PREGNANT PATIENTS FOR NONOBSTETRIC SURGERIES
advertisement
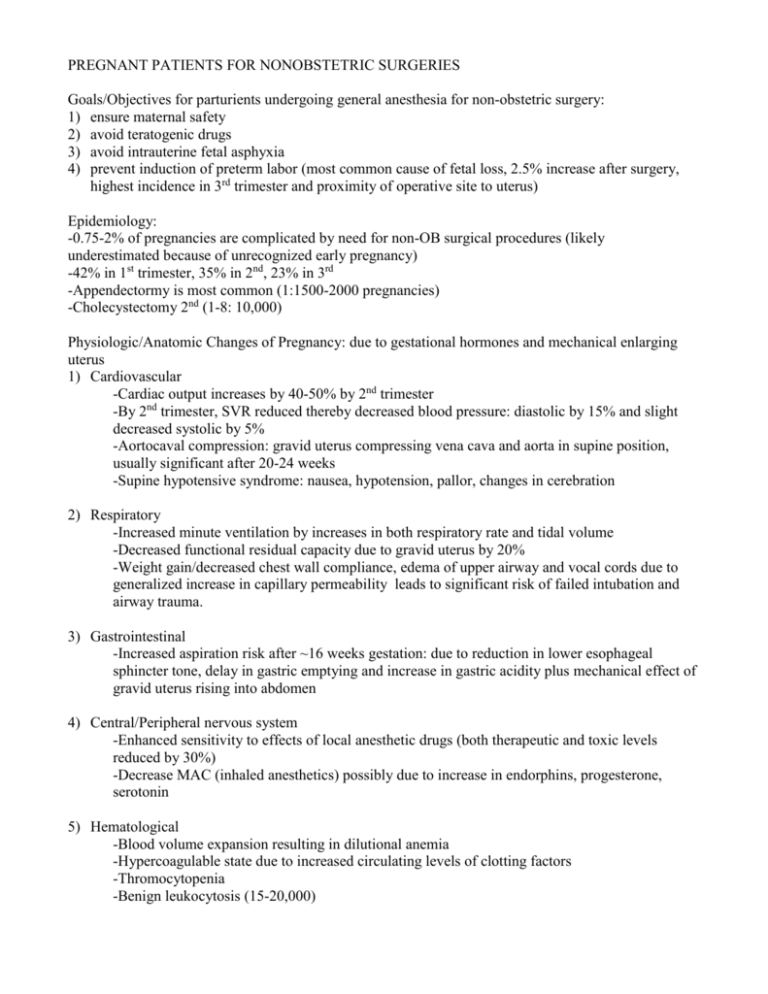
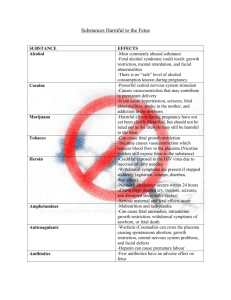
PREGNANT PATIENTS FOR NONOBSTETRIC SURGERIES Goals/Objectives for parturients undergoing general anesthesia for non-obstetric surgery: 1) ensure maternal safety 2) avoid teratogenic drugs 3) avoid intrauterine fetal asphyxia 4) prevent induction of preterm labor (most common cause of fetal loss, 2.5% increase after surgery, highest incidence in 3rd trimester and proximity of operative site to uterus) Epidemiology: -0.75-2% of pregnancies are complicated by need for non-OB surgical procedures (likely underestimated because of unrecognized early pregnancy) -42% in 1st trimester, 35% in 2nd, 23% in 3rd -Appendectormy is most common (1:1500-2000 pregnancies) -Cholecystectomy 2nd (1-8: 10,000) Physiologic/Anatomic Changes of Pregnancy: due to gestational hormones and mechanical enlarging uterus 1) Cardiovascular -Cardiac output increases by 40-50% by 2nd trimester -By 2nd trimester, SVR reduced thereby decreased blood pressure: diastolic by 15% and slight decreased systolic by 5% -Aortocaval compression: gravid uterus compressing vena cava and aorta in supine position, usually significant after 20-24 weeks -Supine hypotensive syndrome: nausea, hypotension, pallor, changes in cerebration 2) Respiratory -Increased minute ventilation by increases in both respiratory rate and tidal volume -Decreased functional residual capacity due to gravid uterus by 20% -Weight gain/decreased chest wall compliance, edema of upper airway and vocal cords due to generalized increase in capillary permeability leads to significant risk of failed intubation and airway trauma. 3) Gastrointestinal -Increased aspiration risk after ~16 weeks gestation: due to reduction in lower esophageal sphincter tone, delay in gastric emptying and increase in gastric acidity plus mechanical effect of gravid uterus rising into abdomen 4) Central/Peripheral nervous system -Enhanced sensitivity to effects of local anesthetic drugs (both therapeutic and toxic levels reduced by 30%) -Decrease MAC (inhaled anesthetics) possibly due to increase in endorphins, progesterone, serotonin 5) Hematological -Blood volume expansion resulting in dilutional anemia -Hypercoagulable state due to increased circulating levels of clotting factors -Thromocytopenia -Benign leukocytosis (15-20,000) Drugs: Teratogenicity= the observation of any significant change in the function or form of a child secondary to prenatal treatment. Dependent upon the dose and gestational age at which it is administered. -Highest risk is during organogenesis 1st trimester. -FDA Classification for Use-in Pregnancy rating Category A: controlled studies show no risk. Adequate, well controlled studies in pregnant women have failed to demonstrate risk to the fetus. Category B: No evidence of risk in humans. Either animal findings show risk, but human findings do not; or, if no adequate human studies have been done, animal findings are negative Category C: Risk cannot be ruled out. Human studies are lacking, and animal studies are either positive for fetal risk or lacking as well. However, potential benefits may justify the potential risk. Category D: Positive evidence of risk to fetus. Nevertheless, potential benefits may outweigh the potential risk. Category X: Contraindicated in pregnancy. Fetal risk clearly outweighs any possible benefit to patient. Commonly used drugs in PACU: -Benzodiazapines: -Previously thought diazepam associated with development of craniofacial defects (cleft lip/palate). Further studies do NOT demonstrate an increased risk of congenital abnormalities. -Administering an anxiolytic (preop for example) may decrease catecholamine surges which can impair uteroplacental perfusion. Chronic benzo use may be deleterious. -Midazolam (Versed): D -Lorazapam (Ativan): D -Opiates: readily cross the placenta and can affect the fetus as seen with loss of beat to beat variability in the fetal hear rate and decreased fetal movement. Post op pain control is essential though as may increase risk of preterm labor. -Fentanyl: C -Morphine: C -Hydromorphone (Dilaudid): C -Meperidine (Demerol): C -Antihypertensives: -Commonly used: Labetalol (C), Hydralazine (C), Nifedipine (C), methyldopa (B). -ACE inhibitors such as enalapril (C/D/D) are teratogenic. -Magnesium used for pre-eclampsia/eclampsia to reduce risk of seizures. -GI -Ondansetron (Zofran): B -Droperidol: C -Metoclopromide (Reglan): B -H2 blockers such as ranitidine, famotidine: B -Promethazine (phenergan): C -Other human teratogens include: Coumadin, Isoretinoin, Lithium, Phenytoin, Thalidomide, Valproic Acid, Chemotherapy agents, Streptomycin, Tetracycline Some post-op considerations: -Good history/report including any complications with pregnancy (gestational diabetes, pregnancy induced hypertension). -OB consultation: for fetal monitoring intra/postop after 16 weeks for fetal HR monitoring and tocomonitoring after 24 weeks gestation (recommended up to 7 days postop) as postop analgesia may mask mild early contractions indicating preterm labor. -Positioning: Avoid supine or trendenlenberg positioning if possible. Left uterine displacement 15-30% after 20 weeks is essential. Place head of bed up to reduce decreased FRC and risk of aspiration. -Oxygen supplementation as needed. Avoid hypoxia. Fetus is dependent upon maternal PaO2. The combination of decreased FRC and increased oxygen consumption promotes very rapid desaturation during short periods of apnea. -Maintain normocarbia. There is a linear relationship between maternal and fetal PaCo2. Therefore, with hypercarbia there is a risk of fetal acidosis and fetal myocardial depression. Hypocarbia: alkalosis causes left shift in hemobglobin oxygenation curve which can compromise fetal oxygenation. -Avoid hypotension. Hypotension compromises uteroplacental perfusion. Causes of decreased uteroplacental perfusion: bleeding, hypovolemia, aortocaval compression, sympatectomy, uterine contractions, vasoconstrictors or other meds increasing uterine tone. Treat the cause: consider IV fluid/blood, left uterine displacement, Ephdrine/phenylephrine. -Pain: has been shown to increase risk of premature labor. Provide good postop analgesia. -DVT prophylaxis: Ted hose/SCDs, early mobilization, heparin