductus arteriosus & ductus venosus become ligaments • Multifetal pregnancy – Monozygotic twins • Identical twins derived from 1 zygote • Share same genetic material; always the same sex – Dizygotic twins • Fraternal twins develop from separate egg & sperm fertilizations • Genetic material is not identical; may or may not be the same sex Female Pelvis & Measurements True pelvis Lies below pelvic brim;consists of pelvic inlet, midpelvis, & pelvic outlet False pelvis Shallow portion above pelvic brim; supports abd viscera Female Pelvis & Measurements (cont’d) Types of pelvis Gynecoid: normal female pelvis; transversely rounded or blunt; Android: heart-shaped or angulated; resembles a male pelvis; narrow pelvic planes Female Pelvis & Measurements Types of pelvis (cont’d) Anthropoid: oval shaped, the outlet is adequate, with a normal or moderately narrow pubic arch Platypelloid: flat shape with an oval inlet; the transverse diameter is wide, the anteroposterior diameter is short Important pelvic inlet diameters Diagonal conjugate Obstetric conjugate Transverse diameter Physiological Maternal Δ’s Reproductive system -Δ’s in the Uterus • Uterus enlarges with ↑ in # & size of blood vessels • wt & capacity • from almost solid structure to thin, muscular sac • from pear-shaped to globular • location from pelvis to abd cavity • 20% of cardiac output supplies uterus/pelvic cavity alone Physiological Maternal Δ’s cont’d Reproductive system -Δ’s Cervix & ovaries • Cervix becomes shorter, more elastic, & larger in diameter • Ovulation stops (Maturation of new follicles is blocked) • Vascularity ↑’s, & glandular tissue multiplies during pregnancy • Thick mucous plug develops in the opening of the cervix • Corpus luteum continues to function & produces progesterone for ~ 6-7 wks Physiological Maternal Δ’s cont’d Reproductive system • Vaginal secretions are ↑’ed • Vagina & perineum are affected by hormonal Δ’s & ↑’ed blood supply to the area • Vagina takes on a bluish-purplish hue, Chadwick’s sign Physiological Maternal Δ’s cont’d • Reproductive System – Breasts • Breast size ↑’s • Colostrum may appear • Tenderness in 1st few wks of pregnancy • Nodularity of breast tissue • Prominent areola with deepened pigmentation • Prominent projections of Montgomery’s tubules Physiological Maternal Δ’s cont’d Respiratory system • Oxygen consumption ↑’s by 15% to 20% • Diaphragm is elevated because of enlarged uterus; SOB may be experienced • Possible slight ↑ in respir. rate Physiological Maternal Δ’s Cardiovascular System • Circulating blood volume ↑‘s by 40% to 50% • Physiological anemia may occur; ↑ in body's iron demand • Heart size ↑‘s & is elevated upward to left as uterus enlarges • Na+ & water retention may occur • Pulse may ↑ about 10 to 15 beats/min Physiological Maternal Δ’s Renal system • frequency of urination ↑’s in 1st & 3rd trimesters • Decreased bladder tone & ↑’ed bladder capacity response to increased levels of progesterone & estrogen • Excretes waste products of mom & fetus • Progesterone causes renal pelvis & ureters to lose tone, leads to urinary stasis • Susceptible to UTIs • Fluid retention Metabolism • Metabolic function ↑’s • Body wt ↑’s Physiological Maternal Δ’s cont’d Integumentary system (skin) • Pigmentation is increased • Linea nigra is apparent • Chloasma may appear • Striae may appear • Vascular spider nevi may appear Chloasma Linea nigra Physiological Maternal Δ’s (cont’d) Gastrointestinal system •Intestines are displaced to sides & upward • N/V may occur from 1st through 3rd months • Constipation may occur • Lack of appetite because of ↓’ed gastric motility & alteration in taste & smell • Flatulence & heartburn because of slow stomach emptying caused by ↑’ed progesterone • Hemorrhoids caused by ↑’ed venous pressure • Swollen, bleeding gum tissue & excessive secretion of saliva caused by ↑’ed levels of estrogen Physiological Maternal Δ’s cont’d Musculoskeletal system • Center of gravity changes in 2nd trimester; lumbosacral curve ↑’s • Aching, numbness, waddling results; walking may be difficult • Lordosis ↑’s • Diastasis recti abdominis • Relaxation & ↑’ed mobility of pelvic joints • Abdominal wall stretches • Umbilicus flattens or protrudes • Encourage pt to maintain good posture as pregnancy progresses Physiological Maternal Δ’s cont’d Endocrine system basal metabolic rate rises – Pituitary enlarges – Prolactin levels ↑ progressively – ↑’ed protein binding – Thyroid gland ↑’s in size – Need for insulin ↑’s Nervous system – numbness, tingling in hands, arms, fingers r/t pressure on nerves, – carpel tunnel syndrome Physiological Maternal Δ’s cont’d • Hematologic Δ’s • Blood volume ↑’s by 40%–50% • RBC volume ↑’s up to 30% • Plasma volume ↑’s by 50% • Hemoglobin Δ’s to 11–12 g/100mL • Hematocrit ↓’s • WBC count ↑’s up to 16,000 mm3 (Normal Hgb 11.7 - 15.5, & Hct 38 - 44) Discomforts of Pregnancy Nausea & vomiting Begins 1st trimester & subsides by 3rd month Caused by elevated hCG levels & Δ’s in carbohydrate metabolism Interventions Eat dry crackers before rising; eat small, frequent, low-fat meals. Drink liquids between rather than at meals. Avoid brushing teeth after rising; avoid fried & spicy foods. Ask health care provider (HCP) about acupressure & use of herbal remedies. Discomforts of Pregnancy (cont’d) • Syncope • Occurs during 1st trimester • Supine hypotension occurs during 2nd & 3rd trimesters • May be caused by hormones, anemia, fatigue, lying flat • Interventions: elevate feet, Δ positions slowly • Urinary urgency & frequency • Occurs during 1st & 3rd trimesters because of pressure of uterus on bladder • Interventions • Drink at least 2000 mL of fluid daily. • Limit fluids during evening; void regularly. • Sleep on side; wear perineal pads; perform Kegel exercises Discomforts of Pregnancy (cont’d) • Breast tenderness • Occurs from 1st through 3rd trimesters • Caused by ↑’ed levels of estrogen & progesterone • Interventions: encourage supportive bra wear; avoid soap on nipples & areolae • ↑’ed vaginal discharge • Occurs from 1st through 3rd trimesters • Caused by hypertrophy & thickening of vaginal mucosa • Interventions: proper cleansing & hygiene; wear cotton underwear; avoid douching Discomforts of Pregnancy (cont’d) • Nasal stuffiness or nosebleeds • Occurs during 1st through 3rd trimesters • Result of increased estrogen that causes swelling of nasal tissues & dryness • Interventions: humidifier; avoid nasal sprays or antihistamines • Fatigue • Occurs during 1st through 3rd trimesters • Result of hormonal Δ’s • Interventions • Frequent rest periods during day; avoid eating or drinking foods with stimulants. • Use correct body mechanics • Regular exercise as approved by HCP; muscle relaxation & strengthening exercises for legs & hip joints Discomforts of Pregnancy (cont’d) • Heartburn • Occurs during 2nd through 3rd trimesters • Results from ↑’ed progesterone levels, ↓’ed GI motility, displacement of stomach by enlarging uterus • Interventions • Eat small, frequent meals & avoid fatty & spicy foods. • Sit upright for 30 mins after meals. • Drink milk between meals. • Consult HCP about antacids. Discomforts of Pregnancy (cont’d) • Ankle edema • Occurs during 2nd & 3rd trimesters • Result of vasodilation, venous stasis, & ↑’ed venous pressure below uterus • Interventions • Elevate legs twice daily & when resting; wear supportive stockings. • Sleep on side. • Avoid sitting or standing in one position for long periods. Discomforts of Pregnancy (cont’d) • Varicose veins • Occurs during 2nd & 3rd trimesters • Caused by weakening walls of veins or valves & by venous congestion • Interventions • Wear supportive stockings. • Elevate feet when sitting; elevate feet & hips when lying down. • Avoid long periods of standing or sitting. • Move about while standing. • Avoid leg crossing & constricting clothing. • Exercise legs, avoid airline travel to prevent thrombophlebitis. Discomforts of Pregnancy (cont’d) • Headaches • Occur during 2nd & 3rd trimesters • Result of Δ’s in blood volume & vascular tone • Interventions • Δ positions slowly. • Apply cool cloth to forehead. • Eat small snacks. • Use acetaminophen if prescribed. Discomforts of Pregnancy (cont’d) • Hemorrhoids • Occur during 2nd & 3rd trimesters • Result of ↑’ed venous pressure & constipation • Interventions • Soak in warm sitz bath; sit on soft pillow. • Eat high-fiber foods & drink sufficient fluids. • ↑ mild exercise; apply tx’s as prescribed Discomforts of Pregnancy (cont’d) • Constipation • Occur during 2nd & 3rd trimesters • Results from ↑ in progesterone, ↓’ed intestinal motility, displacement of intestines, pressure of uterus, iron supplements • Interventions • Eat high-fiber foods. • Drink at least 2000 mL daily. • Exercise regularly. • Consult with HCP about stool softeners, laxatives, & enemas Discomforts of Pregnancy (cont’d) • Backache • Occur during 2nd & 3rd trimesters • Result of exaggerated lumbosacral curve • Risk for falls; use deliberate, slow movements • Interventions • Rest; sleep on a firm mattress. • Use correct body posture & mechanics. • Wear comfortable, supportive shoes. • Perform pelvic tilt exercises. Discomforts of Pregnancy (cont’d) • Leg cramps • Occur during 2nd & 3rd trimesters • Result of altered calcium–phosphorus balance, pressure of uterus, fatigue • Interventions • Engage in regular mild exercise. • Dorsiflex foot of affected leg. • ↑ calcium intake. • Shortness of breath • Occur during 2nd & 3rd trimesters • Result of pressure on diaphragm form enlarged uterus • Interventions: take small rest periods; avoid overexertion; sleep on side or with head elevated Psychological Maternal Δ’s Ambivalence May occur in early pregnancy Mother may experience a dependence– independence conflict related to role Δ’s Partner may experience ambivalence r/t new role, financial responsibilities, & sharing attention Acceptance Factors include readiness for experience & identification with motherhood role Emotional liability Manifested by frequent or extreme Δ’s in emotional state, which are common Psychological Maternal Δ’s cont’d Body image Δ’s Positive or negative Δ’s in woman's perception of her image occur gradually during pregnancy. Physical Δ’s & symptoms contribute to body image. Relationship with fetus Woman may daydream & think about desired maternal qualities Accepts biological fact of pregnancy Accepts fetus is a distinct person to nurture Prepares realistically for birth and parenting Psychological Paternal Δ’s The father • ambivalent feelings • Fears • question his ability • feel rejected Pregnancy Signs 3 Categories: • Presumptive signs (subjective) • Probable signs (objective) • Positive signs Pregnancy Signs Presumptive signs (subjective) • Amenorrhea • N/V • ↑’ed size & fullness in breasts; pronounced nipples • Urinary frequency • Fatigue • Quickening: first perception of fetal movement around the 16th to 20th week of gestation • Discoloration of vaginal mucosa Pregnancy Signs (cont’d) Probable signs (objective) • Hegar’s sign: softening & thinning of lower uterine segment at about 6 wk of gestation • Goodell’s sign: softening of cervix, beginning at 2nd month of gestation • Chadwick’s sign: violet coloration of mucous membranes of cervix, vagina, vulva at ~ 6th wk of gestation • Ballottement: rebounding of fetus against examiner’s fingers on palpation 16-20 wks floating fetus Probable signs (cont’d) • Uterus enlargement • Positive pregnancy test d/t presence of hCG which appears in the urine 8-10 days after conception • Braxton-Hicks contractions – irregular contractions occur intermittently throughout pregnancy but don’t ↑ in intensity or duration or cause cervical dilation • Darkening of nipples & areola • Linea nigra- dark line from symphysis to xiphoid process, chloasma of the face, striae gravidarum- stretch marks Pregnancy Signs (cont’d) Positive signs confirm pregnancy: SIGNS OF THE SENSES– 6 wks+ • Visualization of fetus by U/S – 20 wks+ • Fetal heart sounds by fetal stethoscope – 22 wks+ • Fetal movements palpable by a trained practitioner – Late pregnancy • Fetal movements visible Recommended Schedule of Prenatal Visits—Uncomplicated Pregnancy • Conception to 28 weeks—every 4 weeks • 29 to 36 weeks—every 2 to 3 weeks • 37 weeks to birth—weekly • Certain laboratory &/or diagnostic tests are performed at various times throughout the pregnancy • https://www.youtube.com/watch?v=jThcEjwLri0 Prenatal Visit • Obtain the baseline data • Confirm or r/o a dx of pregnancy • Ascertain risk factors • Determine the estimated date of delivery (EDD) • Provide education on maintaining a healthy pregnancy • Hx taking ‒Chief complaint ‒Reproductive hx ‒Medical-surgical hx ‒Family & Social hx Prenatal Visit (cont.) •Physical examination •Head-to-toe physical •Vaginal speculum examination •Bimanual examination of the uterus Diagnostic Tests •Laboratory work CBC (Hemoglobin & hematocrit levels) •Tests for presence of infection •Group B streptococcus (GBS) after 35 wks & before the end of 37 wks. Pregnancy Tests • Based on the presence of the hormone hCG which is secreted by the chorionic villi of the placenta • Appears in the urine or blood 9-10 days after conception (or 24-48 hrs) after implantation • HPT (home pregnancy tests 97% accurate Diagnostic Tests cont’d Blood type & Rh factor https://www.youtube.com/watch?v=7OWp8d8WKkg • Mother is Rh-negative & has negative antibody screen • Will need to repeat antibody screens • Should be given Rho(D) immunoglobulin (RhoGAM) within 72 hrs of birth of first baby when detected • With every pregnancy, should be given RhoGAM at 28th wk of gestation & within 72 hrs of birth of baby Diagnostic Tests (cont’d) • Rubella titer • Pt with negative titer (<1:8) is at risk of contracting rubella, which can be transmitted to fetus & cause birth anomalies; thus, titer should be assessed before conception • If negative titer, pt must be using effective birth control at time of immunization, must be counseled to not become pregnant for 3 mons following immunization Diagnostic Tests(cont’d) • Papanicolaou’s smear • Sexually transmitted infection • Sickle cell screening • Tuberculin skin test • Positive test indicates need for chest x-ray to rule out active disease • In pregnant pt, x-ray can’t be performed until after 20th week of gestation • Hepatitis B surface antigens • Recommended for all women because of prevalence of disease in general population Diagnostic Tests cont’d • Urinalysis & urine culture • Levels of 2+ to 4+ protein in urine may indicate infection or preeclampsia - Ultrasonography • Outlines, identifies fetal & maternal structures Diagnostic Tests cont’d -Assists in confirming gestational age & estimated date of confinement • Alpha-fetoprotein screening • Can detect neural tube defects,(spina bifida & Down syndrome) • Maternal blood sample drawn at 15th to 18th week of gestation • Chorionic villus sampling • https://www.youtube.com/watch?v=Axt2Ae9mNec • Detects genetic abnormalities by sampling chorionic villus tissue at 8th to 12th wk of gestation • Kick counts (fetal movement counting) Diagnostic Tests (cont’d) • Amniocentesis https://www.youtube.com/watch?v=bZcGpjyOXt0 • Aspiration of amniotic fluid may be done from 13th to 14th wk of gestation • Used to determine genetic disorders, metabolic defects, fetal lung maturity • Risks of maternal hemorrhage, infection, abruptio placentae, premature rupture of membranes • Fern test • Microscopic slide test to determine presence of amniotic fluid leakage Diagnostic Tests (cont’d) - Nitrazine test • Determines presence of amniotic fluid in vaginal secretions; shades of blue indicate that membranes probably ruptured • Nonstress test • Performed to assess placental function & oxygenation • Assesses fetal well-being • Contraction stress test • Performed to assess placental oxygenation & function • Assesses fetal ability to tolerate labor, fetal well-being Gravidity & Parity • Gravidity: # of pregnancies • Gravida: woman who is pregnant • Nulligravida: woman who has never been pregnant • Primigravida: woman pregnant for the first time • Multigravida: woman having had 2 or more pregnancies • Parity: number of births carried past 20 weeks’ gestation, whether or not the fetus was born alive • Nullipara: woman who has not had a birth at more than 20 weeks’ gestation • Primipara: woman who has had one birth that occurred after 20 weeks’ gestation Gravidity & Parity (cont’d) Parity (cont’d) • Multipara: woman who has had 2 or more pregnancies that resulted in viable offspring Use of GTPAL: pregnancy outcomes can be described with the GTPAL acronym • G = gravidity, including present pregnancy • T = term births, after 37 weeks • P = preterm births, before 37 weeks • A = abortions or miscarriages • L = live births Prenatal Visit • • • • • • • • • Teaching Avoiding substance abuse Diet, nutrition, & exercise Infection control & medications Dental hygiene Hygiene & clothing Breast care Sexual activities Employment & travel Methods of Determining the Due Date • Nagele’s rule • Add 7 days to the date of the first day of the LMP, then subtract 3 months & add 1 yr. • Pelvic examination • The practitioner feels the size of the uterus to determine the term of the pregnancy • Obstetric sonogram • High frequency sound waves reflect off fetal & maternal pelvic structures, allowing visualization Trimesters • Pregnancy divided into 3- 13-week parts • Important to know what occurs during each trimester to both woman & fetus • Helps provide anticipatory guidance • Identify deviations from the expected pattern of development Physical examination • Baseline TPR, BP, ht., wt • Head-to-toe physical Vaginal speculum examination Bimanual examination of the uterus McDonald's rule the length in cms of the abdominal contour from the upper margin of the pubic symphysis to the fundus of the uterus, divided by 3.5, gives the duration of pregnancy in lunar months; applicable only after the 6th month of pregnancy. Fundal Height – Measured to evaluate gestational age of fetus – During the 2nd & 3rd trimesters, fundal ht in cms ~ equals the fetus' age in wks plus or minus 2 cm – At 16 wks, fundus can be found approximately halfway between the symphysis pubis & the umbilicus – At 20 to 22 wks, fundus is ~ at the location of the umbilicus – At 36 wks, fundus is at the xiphoid process Nutritional Requirements of Pregnancy • ↑ kCal by 300 per day, & should include – Protein—60 g/day – Calcium—1200 mg/day – Iron—30 mg/day – Folic acid—400 mcg (0.4mg)/day • Recommended wt gain –First trimester: 3–4 lbs total –Remainder of pregnancy: 1 lb/wk –Total wt gain: 25–35 lbs for a woman with a normal BMI • Breast feeding– ↑ 500 kCal or total 2700 kCal Weight Gain • Women of normal weight: 25 to 35 lbs (11.5 to 16 kg) • Obese women: 11 to 20 lbs (5 to 9 kg) • Overweight women: 31 to 50 lbs (14 to 22.7 kg) • Multifetal pregnancy: twins—woman should gain 4 to 6 lbs in first trimester, 1½ lbs per week in second & third trimesters, for a total of 37 to 54 lbs Weight Gain Assessment • • • • • Edema of lower extremities, face, hands Discomforts of pregnancy Eating & sleeping patterns Psychosocial concerns Fundal ht for uterine & fetal growth Milestones of fetal growth: fundus over symphysis at 12-16 wks, at umbilicus at 18-22 wks, at xiphoid at 36wks S&S of Inadequate Nutrition • • • • • Hair Eyes Mouth Neck Skin • • • • • Extremities Finger/toe nails Mom’s wt. BP Fetal growth Nutritional Risk Factors During Pregnancy Adolescent Excessive wt. gain Anemia Anorexia Smoking Frequent pregnancies • PICA • Vegetarianism • Cultural considerations • • • • • • • • • • • • • • • Low income Food/diet fads Drug/alcohol use Overweight/underwt Multiple pregnancy Anemic at conception Lactose intolerance Sudden wt gain Chronic illness Drugs Used in Prenatal Period Class: serum immune globulin Drug: RhoGAM, Rho (D) Immune Globulin Action: prevents production of anti-Rh antibodies in Rh- people & therefore prevents hemolytic disease in RH+ newborn Route IM: Administered at 28 wks of gestation & within 72 hrs of delivery, also administered after amniocentesis, miscarriage, abortion, ectopic pregnancy Contra: Rh+ patients Side effects: painful injection site, fever Nursing: educate pt. in purpose of drug Drugs Used in Prenatal Period cont’d PNV Vitamins – A,D,E,C, folic acid, thiamine, riboflavin, niacinanmide, B6, B12 Minerals – Ca, copper, iron, zinc Indications – vitamin & mineral supplement throughout pregnancy & lactation Dosage – 1 daily Side effects – rare, epigastric distress sometimes occurs when admin. On an empty stomach, admin. With meals, citrus juice enhances absorption The Process: The Four P’s of Labor Process of labor; coordinated sequence of involuntary uterine contractions to move fetus through birth canal, to delivery, actual birth of newborn • 4 major factors interact during normal childbirth; four Ps of labor depend on each other for safe delivery • Power: uterine contractions • Passageway: mother’s rigid bony pelvis, soft tissues of cervix, pelvic floor, vagina, introitus • Passenger: fetus, membranes, placenta • Psyche: woman’s emotional system The Process: The Four P’s of Labor (cont’d) • Attitude • Relationship of fetal body parts to one another • Lie • Relationship of spine of fetus to spine of mother • Presentation • Portion of fetus that enters pelvic inlet first The Process: The Four P’s of Labor (cont’d) • Presenting part: specific fetal structure lying nearest cervix • Position: relationship of assigned area of presenting part to maternal pelvis • Station • Measurement of progress of descent in centimeters above or below midplane, from presenting part to ischial spine Variables Affecting Labor 4 P’s- Passageway, Passenger, Powers, Psyche Passageway: bony pelvis, uterus, cervix, vagina, perineum • Pelvis: MD checks pelvis size by measuring diagonal conjugate, palpating the ischial tuberosities, or U/S • Uterus: contractions begin in the fundus & travel down thru cervix • Cervix: uterine contractions pull cervix open • Vagina: stretches • Perineum: stretches & thins Passenger • Fetal skull • Fetal accommodation to the passageway – Lie •Longitudinal lie •Oblique lie •Transverse lie Passenger (cont.) – Presentation • Foremost part of the fetus that enters the pelvic inlet ‒Head • Cephalic presentation ‒Feet or buttocks • Breech presentation ‒Shoulder • Shoulder presentation Passenger (cont.) – Attitude • Relationship of fetal parts to one another • Vertex (attitude of flexion) is most favorable for vaginal delivery • Military (no flexion or extension) • Brow (partial extension) • Face (full extension) Types of presentation A. Vertex B. Military C. Brow D. Face Passenger (cont.) – Fetal Station: The relationship of the presenting part to the ischial spines • Zero station: Presenting part is at the level of the ischial spines • Minus station: Presenting part is above the ischial spines • Plus station: Presenting part is below the ischial spines Fetal Position • Leopold’s Maneuvers • http://www.youtube.com/watch?v=nIog3oizP8A • LOA • Station • Engaged Leopold’s Maneuvers To determine presentation & position of fetus • If head is in fundus, hard, round movable object is felt; if buttocks is in fundus, then soft, irregular shape is noted, more difficult to move • Back of fetus should be felt on one side of abd • Irregular knobs & lumps, hands, feet, elbows, & knees felt on opposite side of abdomen Powers • Phases of involuntary uterine contraction – Increment: Building up of the contraction - longest phase – Acme: Peak of the contraction – Decrement: Letting up phase – Relaxation period: Rest period between contractions Descriptors of contractions • Frequency: How often the contractions are occurring • Measured by counting the time interval from the beginning of one contraction to the beginning of the following contraction • Duration • The interval from the beginning of a contraction to its end • Intensity • The strength of the contraction Uterine Contractions • Effect of contractions on the cervix • Efface • Dilate • Phase of contractions • Increment • Peak • Decrement • Frequency • Duration • Intensity • Mild • Moderate • Firm • Maternal pushing Cervical Effacement & Dilation True labor • Contractions ↑ in duration &intensity • Cervical dilation, effacement are progressive False labor • Normal contractions are exaggerated • Labor does not produce dilation, effacement, or descent • Contractions are irregular, without progression • Walking has no effect on contractions; often relieves false labor Psyche • Factors impacting the psyche of a laboring woman – Current pregnancy experience – Previous birth experiences – Expectations for current birth experience – Preparation for birth Breathing Techniques Provide focus during contractions • Promote relaxation & oxygenation between contractions • Slow deep breathes – in through the nose, out through the mouth Childbirth Education • Δ’s of pregnancy • Fetal development • Prenatal care • Hazardous substances to avoid • Nutrition • Common discomforts • Work, benefits of exercise • Coping with labor & delivery Types of Classes Available • Gestational DM • Early pregnancy • Exercise for pregnant women • Infant care • Breastfeeding • Sibling • Grandparent • Adolescent childbirth Variations of Basic Childbirth Preparation Classes • Refresher • Cesarean birth • Vaginal birth after cesarean • Adolescent Methods of Childbirth Preparation • Dick-Read method • Bradley method • Lamaze method • https://www.youtube.com/watch?v=0xRl2s2zE78 Signs of Impending Labor (Prelabor) • • • • • • Braxton Hicks contractions Increased vaginal discharge Bloody show ~ 1 wk before labor Rupture of the membranes Energy spurt Weight loss Process of Labor Anticipatory signs of labor • Prelabor • Effacement Measured in % from 0 – 100% . 0 = no effacement, 100%= complete Induction of Labor • Elective induction • Major cause of ↑ in # of induced labors • Often result in • More interventions • Longer labors • Higher costs • Possible cesarean birth Induction of Labor (cont.) • Indications for induced labor • Postdate pregnancy • Premature rupture of membranes (PROM) • Spontaneous rupture of membranes (SROM) without the onset of spontaneous labor • Chorioamnionitis • Pregnancy-induced HTN • Preeclampsia • Severe intrauterine fetal growth restriction • Maternal medical conditions Induction of Labor (cont.) • Contraindications • Maternal contraindications for spontaneous & induced labor • Complete placenta previa • Hx of a classical uterine incision • Structural abnormalities of the pelvis • Invasive cervical CA • Medical conditions (active genital herpes) • Fetal contraindications • Certain anomalies, (hydrocephalus) • Certain fetal malpresentations • Fetal compromise Induction of Labor (cont.) • Labor readiness • Prerequisite for induced labor = “ripe cervix” • Bishop Score often used to determine readiness for labor • 5 factors evaluated • Each factor scored 0 to 3 • Score of 8 or greater associated with successful oxytocin-induced labor • Score of 5 or less indicates cervix is not ripe – associated with unsuccessful induction of labor Induction of Labor (cont.) • Labor readiness (cont.) • Transvaginal ultrasound • Relatively new method • Cervix 27 cm or less is a predictor of successful induction of labor despite Bishop score • Measurement of fetal fibronectin levels • Newer method • Presence in cervical secretions is associated with labor readiness • More often used as a predictor of preterm labor risk Induction of Labor (cont.) • Labor readiness (cont.) • Fetus should be mature • Several ways to assess fetal maturity • At least 38 weeks’ gestation considered mature • Date fetal heart tones first heard • Other pregnancy milestones • Fetal lung maturity is the major point of consideration • Measure L/S ratio by amniocentesis Induction of Labor (cont.) • Methods of cervical ripening • Mechanical methods • Membrane stripping • Inserting a catheter into the cervix & inflating the balloon • Cervical dilators (laminaria) Induction of Labor (cont.) • Pharmacologic methods • Prostaglandin E2 (dinoprostone) • Prostaglandin E1 (misoprostol) • Artificial rupture of membranes (AROM) • Also called amniotomy • Oxytocin induction • IV oxytocin (Pitocin) most common Induction of Labor (cont.) • Nursing care • The LPN role during induction depends upon the procedure • Assist with pelvic exam in mechanical ripening of cervix or amniotomy (AROM) • Document FHR before & after amniotomy • Suprapubic or fundal pressure during the procedure if trained • RN responsible for monitoring mother & baby during pharmacologic ripening of cervix When to go to the hospital • Instruct Mom when to call MD & when to go to the hospital • Wait for contractions to be 5-10 mins apart • Clear liquids once labor begins • Prenatal records, medical hx & prenatal course sent to hospital before mother’s admission & include any special requests mother or father have regarding procedures, meds, etc. Admission to L&D suite • Baseline VS’s, breath sounds, wt., urine spec. for blood, protein & glucose, nitrazine test prn. • Leopold’s maneuvers • Onset of labor, S&S of prelabor, Rh factor, blood type, gravada/para status, ? breast/bottle feeding • Check Contractions • Monitored Baseline FHR • Vaginal exams • Couple’s expectations & concerns Stages & Duration of Labor http://www.youtube.com/watch?v=b-CtjWf7K8w • First stage: dilation & effacement (can last 4 to 6 hrs) • Early labor (latent phase) • Active labor (active phase) • Transition (transition phase) • Second stage: birth (30 mins to 2 hrs) • Third stage: delivery of placenta (5 to 30 mins) • Fourth stage: recovery Stage 1 Effacement & dilation Begin with true labor contractions & end with complete dilation of cervix (0-10cm) Effacement: thinning & shortening of cervical canal Dilation: enlargement of cervical opening from 0-10cm. 10cm = complete dilation. Divided into the latent, active & transition phases Nursing Process During the First Stage of Labor: Dilation • Focus is on assessment • Providing physical care to the mother & fetus • Providing psychological care to the mother • Keeping the practitioner informed about labor progress Latent phase • Cervix dilates from 0-4 cm • Irregular, short, mild contractions occur • Contractions every 10 – 20 minutes lasting 15- 45 seconds • Intensity of contractions gradually increases • Mom up & about, talkative, anxious Nursing Interventions During the Latent Phase (Early Labor) • Assessment • Assess FHR & contractions at least once every hour • Assess maternal status • Assess status of fetal membranes • Assess the woman’s psychosocial state Active phase • Cervix dilates from 4- 8 cm • Contractions occur every 3- 5 minutes, last 40 -60 seconds & are moderately intense • Mom begins to use breathing techniques to help reduce discomfort Nursing Interventions During Active Labor • Assessment • Assess woman’s psychosocial state • Assess labor progress • Assess fetal status • Assess maternal status Transition Phase • Period of cervical dilation from 8–10 cm • Most difficult time for Mom • Intense contractions occur every 2- 3 mins. & last 60 -90 sec. • Mom may experience loss of control of breathing techniques & experience N/V • Other S&S: restlessness, anger, difficulty following directions, rectal pressure, “don’t touch me stage” Nursing Interventions Stage 1 Offer fluids & ice chips; IV fluids Record I&O’s Provide oral care Enc. Urination Q 2 hrs Back Rubs Freq. position Δ’s Enc. Ambulation (membranes intact); Pericare ruptured; Δ linens prn • Offer pain meds prn • Offer encouragement & praise • Inform Mom & support person of progress • • • • • • • Fetal Monitoring Means of assessing fetal heart rate (FHR) as it relates to uterine contractions • Normal FHR 110 to 160 beats/min • External fetal monitoring • Noninvasive; performed using tocotransducer or Doppler ultrasonic transducer; transducer, fastened with belt, should be placed on side of mother where fetal back is located (find using Leopold’s maneuvers) • Internal fetal monitoring • Invasive; requires rupturing of membranes; attachment of electrode to presenting part of fetus; mother must be dilated 2 to 3 cm to perform this procedure Fetal Monitoring (cont’d) Periodic patterns in FHR • Baseline FHR • 110-160 BPM • Fetal bradycardia • <110 BPM • Fetal tachycardia • >160 BPM • Baseline variability • Moderate variability • Marked variability • Absent variability • Accelerations • Early decelerations • Variable decelerations • Late decelerations • Prolonged decelerations • Recurrent decelerations • Intermittent decelerations • Sinusoidal pattern Nursing Care during Labor & Delivery • Monitoring uterine contractions – External Methods • Palpation to evaluate the contraction pattern • Tocodynamometer (toco) Nursing Interventions: Uterine Contractions • Reassuring periodic Δ’s – Accelerations - above the baseline by at least 15 bpm for at least 15 secs (15 x 15 window) • Benign periodic Δ’s – Early decelerations • Non-reassuring periodic Δ’s – Variable decelerations indicating some type of acute umbilical cord compression – Late decelerations indicating uteroplacental insufficiency Stage 2 • • • • • • • The expulsion stage Complete dilation of cervix & ends with birth of baby Ferguson’s Reflex Mom pushes baby through birth canal using abd. muscles Fetus has left uterus & is in vaginal canal Vaginal tissues bulges, rectum dilates, pelvic floor muscles stretch & head of fetus appears at vaginal opening Crowning With additional pushing baby is born Nursing Interventions During the 2nd Stage of Labor: Expulsion of the Fetus • Assessment • Monitor VSs every 15 - 30 mins • Assess contraction pattern every 15mins • Assess the woman’s report of an uncontrollable urge to push • Check FHR every 15 mins for the lowrisk women & every 5 mins for women at risk for labor complications Mechanism of Labor: different positions the fetus must assume as it travels the birth canal • Descent • Station • Engagement • Flexion • Internal rotation • Extension • External rotation • Expulsion Episiotomy: surgical incision in perineum to widen opening; helps prevent vaginal tears, can be left, right, or midline Stage 3 Placental Stage • Begins with birth of baby & ends with expulsion of placenta • Uterus continues to contract, becomes smaller causing placenta to separate from uterine wall • Voluntary pushing by mother help to expel placenta Nursing Process During the 3rd Stage of Labor: Delivery of the Placenta • Assessment • Assess the woman’s psychosocial state after she gives birth • Monitor for signs of placental separation Stage 4 Recovery Stage • Expulsion of placenta & 2 hrs, postpartum or until mother’s condition has stabilized • Close monitoring of vaginal bleeding needed to detect hemorrhage • Approx. blood loss = 250 – 500 mL • https://www.youtube.com/watch?v=zD8j2JG2y3A Stage 4 • VS’s • Assess Fundus; vaginal bleeding; perineal sutures • Ice packs applied to all perineum • Monitor output • Provide warm blankets, tremors are common • Maintain IV fluids • Enc. Fluids, snacks • Evaluate mobility of LE’s • Admin. Analgesics prn Nursing Responsibilities During Birth • Preparing the delivery instruments & infant equipment • Perineal scrub • Administering medications • Providing initial care to the infant • Assessing Apgar score • Assessing infant for obvious abnormalities • Examining the placenta • Identifying mother & infant • Promoting parent-infant bonding Pharmacological Techniques • The nurse’s role • Begins at admission • Woman’s preference for pain relief • Keep side rails up • Provide education regarding procedures & expected effects • Observe for hypotension Pain Management Principles & Techniques • Non-Pharmacologic Pain Interventions • Continuous labor support • Comfort measures • Relaxation techniques • Intradermal water injections • Acupressure & acupuncture Pharmacological Interventions • Analgesia & sedation • Use of med. to ↓ sensation of pain • Sedatives given to promote sedation & relaxation • Opioids given to promote analgesia during labor • Anesthesia • Use of med. to partially or totally block all sensation to an area of the body • Local, regional, general Pharmacological Interventions • Types of anesthesia • Local anesthesia • Used to numb perineum just before birth to allow for episiotomy & repair • Regional anesthesia • Involves blocking a group of sensory nerves that supply a particular organ or area of the body • General anesthesia • Not used frequently in obstetrics because of the risks involved Pharmacological Interventions (cont.) • Types of regional anesthesia • Pudendal • Epidural anesthesia • Intrathecal anesthesia http://www.youtube.com/watch?v=bxcCh46Qug8 • Spinal block –type saddle block Epidural analgesia • Opioids are used for epidural analgesia. An adverse effect of epidural analgesia is a delayed respiratory depression. Naloxone (Narcan) is an opioid antagonist, which reverses the effects of opioids & is given for respiratory depression. Pharmacological Interventions (cont.) • Complications Associated With Epidural & Spinal Anesthesia • Hypotension • Maternal fever • Shivering • Pruritus • Inadvertent injection into blood stream • Spinal HA • Fetal distress Nursing Interventions epidural/saddle blocks • VS’s, • Position on left side • Monitor FHR • Monitor Contractions • I&O’s • Examine epidural/spinal catheter for placement • Observe for side effects Pharmacological Interventions (cont.) • Life-Threatening Complications Occurring With General Anesthesia • Failed intubation • Aspiration • Malignant hyperthermia Oxytocic Medication: Oxytocin (Pitocin) • Stimulates smooth muscle of uterus; induces contractions of the myocardium; promotes milk letdown • Uses • Induces or augments labor; controls postpartum bleeding; promotes milk letdown & facilitates breast-feeding; induces or completes an abortion • Adverse reactions • May include allergies, dysrhythmias, Δ’s in blood pressure, uterine rupture, hyperstimulation of uterine contractions • Contraindications Shouldn’t be used in a woman who can’t deliver vaginally or in a woman with hypertonic uterine contractions. Oxytocic Medication: Oxytocin (Pitocin) (cont’d) • Interventions • Monitor maternal & fetal status closely, including frequency, duration, force of contractions, FHR every 15 minutes • Administer med with IV infusion device only • Do not leave pt unattended during infusion • If uterine hyperstimulation or nonreassuring FHR occurs, stop med immediately, turn pt to side, infuse IV NS, administer oxygen via face mask as prescribed; then notify healthcare provider Prostaglandins Ripen cervix, stimulate uterine contractions • Adverse reactions • Diarrhea; N/V; fever; chills; flushing; dysrhythmias; bronchoconstriction; peripheral vasoconstriction • Contraindications • Clients with significant cardiovascular disease or history of asthma, pulmonary disease • Interventions • Monitor maternal VSs, fetal status, including labor status as it relates to mother & fetus • Before administration, have woman void, then maintain supine or side-lying position for 30 to 40 minutes after administration Opioid Analgesics • These are used to relieve moderate to severe pain associated with labor • Regular use during pregnancy may produce withdrawal symptoms in neonate • Keep naloxone (Narcan) on hand at all times as antidote • Meperidine hydrochloride (Demerol) • Not administered during advanced labor (within 1 hour of delivery) Opioid Analgesics (cont’d) Morphine sulfate, fentanyl (Sublimaze) • May cause respiratory depression • Butorphanol tartrate (Stadol), nalbuphine (Nubain) • Have some opioid antagonist effects • Interventions • Monitor VSs (especially for respiratory depression), FHR • Have antidote, naloxone (Narcan), available at all times Assisted Delivery • Episiotomy • A surgical incision is made into the perineum to enlarge the vaginal opening • Vacuum-assisted delivery • A suction cup is placed on the fetus’s head; suction is applied & used to guide the delivery of the infant • Forceps • Instruments with curved, blunted blades are placed around the head of the fetus to facilitate delivery Assisted Delivery (cont.) • Complications of operative vaginal delivery • Neonatal cephalhematoma, retinal, subdural, & subgaleal hemorrhage occur more frequently with vacuum extraction than with forceps. • Facial bruising, facial nerve injury, skull fractures, & seizures are more common with forceps. • Maternal complications include • Extension of episiotomy into anal sphincter • Uterine rupture, perineal pain, lacerations, hematomas, urinary retention, anemia, & rehospitalization Assisted Delivery (cont.) • Nursing care during an assisted delivery • Obtain needed equipment & supplies • Monitor maternal & fetal status before, during, & after the procedure • Assist the birth attendant • Provide support for the woman • Document the type of procedure • Document maternal & fetal response to the procedure Indications for Cesarean Birth •Hx of previous cesarean birth •Previous surgery on the uterus •Labor dystocia (failure to progress in labor) Fetal compromise, Abnormal labor •Non-reassuring fetal status •Fetal malpresentation • Placenta previa or abruptio placentae Maternal conditions (GH or DM) •Active maternal herpes virus Cesarean Birth (cont.) • Maternal complications • Laceration of uterine artery, bladder, ureter, or bowel • Hemorrhage requiring blood transfusion • Hysterectomy • Infection, Pneumonia • Postpartum hemorrhage, thrombophlebitis, & other surgical-related complications • Fetal complications • Delivery of an immature fetus • Depressed fetal respiratory drive, • Fetal injury can occur Cesarean Birth (cont.) • Incision types • Abdominal incisions • Vertical approach done in the midline of the lower abdomen • Pfannenstiel’s incision (bikini cut) • Uterine incisions • Classical incision • Low cervical vertical incision • Low cervical transverse incision (preferred method) Cesarean Birth (cont.) • Steps in a cesarean delivery • Called perioperative period • Preoperative phase • Team approach, sometimes referred to as collaborative management • Intraoperative phase • LPN acts as scrub nurse • Postoperative phase • LPN can assume care of woman after she has sufficiently recovered from anesthesia Cesarean Birth (cont.) • Postop Nursing care • VS’s • CDB, Splinting incision • I&O’s, Foley cath • Assessing abd. incision or staples, Lochia for quantity, color, & presence of clots • PCA pumps, IV fluids • Enc. ambulation Vaginal Birth After Cesarean • Prerequisites • ACOG Recommendations: • Adequate pelvis • No previous uterine ruptures • Personnel & facilities available to perform an immediate cesarean delivery • No more than 1 previous, low transverse uterine scar • Signed informed consent listing benefits & risks • Surgeon, anesthesia provider, & operating room personnel in the hospital • Practitioner who can read & interpret EFM tracings & recognize the S&S of uterine rupture Vaginal Birth After Cesarean (cont.) • Contraindications • Previous classic C-section uterine scar • Placenta previa • History of previous uterine rupture • Lack of facilities or equipment to perform an immediate emergency cesarean